In the United States, around 10 million people are eligible for a type of lung cancer test called low-dose CT screening. This shows how common smoking-related health issues are. About 1.6 million of these are still smoking, with a smoking history of 20 to 29 pack years. They face a higher chance of getting lung cancer. Understanding “pack years” is important because it helps us know how much someone has smoked. This is linked directly to their risk of developing lung cancer. A “pack year” means how many packs of cigarettes someone smoked every day multiplied by how many years they smoked. Studies show those with at least 20 pack years of smoking have a high risk of lung cancer. This highlights how critical it is to get screened early and find ways to prevent this health problem.
Key Takeaways
- Understanding pack years helps assess lung cancer risk effectively.
- Nearly 10 million individuals are currently eligible for lung cancer screening in the U.S.
- Approximately 1.6 million current smokers have a 20 to 29 pack year smoking history.
- Those with higher pack years typically face increased lung cancer risk.
- Early detection through screening can significantly reduce mortality rates.
- Smoking cessation can lower lung cancer risks considerably over time.
Understanding Pack Years and Lung Cancer Risk
Pack years are key to knowing your lung cancer risk. Learning about Definition of Pack Years shows us how smoking affects our health. It touches on defining a pack year, calculating it, and why it matters when looking at smoking history.
Definition of Pack Years
A pack year measures how much a person has smoked. To find it, multiply the daily packs by smoking years. If you smoke one pack daily for 20 years, you have 20 pack years. This helps doctors understand a person’s smoke exposure and the risks to their health.
How to Calculate Pack Years
To calculate pack years, the formula is simple: (number of packs per day) x (years smoked) = pack years. If you smoke two packs daily for ten years, you’ve had 20 pack years. This calculation aids doctors. They can figure out the best screenings and how to prevent diseases.
Significance of Pack Years in Assessing Health Risks
Pack years are crucial for predicting lung cancer and related illnesses risks. Doctors warn that lung cancer risk grows with pack years. Studies show smoking causes around 85% of lung cancer cases. Knowing your pack years helps doctors decide if you need lung screenings. This is especially true for people with 20 or more pack years. This information is vital for stopping smoking and for health initiatives.
20 Pack Year Lung Cancer Risk
Lung cancer is the second most common cancer in the U.S. It’s a big health issue. Over 228,000 new cases happen every year. This shows us how smoking and lung cancer are linked. People who have smoked for 20 pack years are more likely to get lung cancer. This tells us a lot about smoking’s dangers.
Statistics on Lung Cancer Incidence
In 2020, about 228,820 people got diagnosed with lung cancer in the U.S. Sadly, around 135,720 died from it. Smoking causes 90% of these lung cancer cases. This fact shows how dangerous smoking is. Smokers are almost 20 times more at risk than non-smokers. The average age for finding out you have lung cancer is 70. The survival rate after 5 years is only 20.5%. But it’s higher if the cancer is caught early.
Comparison with High Pack Year Smokers
There are differences in risk between those who smoked a lot and those who smoked less. People who smoked 20-29 pack years have a different risk than those who smoked 30 or more. The risk is about 1.07 times higher for the 20-29 pack years group. This shows we need different guidelines for different people. The policy of screening smokers aged 50 to 80 years who smoked at least 20 pack years helps find those at the greatest risk.
Demographics and Lung Cancer
Studying lung cancer’s demographics helps us get vital insights. It shows how race and ethnicity affect lung cancer rates, revealing big differences. We also see how the disease impacts men and women differently.
Impact of Race and Ethnicity
Research shows racial and ethnic minorities usually have fewer pack years than non-Hispanic whites. Despite lower smoking rates, their lung cancer risk might be the same or even higher. This highlights the need to focus on race and ethnicity in health strategies and prevention.
Gender Differences in Lung Cancer Risk
Understanding gender differences is key in lung cancer research. Women tend to develop lung cancer after less exposure to smoking than men. This is due to biological reasons. Knowing these differences helps improve risk assessments and prevention methods.
| Group | Median Pack Years | Lung Cancer Risk |
|---|---|---|
| Non-Hispanic Whites | Higher | Higher risk |
| Racial and Ethnic Minorities | Lower | Similar or elevated risk |
| Women | Fewer than men | Higher susceptibility |
Impact of Quitting Smoking on Lung Cancer Risk
Quitting smoking is crucial in lowering the chance of getting lung cancer. The less you smoke, the better your chances over time. This is especially true for people who stop smoking early on.
