Did you know that video-assisted thoracoscopic surgery (VATS) has been around for over 20 years? This shows how effective and mature the method is, especially for lung cancer surgery. It’s important for both surgeons and patients to know about lobectomy. This helps them understand how it affects their results. We’ll look into different surgical methods, focusing on the differences between open surgery and minimally invasive surgery.
Lobectomy removes a lung lobe and is mainly done for lung cancer or some benign lung diseases. The move towards VATS brought big benefits. These include less pain after surgery, quicker recovery, and fewer problems than with traditional open surgery. Studies also show that patients do better when they have the minimally invasive option.
Minimally invasive surgery is becoming more popular because it’s better for patients and still treats the problem effectively. Next, we’ll go deeper into how both open lobectomy and VATS work. We want to give you the information you need to make smart decisions about lung cancer surgery.
Key Takeaways
- Video-assisted thoracoscopic surgery (VATS) has been an established technique for over 20 years.
- Minimally invasive surgery reduces postoperative complications and shortens recovery time.
- VATS is preferred for peripheral lung carcinomas measuring 7 cm or less.
- Open lobectomy is often reserved for larger tumors, with a higher chance of complications.
- The choice between surgical techniques significantly impacts patient outcomes in lung cancer surgery.
The Basics of Lobectomy
Lobectomy is a key surgery that removes a lung lobe. It’s often used to treat lung cancer, the main reason for the procedure. Surgical methods like video-assisted thoracoscopic surgery (VATS) have improved a lot. They offer better results and shorter recovery times.
Definition and Purpose of Lobectomy
A lobectomy means taking out a lung lobe to deal with lung issues. Its main aim is to get rid of cancer while saving as much healthy lung as possible. VATS makes lobectomy better by using small cuts, which helps surgeons be more precise than older methods.
Indications for Lobectomy
Lobectomy is mostly for treating early-stage lung cancer and serious lung problems. Conditions like tuberculosis, lung abscesses, emphysema, non-cancerous tumors, and fungal infections might need this surgery too. Whether to do a lobectomy depends on how bad the lung issue is and the patient’s overall health.
History and Evolution of Lobectomy Techniques
Lobectomy’s history shows great improvements in surgery. It first required a big cut in the chest through open thoracotomy. Now, VATS has changed that. This less invasive option makes the surgery more efficient, lowers health risks, and helps patients recover faster. The progress in lobectomy reflects the big leaps in surgical technology, changing how doctors treat patients.
Understanding the Surgical Approach of Lobectomy
Lung surgery is complex, and knowing about lobectomy is key for the best patient results. There are many ways to do a lobectomy, such as open surgery or less invasive methods. Each has its benefits and disadvantages. These depend on the patient’s situation and the tumor’s details.
Overview of Surgical Techniques
The traditional way to operate on the lung is an open lobectomy. It involves a big cut to reach the sick lung part. Though it works well, this way can mean a harder recovery and more pain after. Minimally invasive methods like video-assisted thoracic surgery (VATS) use small cuts and a camera. This modern method helps patients recover faster and with fewer problems. It shows how surgery has gotten better to meet patient needs.
Differences Between Open and Minimally Invasive Approaches
Different surgeries might be better for you, based on a few things. Techniques that are less invasive, like VATS and robot-assisted surgery, are good for small tumors. But big tumors might need a thoracotomy. Each type of surgery comes with its risks, like getting an infection or bleeding. The choice of surgery depends on how big and where the tumor is and if the patient is healthy enough. This ensures the surgery fits the patient perfectly.
After surgery, most people can go back to regular life in about a month or two. But getting back to 100% can take a few months. Getting checked regularly and doing physiotherapy is very important. It helps get better faster and reduces problems like having trouble breathing.
For more stuff on lung adenocarcinoma, which is a common type of lung cancer, check out this resource.
The Open Thoracotomy Approach
The open thoracotomy technique is a classic and trusted way to perform lobectomy. Surgeons cut a big incision in the chest for direct access. This method helps surgeons see and handle lung parts better, especially during tricky operations. Even though it’s a strong choice, open thoracotomy has its pros and cons.
