In the United States, only about 18.8% of lung cancer patients live past five years, as noted in 2017 data. This highlights how crucial early detection and managing lung health are. Spirometry plays a key role here, especially since 84% of lung cancer cases are non-small cell lung cancer (NSCLC). These tests give crucial details on lung function, helping doctors spot issues like COPD.
Doctors use various lung function tests to gauge how well your lungs work. They use this information to make choices about your diagnosis and care. We will look closer at how spirometry tests are important for folks with lung cancer. These tests’ results are key for deciding how to manage and treat patients.
Key Takeaways
- Lung cancer accounts for 84% of diagnosed cases, with NSCLC being the most prevalent type.
- Lung cancer survival rates highlight the need for effective early detection methods.
- Spirometry tests play a crucial role in evaluating pulmonary function and airflow capacity.
- Abnormal spirometry results are linked to poorer overall survival in lung cancer patients.
- Understanding spirometry measurements helps differentiate between obstructive and restrictive lung diseases.
- Effective patient management relies heavily on accurate spirometry results prior to lung cancer treatment.
Understanding Spirometry and Its Importance in Lung Cancer
Spirometry is key for testing lung function, allowing accurate measurements of air flow. It’s crucial for diagnosing pulmonary diseases, especially lung cancer. Through spirometry, doctors can spot changes in lung function early. This leads to better treatment choices for lung cancer patients.
The cost of a spirometry test is about $60 for those paying without insurance. This test gives important numbers like Forced Vital Capacity (FVC) and Forced Expiratory Volume (FEV-1). FVC shows the quantity of air you can breathe in and out. FEV-1 measures how much air you can blow out in one second. A normal FEV-1 and FVC score is within 80% to 120% of expected values, considering factors like age, sex, and height.
These test results help doctors figure out if someone has lung problems like asthma, COPD, cystic fibrosis, or pulmonary fibrosis. If spirometry results are off, it might mean lung issues that need medicine or other treatments. Spirometry is also vital in checking if treatments for chronic lung problems are working well.
Spirometry is part of broader pulmonary function tests (PFTs). Besides spirometry, PFTs include lung volume and diffusion capacity tests. Lung volume tests measure the total air your lungs can hold. Diffusion capacity tests see how well oxygen gets into your blood.
In conclusion, spirometry is incredibly important. Having regular tests can track lung function changes and help adjust treatments, improving care for patients. For more on spirometry in respiratory disease diagnosis, check out this resource.
What Is a Spirometry Test?
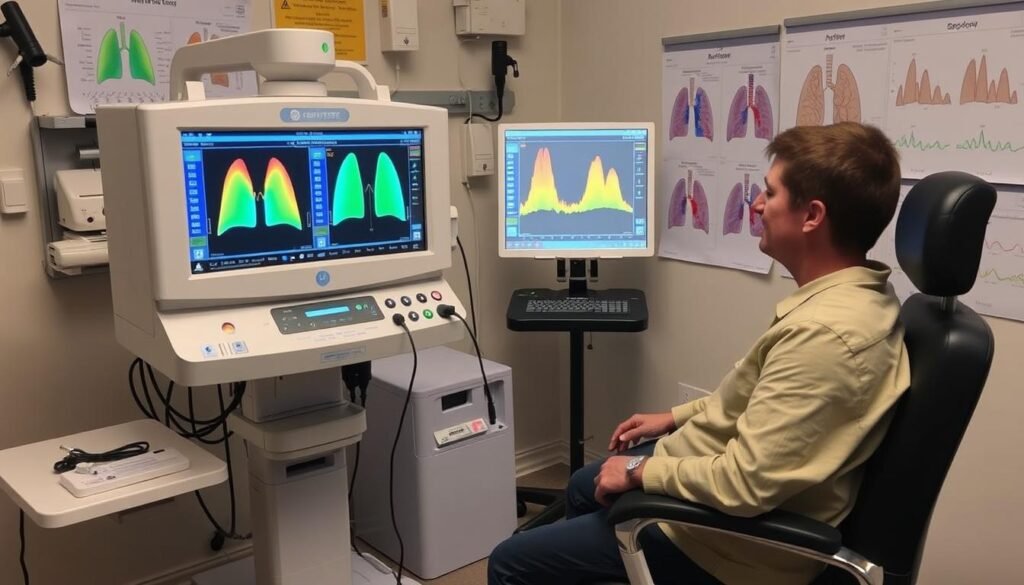
A spirometry test is often done to check lung health. It’s a key pulmonary function test. It measures how much and how fast you can breathe out. This test uses a spirometer to get accurate airflow readings.