Knowing how stopping smoking affects lung cancer risk matters a lot. It’s key for those who’ve used tobacco before.
Reduction in Risk Over Time
The good from quitting smoking shows up slowly. Within 10 to 15 years, people who stop can cut their risk by half or more.
This big improvement tells us why it’s so important to stop smoking soon. It encourages people to think about quitting.
Importance of Time Since Quitting
How long it’s been since you quit matters a lot. Even after 15 years, there’s still a risk for lung cancer in ex-smokers.
That’s why they need to keep an eye on their health. They should get regular check-ups, especially if they smoked a lot before. For more info, go to this lung cancer advice page.

| Years Since Quitting | Risk of Lung Cancer Compared to Current Smokers |
|---|---|
| Less than 5 | HR = 12.12 |
| 5 – 9 | HR = 11.77 |
| 10 – 14 | HR = 7.81 |
| 15 – 24 | HR = 5.88 |
| 25 and more | HR = 3.85 |
Lung Cancer Screening Guidelines
Being ahead of your health can really help catch lung cancer early. The new Lung Cancer Screening Guidelines show us how to spot people who may be at risk sooner. This could mean a big difference in getting the right help early.
Who Should Get Screened?
Now, people between 50 and 80 who’ve smoked a lot over the years should get checked every year. This is for those who smoke now or stopped in the last 15 years. Thanks to these updates, about 5 million more folks are eligible for screening.
Before, the advice was aimed at those 55 to 74. This is a big change in who should get checked for lung cancer.
Low-Dose CT Scan as a Screening Tool
A Low-Dose CT Scan picks up lung cancer better early on than old-school chest X-rays. It’s really good at finding cancer when it’s easier to treat. But, like all tests, it has its downsides, like false alarms.
Talking about quitting smoking regularly is key. It highlights how important it is for patients and doctors to make decisions together.
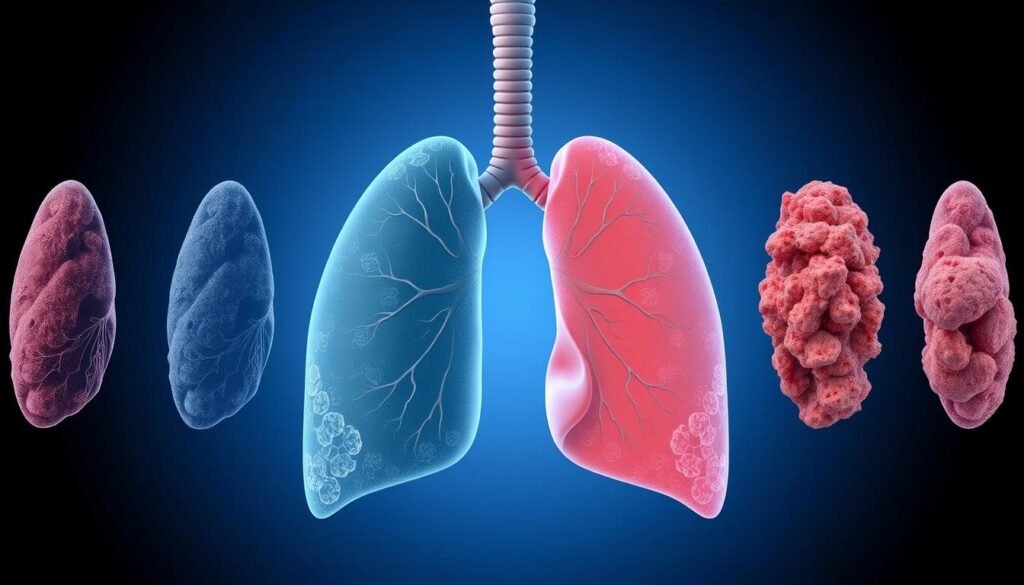
Understanding Lung Cancer Stages
To fully grasp lung cancer, knowing the stages is key. It’s crucial for deciding on treatment and predicting the outcome. Understanding the stage helps doctors create a personalized treatment plan.
How Stage Affects Treatment Options
Staging is vital in choosing the right lung cancer treatment. For early stages, surgery might remove the tumor completely. Treatments vary, especially when lung cancer hasn’t spread too far.
Options for treatment include:
- Radiofrequency ablation: This is for tumors on the lungs’ edge.
- Chemotherapy: Uses IV drugs to kill cancer cells.