Technique and Procedure Description
In this surgery, doctors cut along the rib cage. The cut’s size can change based on the situation and the surgeon’s choice. They then open the chest to reach the lung. The damaged lung part is found and removed, either partly or entirely. This method lets doctors inspect nearby areas well, helping in treating advanced issues like spreading tumors.
Advantages and Disadvantages of Open Thoracotomy
Open surgery has clear benefits. It offers direct access, so doctors can do bigger removals if needed and fix problems not seen with less invasive methods. Also, the bigger cut can help manage bleeding and other issues during surgery.
- Advantages of Open Surgery:
- Enhanced visibility and access to structures.
- Ability to perform complex resections.
- Better control over intraoperative complications.
- Disadvantages:
- Longer recovery times compared to minimally invasive approaches.
- More postoperative pain and potential for complications.
- Possibly longer hospital stays.
Common Indications for Open Surgery
Open thoracotomy is mainly for advanced lung cancer. Recent guidelines suggest it when other surgeries are not suitable. It’s the top surgery for lung cancer stages I–IIIa, especially if the tumor’s size or place challenges less invasive methods. When a full lymph node check is needed, full thoracotomy is often better. Also, it’s chosen for patients with serious lung function issues because it gives surgeons precise control.
What is Minimally Invasive Surgery?
Minimally invasive surgery (MIS) is a big step forward in surgery. It aims to cut down on the harm caused by surgery. By using smaller cuts, it lessens the injury compared to the old ways. A main goal of minimally invasive surgery is to make recovery better. This is key, especially for complex surgeries like those on the lung.
Definition of Minimally Invasive Surgery
This surgery means making one to five small cuts. They are usually about an inch wide, between the ribs. This reduces damage to nearby tissues and allows for faster healing. It also lessens pain after the operation. Surgeons use special methods like video-assisted thoracoscopic surgery (VATS) and robotic-assisted surgery. These help in performing lung surgeries with more accuracy.
Benefits of Minimally Invasive Surgery Over Open Techniques
The benefits of this surgery are big. When compared to open surgery, patients often see:
- Quicker recovery times, with many getting back strength in two to three weeks.
- Far fewer complications, which means better health results.
- Shorter stays in the hospital, making the experience better for patients.
- Less pain after surgery and smaller scars, which worries people less about looks.
- Less blood loss during surgery, which helps in recovering faster.
- No need to cut ribs or breastbone, which means less injury to the chest.
Whether someone can have minimally invasive thoracic surgery depends on their situation. Yet, the benefits often make it the better choice. Studies comparing VATS sleeve lobectomy to open surgeries show similar survival rates long-term. This means the less invasive method is just as effective in treating lung cancer.

Video-Assisted Thoracoscopic Surgery (VATS)
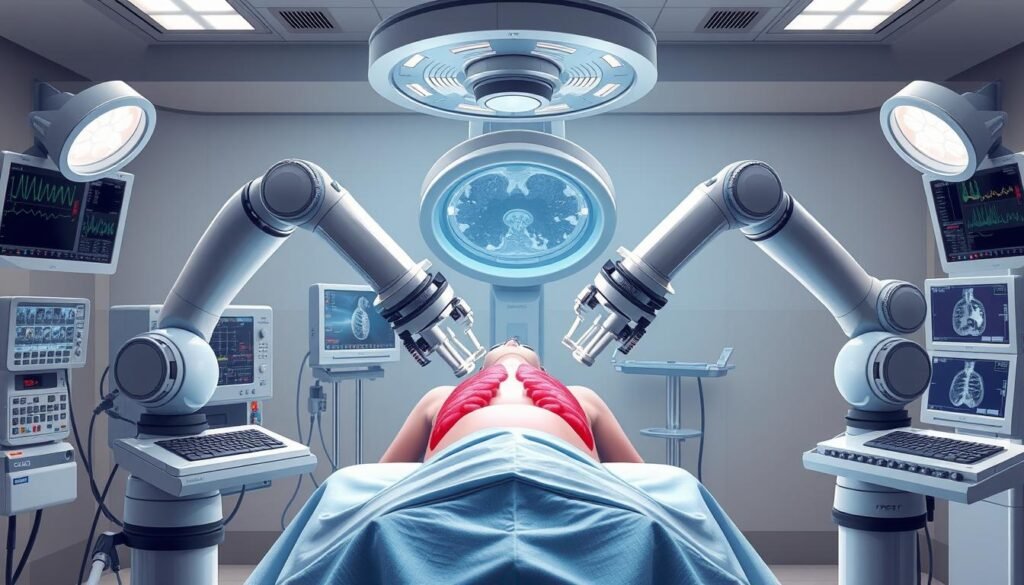
Video-Assisted Thoracoscopic Surgery (VATS) is a big step forward in minimally invasive surgery. It uses a thoracoscope with a camera and tools to perform surgery through small cuts in the chest. This method is used for things like removing lung tissue and treating lung cancer. It’s become popular due to its accuracy and shorter recovery times.
