Did you know small cell lung cancer (SCLC) makes up 15% of lung cancer cases in the US? This fast-moving cancer needs quick diagnosis for the best treatment. Many patients find out they have it through chest X-rays that show something’s not right. This leads to more tests.
To battle this disease, knowing about diagnostic tests is key. Imaging, biopsies, and lab tests are important to confirm SCLC and see how far it’s spread. Diagnostic tests help doctors create a personalized treatment plan. This can really improve how well patients do.
Key Takeaways
- Early diagnosis can significantly improve treatment outcomes for small cell lung cancer patients.
- Various imaging techniques such as CT scans and MRIs are crucial in determining cancer presence and spread.
- Biopsy methods, including fine needle aspiration and bronchoscopy, help accurately identify cancer types.
- Understanding staging (limited vs. extensive) is essential for establishing treatment plans.
- A multidisciplinary team approach ensures comprehensive care and treatment options.
- Low-dose diagnostic scans minimize radiation exposure while maintaining image quality.
Understanding Small Cell Lung Cancer
Small cell lung cancer (SCLC), or 30% of all lung cancers, grows fast and spreads early. It’s mostly known as small cell carcinoma. There’s also a rare form called combined small cell carcinoma.
Smoking tobacco is the biggest risk for SCLC. Other risks include secondhand smoke, asbestos, and certain workplace chemicals. Getting older also increases cancer risk. Together, smoking and these factors make lung cancer more likely.
Knowing how SCLC works is key to finding good treatments. Diagnosis and staging tests, like chest x-rays and CT scans, help catch it early. Catching it early improves chances for successful treatment.
The survival rate for SCLC is low, only about 7% after five years. This fact highlights the need for early detection. People with lung cancer should talk about how stopping smoking could help their health.
For more on small cell lung cancer, check helpful resources. The American Cancer Society offers a complete guide. Also, visit Care Your Lungs for info on diagnosis and management.
Symptoms of Small Cell Lung Cancer
Small cell lung cancer quickly gets people’s attention because of how fast it progresses. A persistent cough and chest pain are common signs. These symptoms are serious and suggest something might be wrong.
Patients often feel extremely tired and have trouble breathing. This makes even simple tasks hard to do. Wheezing and getting infections over and over again are other signs. These problems show the cancer is affecting the lungs.
Most patients, around 70%, find out they have widespread disease when they’re first diagnosed. So, knowing these signs early on is key. It can help catch the cancer sooner rather than later.
About 75% of people with SCLC are in the hospital within three months after finding out they have it. This fact highlights why it’s so important to watch for these symptoms. If you know what to look for, you can get help sooner. This might make things better for those dealing with this tough type of cancer.
| Small Cell Lung Cancer Symptoms | Frequency |
|---|---|
| Persistent cough | Common |
| Chest pain | Common |
| Weight loss | Frequent |
| Shortness of breath | Frequent |
| Wheezing | Occasional |
| Recurrent respiratory infections | Occasional |
Importance of Early Diagnosis
Finding lung cancer early is key to effective treatment and living longer. When small cell lung cancer (SCLC) is caught early, patients have more treatment options. This significantly improves their chances. For example, early-stage lung cancer patients have a 5-year survival rate over 90%. But it drops below 10% for advanced stages. This shows how crucial early detection of SCLC is.
Sometimes, lung cancer starts with hard-to-notice signs. It’s important to know these, especially for those at high risk. Signs like a continuous cough, losing weight without trying, or getting sick often can be clues. Seeing these signs early can mean faster testing and advice from doctors.
Screening with low-dose CT (LDCT) scans is now seen as better than regular chest x-rays. Research says it can cut death rates by 20% compared to older methods. Yet, LDCT scans aren’t perfect and can show a 23.3% false positive rate. This fact points out why we need to keep improving how we find SCLC early.
Health groups now suggest yearly LDCT scans for people 50-80 years old with a smoking history. Accepting these scans can help catch lung cancer soon. This early step is crucial for getting on the right treatment path early, which can save lives.
| Stage | 5-Year Survival Rate |
|---|---|
| Stage IA | Exceeds 90% |
| Stage IV | Less than 10% |
Initial Steps in Diagnosis
Diagnosing small cell lung cancer (SCLC) starts with looking at the patient’s medical history and a physical check-up. Health experts consider many things, including symptoms and risk factors, like if the person smokes. This helps doctors get important information for the next steps in diagnosis.