When taking the test, you’ll breathe in deeply then blow out hard into the spirometer. This checks for lung problems like asthma, COPD, and pulmonary fibrosis. It’s a safe, easy test that doesn’t hurt.
It’s important to do spirometry tests regularly to watch for lung changes. Before testing, avoid smoking for 24 hours for the best results. The test is quick, taking only 15 to 30 minutes.
The results are compared to normal values based on sex, age, and height. This shows if there’s an issue, like obstructive or restrictive lung disease. Knowing this helps doctors make the right treatment plan.
| Key Components | Description |
|---|---|
| Test Duration | 15-30 minutes |
| Preparation | Avoid smoking for at least 24 hours prior |
| Pain Level | Noninvasive and painless |
| Main Purpose | Measure airflow, identify lung diseases |
| Common Conditions Assessed | Asthma, COPD, pulmonary fibrosis |
How Lung Cancer Spirometry Results Help Diagnose Pulmonary Diseases
Lung cancer spirometry results are key in diagnosing different lung diseases. They show if a lung disease is obstructive or restrictive. By looking at airflow and how much air the lungs can hold, doctors can figure out how healthy a patient’s lungs are. This leads to better treatment plans.
Role in Identifying Obstructive and Restrictive Lung Diseases
Spirometry is crucial for telling obstructive and restrictive lung diseases apart. An obstructive lung disease, indicated by a low FEV1/FVC ratio, means the airways are narrowed. On the other hand, reduced FVC points to restrictive lung disease, meaning the lungs can’t fully expand. Knowing these differences helps diagnose lung diseases accurately and decide on the right treatment.
Associations with Chronic Obstructive Pulmonary Disease (COPD)
Many lung cancer patients also have COPD. Studies show that 50% to 80% of people with lung cancer have COPD. Spirometry results can show these patients might have worse health outcomes because they have both conditions. So, recognizing COPD in cancer care is very important. It can make treatments better and help patients live better lives.
Other Respiratory Conditions Evaluated through Spirometry
Spirometry also helps diagnose conditions like asthma, bronchitis, and emphysema. It provides important info on lung function. This helps doctors make decisions about surgery risks, treatments, and keeping an eye on lung health. Understanding spirometry results is key in managing shortness of breath and other lung issues. This means better patient care.
| Condition | Spirometry Findings | Characteristics |
|---|---|---|
| Obstructive Lung Disease | Reduced FEV1/FVC Ratio | Difficulty exhaling air, common in COPD |
| Restrictive Lung Disease | Reduced FVC | Limited lung expansion, often due to lung stiffness |
| Asthma | Variable airflow obstruction | Wheezing, shortness of breath, and chest tightness |
| Chronic Bronchitis | Reduced FEV1 with normal FVC | Frequent cough and sputum production |
| Emphysema | Low FEV1/FVC ratio | Destruction of alveoli leading to air trapping |
For more info on spirometry, check out this resource. Understanding spirometry’s importance in diagnosing and treating lung diseases is crucial. It’s especially true given the complex link between different lung conditions and lung cancer.