Detailed Overview of VATS Procedure
The VATS lobectomy involves removing a lung lobe through small cuts, reducing damage to nearby tissues. The surgery usually takes 2 to 3 hours. Patients often stay in the hospital for 3 to 5 days afterwards. While there are benefits, there can be risks such as pneumonia, bleeding, and nerve damage. Doctors carefully choose patients for this surgery by looking at their medical history.
Comparative Outcomes: VATS vs. Open Thoracotomy
VATS and open surgery vary greatly in recovery times and pain levels. Those who have VATS usually feel less pain and recover faster, by about two days, compared to open surgery. Studies also show VATS has fewer complications, which is good for early-stage lung cancer patients. It’s proven to be safe and offers survival rates similar to traditional surgery. To learn more about VATS, click here.
Robotic-Assisted Thoracic Surgery (RATS)
Robotic-assisted thoracic surgery (RATS) is a big step forward in surgery, especially for lung operations like lobectomy. It uses high-tech robotic systems to improve precision and control. The da Vinci robotic system is the most used since 2000. RATS tailors surgical techniques to fit each patient’s needs and case complexity.
Overview of Robotic-Assisted Techniques
The robotic-assisted surgery overview shows how robots can do complex moves in lobectomy. Surgeons get better movement, dexterity, and see things clearly in high-definition. The way it’s done varies, including how many cuts are made or if a mini-thoracotomy is needed. RATS comes with many potential upsides and challenges, affecting how long surgery takes and how much it costs.
Benefits of Robotic Assistance in Lobectomy
Key benefits of RATS include:
- Reducing shaky hands for more accurate surgery
- Giving surgeons more freedom in their movements
- Offering training chances due to the dual console
- Possibly getting better results in lymph node collection, with some studies showing higher counts than traditional methods
However, RATS can be more expensive due to one-time use tools, sometimes up to €1100 more per case than VATS. Surgeries might take longer, and there’s a big learning curve for teams.
Many experts have reviewed how effective RATS is in thoracic surgery, focusing on lobectomy. Knowing the pros and cons of RATS is key for the best patient results.
Clinical Outcomes and Effectiveness
When we look into lobectomy’s effects for lung cancer, we learn how well it works. Recent research shows big differences in how patients recover from lung surgeries. There’s a clear gap between traditional surgeries and modern, less invasive options.
Postoperative Recovery Times
Studies point out that less invasive surgeries like robotic or video-assisted lobectomy lead to quicker recoveries. Data suggests that those who have these modern surgeries usually leave the hospital in about four days. In contrast, traditional surgery patients often stay for five days. This quicker recovery highlights the benefits of newer, gentler surgical methods. It improves patient outcomes after lung cancer surgery.
Hospital Stay and Complication Rates
Looking at surgery complications, it’s clear that robotic and video-assisted methods are safer. They result in fewer problems than open surgeries. Lower complication rates mean patients are happier and healthcare costs go down. Research, including a study in the New England Journal of Medicine, shows fewer complications with lung-saving surgeries. This information guides doctors and patients in making informed decisions about lung cancer treatments.
Post-operative Care After Lobectomy
Post-op care is crucial after a lobectomy for a patient’s recovery and health. It’s important to watch patients closely to catch and handle any complications early. This kind of care helps lower recovery risks and makes getting back to everyday life easier.