Medical History and Physical Exam
Doctors make sure to get a complete medical history and do a full physical exam. They look for signs of lung cancer and check the patient’s overall health. They might ask about:
- How long and how severe symptoms have been.
- If cancer runs in the family.
- How much and how long the person has smoked.
- If they’ve been around harmful stuff like asbestos.
Chest X-ray and Initial Imaging
The first step in imaging is usually a chest X-ray. This helps doctors see if there are any lung problems that need a closer look. If something looks off, they might do more tests, like CT scans or MRIs, to learn more about the disease.
Diagnostic Tests for Small Cell Lung Cancer
Small cell lung cancer (SCLC) can be tough to diagnose right away. It’s very important to have effective tests for SCLC. These tests help doctors create the best treatment plans. They use different tests to learn about the disease’s presence and how far it has spread.
Overview of Tests Used for Diagnosis
Doctors have various tests to confirm if someone has small cell lung cancer. They also use these tests to figure out the cancer stage. Some key methods used for checking SCLC are:
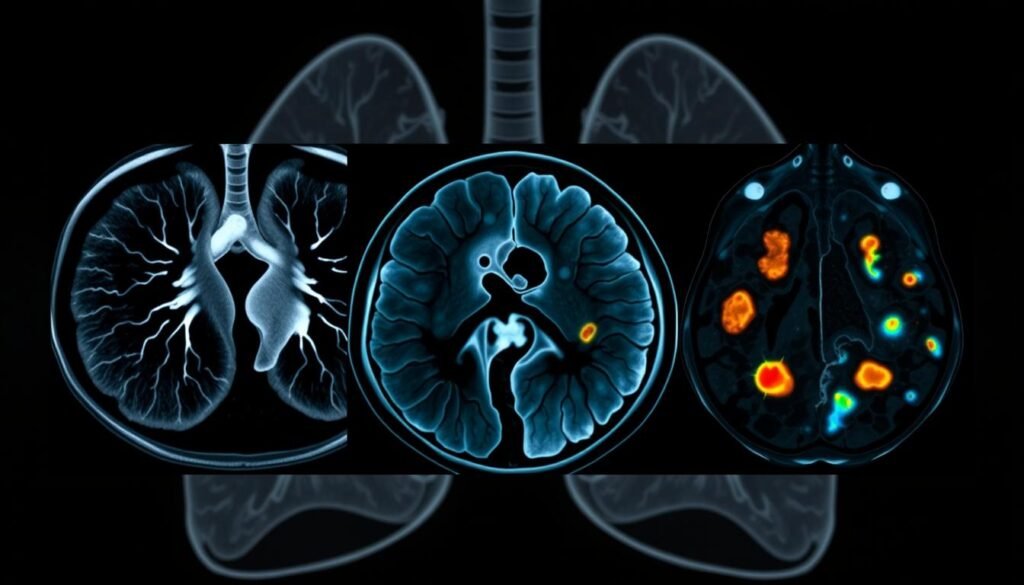
- Imaging Studies: These are things like CT scans, MRIs, and PET scans. They help find tumors, see their size, and if cancer has spread.
- Lung Biopsy: This is when doctors take a small sample of lung tissue. This can be done in different ways. A lung biopsy clearly tells if it’s cancer and helps in choosing treatments.
- Comprehensive Biomarker Testing: This test looks for specific genes related to SCLC. Finding these genes can help give a treatment that fits the patient’s specific cancer.
Each test is important for understanding the disease completely. With a full picture, doctors can quickly start the right treatment. This approach greatly improves the chances for patients with SCLC.
| Test Type | Description | Purpose |
|---|---|---|
| Imaging Studies | CT scans, MRIs, PET scans | To visualize and assess tumors and metastasis |
| Lung Biopsy | Tissue sampling methods | To confirm cancer type and enable treatment planning |
| Biomarker Testing | Genetic analysis of the tumor | To identify treatment-specific genetic mutations |
Imaging Techniques in Lung Cancer Diagnosis
Imaging methods are key for pinpointing lung cancer, especially small cell lung cancer (SCLC). Various techniques unveil vital details on tumors and how far they’ve spread. This info is crucial for crafting effective treatments. Knowing the role of each imaging method aids doctors and improves patient care.
CT Scans: Detailed Imaging of the Lungs
CT scans stand out in diagnosing SCLC. They provide in-depth pictures of the lungs. These images help spot tumors and check lymph nodes. The clarity of CT scans is vital for assessing the disease’s reach and planning treatment.