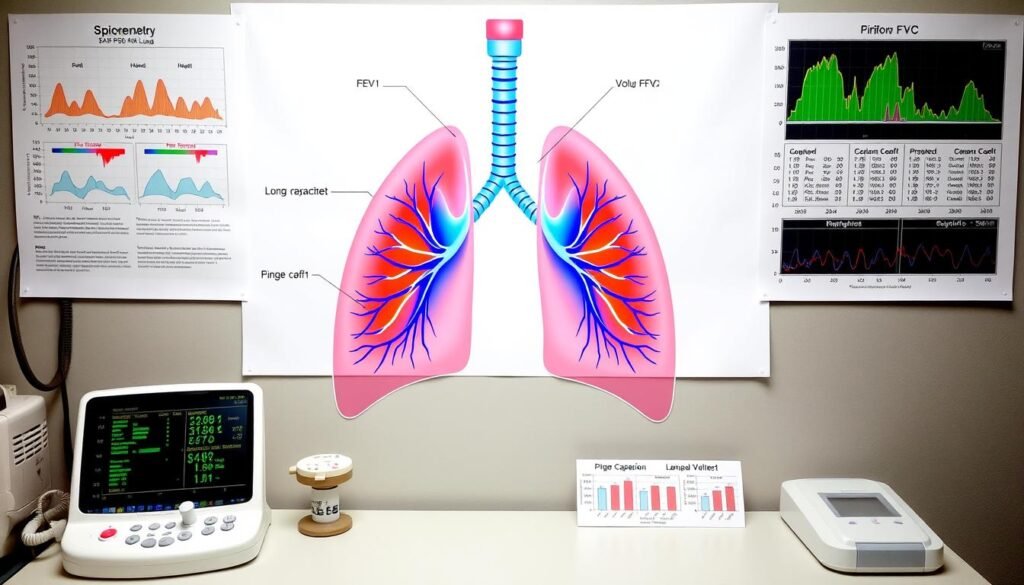
Key Measurements in Spirometry: FEV1 and FVC
Spirometry is key for understanding lung function with two main measurements: FEV1 and FVC. These help diagnose lung diseases and create personalized treatments. They are vital for medical professionals.
Forced Expiratory Volume in 1 Second (FEV1)
FEV1 tells us how much air you can forcefully exhale in one second. It’s vital for spotting airway obstruction from conditions like asthma or COPD. When FEV1 is low, it might mean the lungs are not working well.
Regular lung function tests show how well treatments are working. They help keep airways open.
Forced Vital Capacity (FVC)
FVC measures the total air exhaled after taking a deep breath. It indicates the size of the lungs. This is crucial for telling apart obstructive from restrictive lung diseases.
In people with lung issues, a low FVC suggests a problem that needs more tests. Visit this site for more details.
Understanding the FEV1/FVC Ratio
The FEV1/FVC ratio is important for checking lung health. A ratio under 70% often signals obstructive lung disease, per GOLD guidelines. The ATS uses specific standards for more accuracy.
This ratio helps doctors figure out the problem and plan treatments. It aims to better the lives of patients.
| Measurement | Significance | Normal Values | Implications of Abnormal Values |
|---|---|---|---|
| FEV1 | Indicates airway obstruction | Depends on age, gender, and height | Possible airway blockage or weak lungs |
| FVC | Shows lung size | Varies by age, gender, and height | Could mean restrictive lung disease |
| FEV1/FVC Ratio | Tells obstructive vs. restrictive diseases apart | Usually over 70% | Below 70% points to obstructive issues |
Keeping tabs on FEV1 and FVC is crucial for doctors. It helps them see changes and adjust care. Timely care based on these numbers is key for patient health.
What Lung Cancer Spirometry Results Tell You
Understanding lung cancer spirometry results is key for checking a patient’s lung health. When results are not normal, they show there’s a problem that needs attention. They help us see how well a person’s lungs work.
Interpreting Abnormal Results
Abnormal spirometry results often point to lung diseases like COPD or asthma. They can also highlight restrictive conditions tied to obesity or other issues. The FEV1/FVC ratio is especially crucial as it measures airway obstruction.
Normally, young adults have a ratio above 85%. This number gets lower with age, dropping to 70% or lower after 60 years.
Implications for Overall Survival in Lung Cancer Patients
Studies link lung function, shown by spirometry, to survival rates in lung cancer patients. Those with low FEV1 or FVC numbers are at a greater risk of dying. This is why it’s important for doctors to keep an eye on these results.
Adjusting treatments based on these measures can help patients live longer. Doctors also use these results with other tests, like physical exams and imaging, to make a full treatment plan.
Preparing for a Spirometry Test
Getting ready for a spirometry test properly ensures the results about your lungs are correct. It’s crucial for patients to follow specific steps before the test. This helps doctors get the info they need, especially for checking lung health.