- Targeted drug therapy: Attacks specific cancer cell mutations.
- Immunotherapy: Helps the immune system fight cancer.
- Radiation therapy: Works for managing lung cancers, alone or with surgery.
These treatments can cause side effects like nausea and fatigue. Patients need good care to manage these.
Prognosis and Survival Rates
Survival chances depend a lot on the cancer stage when found. Early detection means better odds. Small tumors, for instance, often mean higher survival rates than widespread cancer.
Stages are key for predicting survival and choosing treatments. Look at these stats:
| Stage | 5-Year Survival Rate | Treatment Options |
|---|---|---|
| Stage I | Up to 92% | Surgery, targeted therapy |
| Stage II | Up to 70% | Surgery, chemotherapy |
| Stage III | Up to 38% | Chemotherapy, radiation, surgery |
| Stage IV | Up to 7% | Palliative care, chemotherapy |
Knowing lung cancer stages illuminates treatment choices and gives a sense of what to expect. This is key for patients and their families in navigating lung cancer treatment.
Risks Beyond Smoking: Additional Factors for Lung Cancer
Cigarette smoking is a top cause of lung cancer. But, we also need to look at secondhand smoke and environmental risks. Things like radon exposure matter too. It’s crucial to understand these to fight lung cancer better.
Secondhand Smoke Exposure
Being around secondhand smoke is bad, especially for non-smokers. Breathing in smoke from others’ cigarettes can make you more likely to get lung cancer. So, it’s important to reduce this exposure. Doing so helps everyone and makes the air healthier.
Radon Exposure and Other Environmental Risks
Radon exposure is a big environmental risk for lung cancer. This gas comes from the natural breakdown of soil and rock. Being around radon a lot can lead to lung cancer. Also, working around dangerous chemicals can make lung cancer more likely. We must know about these risks and try to avoid them.
It’s vital to tackle issues like secondhand smoke and radon. Adding preventive steps can help lower lung cancer rates. Education on these dangers can make a big difference, too.
Understanding Cancer Risk Assessment
Cancer risk assessment helps figure out someone’s chance of getting lung cancer. It looks at things like Medical History and Family History. Knowing this info helps doctors suggest the best screening and prevention plans.
The Role of Medical History
Looking at medical history helps doctors understand someone’s lung cancer risk. Things like past lung diseases, smoking, and being around cancer-causing stuff are key. People need to give doctors full details of their health past for accurate risk checks.
Evaluating Family History and Genetic Factors
Family history is a big clue in figuring out lung cancer risk. If relatives had lung cancer, your own risk might go up. Genes can also play a role, suggesting the need for gene testing. Talking about Family History with doctors helps choose the right screening tests. Tools like the University of Maryland’s lung health tool can show your risk by looking at these key points.
Effective Tobacco Cessation Strategies
Quitting smoking lowers the risk of lung cancer greatly. It makes effective Tobacco Cessation Strategies vital for health improvement. There are many Quitting Resources focused on education and support. They help those wanting to stop smoking.
Resources for Quitting Smoking
Many organizations offer help to those wanting to quit smoking. The CDC has comprehensive guides, tips, and hotline services. These resources help smokers see the quitting benefits. They also provide tools for success.
Support Programs and Counseling
Support programs and counseling boost quitting success. There are group meetings, counseling sessions, and online forums. These Support Programs give the needed encouragement. They offer resources for individuals to stick to their goals, leading to healthier lives.
| Type of Support | Description |
|---|---|
| Hotlines | 24/7 support for immediate assistance. |
| Online Programs | Interactive courses and resources for quitting. |
| In-person Counseling | Guided sessions with professionals for personalized support. |
| Group Support | Meetings with others facing similar challenges. |
Conclusion
Knowing about the 20 pack year risk for lung cancer is key. It helps us find better ways to prevent this illness. The numbers show regular health checks and knowing your risk factors really matter.
Whether you smoke a lot or a little, your health in the future is at stake. Even people who don’t smoke much can still get lung cancer. This tells us how important it is to keep an eye on our health.
The risk of getting lung cancer varies for people from different backgrounds. This means that prevention plans need to be specific for each group. Right now, we are not doing enough to screen everyone who is at high risk.
By knowing more about the risks and getting checked often, we can fight lung cancer better. This could mean saving many lives and years of health for lots of people. Everyone — people, doctors, and the government — needs to work together to take on lung cancer.