MRIs: Checking for Tumor Spread
MRI is essential for spotting cancer spread, especially to the brain and soft tissues. Brain MRIs with contrast detect brain metastasis in a significant number of SCLC patients without neurological signs. Thus, MRIs are critical for thorough assessment.
PET Scans: Understanding Metastasis
PET scans go beyond detection. They show areas of high metabolic activity, likely indicating cancer spread. This technique gives doctors clear insight into the disease’s stage, helping tune treatments.
Nuclear Imaging: Bone Scans and Their Relevance
Nuclear imaging, like bone scans, is crucial for spotting bone metastasis in SCLC patients. Technetium-99m bone scintigraphy is used when FDG-PET or PET/CT scans aren’t an option. Understanding where and how bone metastasis occurs supports better treatment decisions and disease tracking.
| Imaging Technique | Primary Use | Key Benefits |
|---|---|---|
| CT Scans | Detailed imaging of the lungs | Assesses tumor growth and lymph node involvement |
| MRIs | Metastasis evaluation | Detects lesions in brain and soft tissues |
| PET Scans | Metabolic activity tracking | Identifies cancer spread effectively |
| Nuclear Imaging | Bone metastasis detection | Evaluates metastasis patterns, helpful in treatment |
Biopsy Methods for Accurate Diagnosis
Diagnosing small cell lung cancer depends on effective tissue sampling. There are various biopsy methods available, each with its own benefits. Knowing about these methods is key for accurate diagnosis and treatment planning.
Fine Needle Aspiration (FNA) Biopsy
An FNA biopsy uses a thin needle to get a tissue sample. It is often guided by imaging for precise targeting. This method is less invasive, which is great for initial testing, especially in high-risk patients.
Core Needle Biopsy
A core needle biopsy is used when more tissue is needed. It extracts a cylinder of tissue with a larger needle. This helps doctors make a clear diagnosis, distinguishing between lung cancer types.
Bronchoscopy: A Closer Look
Bronchoscopy inserts a thin tube with a camera into the lungs. It lets doctors see the lungs directly and take samples. The success varies with the lesion’s size, better for big central lesions.
Endobronchial Ultrasound: Enhanced Biopsy Accuracy
Endobronchial ultrasound (EBUS) uses ultrasound with bronchoscopy for better imaging. It helps sample lymph nodes and structures near the lungs. EBUS improves sampling accuracy, especially in difficult-to-reach areas.
| Biopsy Method | Tissue Sample Size | Diagnostic Yield |
|---|---|---|
| Fine Needle Aspiration (FNA) | Small Sample | Moderate |
| Core Needle Biopsy | Large Sample | High |
| Bronchoscopy | Variable Sample | 88% for large lesions, 14% for small lesions |
| Endobronchial Ultrasound (EBUS) | Variable Sample | High Accuracy (96% success) |
Thoracentesis: Fluid Analysis for Diagnosis
Thoracentesis is a key method for figuring out problems related to fluid around the lungs. It’s a simple procedure that lets doctors take fluid for tests. This helps them learn more about the patient’s health. Analyzing this fluid helps identify reasons behind it, like lung cancer.
When doing thoracentesis, doctors use a needle to get fluid from around the lungs. This method is quick and lets them examine the fluid closely. The test shows if the fluid is due to changes in blood vessels or inflammation. Knowing this helps pinpoint the problem.
In cases of lung cancer, checking the fluid is very important. At Christchurch Hospital in New Zealand, the accuracy of these tests for lung cancer was about 79.0%. It’s a vital step to catch cancer cells early for better treatment options.
The look of the fluid can tell doctors a lot. For example, if it’s cloudy, the test is more likely to be right. The fluid’s color and thickness seen in scans also matter a lot. These details help doctors make better choices for their patients.
Analyzing the fluid helps doctors predict how a disease might change and respond to treatment. Knowing the fluid type helps in planning the best care for the patient.

Overall, thoracentesis is crucial for decoding problems with fluid around the lungs, especially for lung cancer. It gives doctors important information for choosing the best way to treat patients.
Utility of Sputum Cytology in Lung Cancer
The sputum cytology test is key for lung cancer screening. It checks mucus from the lungs to find cancer cells. It’s really good at spotting tumors in the big airways. This method helps identify lung cancer cells.