Importance of Proper Post-operative Monitoring
Seeing a doctor regularly after a lobectomy is key. Patients usually meet with their doctor within a week after leaving the hospital. They then have follow-ups with an oncologist or surgeon at two and six weeks. This keeps a close eye on the patient’s health, spotting problems early for quick action.
Common Post-operative Complications
After a lobectomy, patients may face common issues like:
- Infections: Symptoms include fever and strange discharge from the cut.
- Respiratory issues: Watch for symptoms such as trouble breathing or odd phlegm.
- Hypoxemia: This needs fast treatment to keep oxygen levels right.
- Blood clots: Be alert for signs like dizziness or confusion.
- Post-thoracotomy pain syndrome: Ongoing chest pain can impact movement and life quality.
After the surgery, patients might feel weak for six to eight weeks and could have chest pain for up to three months. How soon you can drive again depends on the surgery type. Those with less invasive surgery might start in four weeks, while others could take six weeks. Light walks and breathing exercises are good for healing and improving lung health.
Lung Cancer Staging and Surgical Decision-Making
Lung cancer staging is key in decision-making for surgery. It’s vital for choosing the right surgery method. Understanding the cancer stage helps tailor treatment to improve results.
The Role of Staging in Selecting Surgical Approach
Staging helps healthcare teams pick the right surgery. It considers tumor size, location, and how far it has spread. Most non-small cell lung cancer (NSCLC) patients have tumors that have spread. This makes deciding on surgery complex.
The decision also looks at the patient’s health and the tumor’s traits. It evaluates how treatments like lobectomy can help.
Factors Influencing Surgical Decision-Making
Several factors determine the surgical method. These include:
- Tumor Size: This affects if a lobectomy or segmentectomy is possible.
- Location: Where the tumor is can dictate the surgery type and its risks.
- Patient Anatomy: Individual differences impact surgical choices.
- Patient Health: Health conditions, measured by tools like the Charlson-Deyo index, guide the surgical plan.
- Surgeon Experience: The surgeon’s skill set influences their recommendations.
These considerations lead to tailored treatments and aim for better survival rates. Evidence shows lobectomy brings better five-year survival rates for certain tumors. Matching the surgical approach with the cancer stage and patient details helps improve outcomes.
Comparative Oncological Outcomes
Choosing between video-assisted thoracoscopic surgery (VATS) and open surgery for lung cancer is a hot research topic. Studies comparing VATS and open surgery shed light on patient health and recovery. Data from 47,054 patients show trends based on the surgical method used.
Research Findings on VATS and Open Surgery Outcomes
Looking at 19 studies, less invasive surgery has clear benefits in short-term death rates for lung cancer. The risk ratio was 0.45, showing VATS patients had lower death risks versus open surgery ones. This was true even for older patients, with a similar odds ratio. Yet, high-risk patients didn’t significantly benefit from less invasive methods. This suggests surgery choices should be custom to the patient.
Long-term Survival Rates and Recurrence
Studies found no big difference in long-term survival rates after lobectomy between the two surgical methods. The 5-year recurrence-free survival (RFS) rate after lobectomy was 75.5%. But those having trisegmentectomy had an 84.0% RFS rate. Tumor distance from the intersegmental plane had little effect on survival rates. Segmentectomy could better preserve lung function than lobectomy. However, the risk of cancer coming back needs careful thought in decision-making.
Conclusion
In talking about lobectomy results, we see that open and less invasive ways both have pros and cons. It’s crucial to focus on what’s best for each patient when choosing a surgery method. This means looking at the patient’s health and keeping up with new surgical methods.
The choice between removing an upper or lower part of the lung matters a lot for patients. For example, taking out the upper part often leads to a longer hospital stay. Patients might also need more treatments compared to when the lower part is removed.
Such choices affect how fast patients recover and the cost of healthcare. It also impacts how healthcare resources are used.
Looking ahead, it’s important to keep researching and improving lung surgery methods. A deeper knowledge about these surgeries will help in giving patients better care. It’s about finding the right surgery for each person.
This progress aims to improve how doctors care for patients. Ideally, it leads to better survival chances for those getting lung surgery.