Pre-Test Considerations for Accurate Results
There are several important things to do before your spirometry test. These help make sure the test results are accurate. What to remember includes:
- Wear clothes that are loose and comfy to not interfere with the test.
- Don’t do hard exercises on the test day, so your lungs are rested.
- Stay away from smoking and asthma medicine for at least four hours before your test.
- Avoid big meals to keep from feeling uncomfortable during the test.
This preparation helps ensure the spirometry test goes smoothly. It also helps in finding any lung problems early.
What Happens During the Spirometry Procedure?
During the spirometry test, you’ll breathe into a special device. This helps measure how well your lungs are working. The most important parts of the test include:
- Making sure your lips tightly seal the mouthpiece to avoid air leakage.
- Using a nose clip to make you breathe through your mouth only.
- Doing the test a few times for accurate and consistent results.
The whole test usually takes about 15 minutes. Listening to the test instructions is key to getting good results.
Understanding why these lung tests matter can help find lung problems early. Being thorough in your test preparation and following through can boost your health.
For deeper insights into lung health and catching lung cancer early, please visit early detection strategies for lung cancer.
Post-Test: Understanding Your Results
After you take a spirometry test, understanding the results is key. It tells you how well your lungs work. The results are measured against normal values for your age, height, and sex. This helps you know the health of your respiratory system.
Evaluating Airflow Measurement and Lung Function
The spirometry test looks at airflow measurements like FEV1 and FVC. A normal ratio is between 70% and 85%. If your results are lower, it might mean there’s a problem with your lungs. Understanding these numbers helps you talk to your doctor about what they mean.
The Importance of Percent Predicted Values
Percent predicted values compare your results to what’s expected for someone healthy. For example, a low FEV1 might mean a serious lung issue. It shows why regular checks are important. They can catch diseases like COPD early. Knowing these values helps you make better health choices.
Using Spirometry Results to Inform Treatment Decisions
Healthcare providers rely more on spirometry results for lung cancer patients. The test data helps pick the right treatment, matching it to how well the lungs work. The spirometry measures, like Forced Expiratory Volume in one second (FEV1) and forced vital capacity (FVC), are key for personalized care.
Determining Treatment Options Based on Lung Function
Spirometry data helps doctors understand how bad a lung problem is. This allows them to find the best treatment. For example, someone with low FEV1 might get better with certain medications.
Also, knowing if a patient has COPD and how severe it is during lung cancer checks affects treatment choices. This could mean changing medicines or even considering surgery. Treatment options can include:
- Bronchodilators for obstructive patterns
- Corticosteroids to reduce inflammation
- Personalized exercise programs to improve lung capacity
- Surgical interventions based on lung function assessment
Monitoring Progress through Follow-up Spirometry
Regular spirometry check-ups are key in watching lung health over time. These follow-up tests help doctors see if treatments are working by comparing current results to the initial ones. They can then decide if a patient’s lung function is getting better, staying the same, or getting worse. This helps adjust treatment plans as needed.
Patients should plan for:
- Scheduled follow-up spirometry tests to check lung function
- Regular checks on symptoms and how well treatment is working
- Changes to treatment based on how they’re doing
- Learning more about how to keep their lungs healthy
Adding spirometry to regular care helps make sure treatments are working well. It’s key in creating a care plan that’s made just for each patient. Focusing on lung health leads to better care for people with lung cancer.
Conclusion
Spirometry is key in managing respiratory health. It gives valuable data on lung function. This helps doctors spot different lung problems.
Those with obstructed lung function face a higher lung cancer risk. Low FEV1 and FVC scores are a big warning sign. This shows how crucial spirometry is for early cancer detection.
Keeping an eye on spirometry results helps doctors make better treatment choices. Studies show people with airflow issues have a higher lung cancer risk. Regular checks are therefore vital.
By adding spirometry to other screening methods, health outcomes can improve. It helps uncover hidden or mistaken diagnoses, offering a clearer view of a patient’s health.
Spirometry’s insights don’t just help with current treatments. They also support long-term survival for lung cancer patients. As more learn about spirometry, we can boost lung health care. This means better life chances for those fighting lung cancer.