Collecting sputum samples in the morning over several days improves accuracy. The method’s sensitivity in finding lung cancer varies. It’s about 65% on average but can range from 22% to 98%. This depends on how many samples are taken. Compared to X-ray screenings, this method is better at catching tumors early.
One study found cancer cells in the sputum of 11 out of 39 cases. This shows how useful the test is for diagnosing certain types of lung cancer. Even when no cancer cells are found, the test is still important. It helps decide if more tests are needed when lung cancer is suspected.
The sputum cytology test is a non-invasive way to check lung health. It also sets the stage for more tests if needed. It’s crucial for finding lung cancer early. As our knowledge gets better, this test might become even more reliable.
| Parameter | Value |
|---|---|
| Average Sensitivity | 65% (Range: 22–98%) |
| Malignant Cells Detected | 11 out of 39 cases |
| Higher Detection Rate | Compared to X-ray screening |
The Role of Tumor Markers in Diagnosis
Tumor markers are essential in the cancer diagnosis process. They help find diseases like small cell lung cancer (SCLC). These markers might be things cancer cells release or that show up in the body when cancer is there. For SCLC, some markers give important info on diagnosis, outlook, and how well treatments work.
Key SCLC markers include Chromogranin A (CgA), pro-gastrin releasing peptide (ProGRP), and neuron-specific enolase (NSE). Chromogranin A can tell if someone has SCLC with 61% accuracy. ProGRP is really good at telling SCLC apart from non-small cell lung cancer (NSCLC). And NSE helps find both SCLC and neuroblastoma.
There have been big steps forward in understanding these markers. For example, tests of plasma DNA show lung cancer patients have more free-circulating DNA than healthy people. Looking at plasma DNA in SCLC, scientists found a 71% sensitivity using markers like ACTBP2, UT762, and AR. Also, new SCLC-specific monoclonal antibodies (MoAbs) are being made for better diagnosis accuracy.
Tumor markers are not just for starting treatment; they also track how well treatments are working. Doctors use them for ongoing checks through blood tests or looking at cells. Even though they’re helpful, tumor markers aren’t perfect. They’re often used with other tests.
Researchers are always finding new tumor markers. This helps with more accurate diagnosis of SCLC. Knowing more about SCLC and its markers helps doctors care for patients better. This leads to improved treatment approaches.

Staging Small Cell Lung Cancer
Understanding how far small cell lung cancer (SCLC) has spread is important. There are two main stages: limited and extensive. Limited-stage SCLC means the cancer is only in one lung and nearby lymph nodes. When it’s extensive-stage, the cancer has spread to other parts of the body, making treatment more complex.
The Veterans’ Administration Lung Study Group (VALSG) was the go-to for staging for years. But now, more doctors are using the TNM classification for better accuracy. Using staging SCLC, tools like PET scans help a lot. They make staging more accurate and help plan treatments by showing cancer spread.
Treatment changes a lot based on the stage of the small cell carcinoma. Early-stage patients, like 20-25% of those at limited stage, may find cure with chemo and radiotherapy. But those found at later stages, like 3 or 4, have less options and often a tougher outlook.
Staging helps doctors find the best treatments for each patient. The right staging leads to better treatment choices. This helps doctors and patients understand cancer better. For more on SCLC staging, check here.
| Stage | Definition | Treatment Options |
|---|---|---|
| Limited Stage | Cancer confined to one lung and its adjacent lymph nodes | Chemotherapy + Radiotherapy |
| Extensive Stage | Cancer has spread beyond the lung and nearby lymph nodes | Palliative Care, Chemotherapy |
Conclusion
The way we diagnose SCLC is key to better understanding and treating small cell lung cancer. Using different tests helps catch it early which makes treatment more effective. SCLC makes up about 15% of all lung cancer cases. So, testing for lung cancer is very important. Catching it early can lead to higher survival rates.
The five-year survival rate for SCLC is only 10%. This shows how vital these diagnostic strategies are for helping patients.
With new tech, there’s hope for lung cancer diagnosis improvement. New methods could make diagnosis faster and more accurate. This can lead to quick treatments that could change a patient’s outcome. New treatments and markers are promising for fighting this tough disease. They could help many people with SCLC.
To manage small cell lung cancer well, we need to use these diagnostic tools. Early and accurate diagnosis is a big step. It helps healthcare workers help their patients live longer and better lives despite this aggressive cancer.