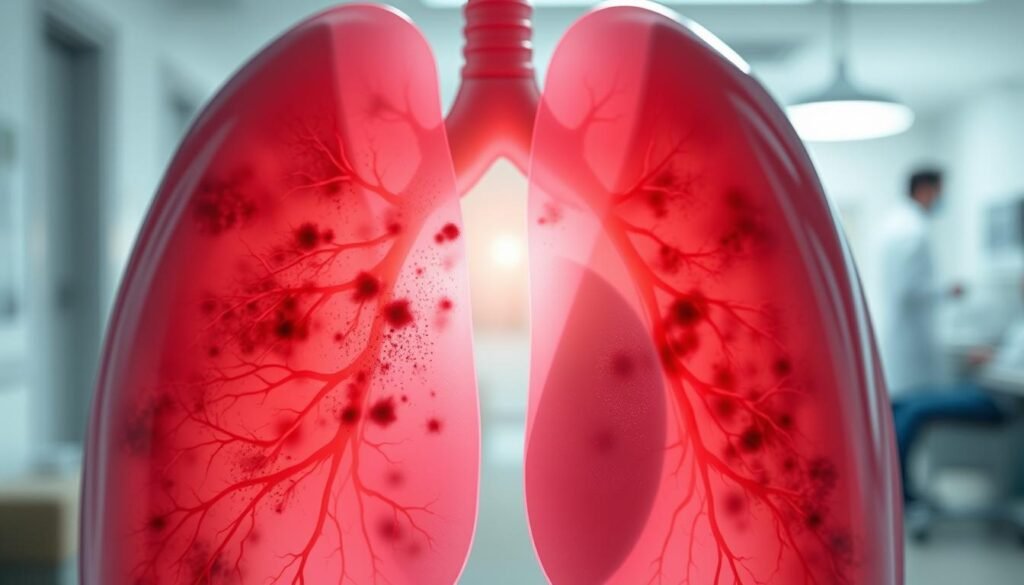
Lung cancer causes nearly 1 in 5 cancer deaths in the U.S. This fact shows the heavy toll lung cancer takes on public health. The lung cancer impact factor tells us about lung cancer today and the progress in research and treatment to help patients.
In exploring lung cancer research, we see important changes in how we manage lung cancer. There are 31 review articles and 125 experts discussing lung cancer treatment’s complexity. Their work highlights advancements in machine learning and targeted therapy, giving hope to decrease deaths from this disease. For more details, visit lung cancer statistics.
The impact of COVID-19 on healthcare emphasizes the need to understand current lung cancer data. Studies on patient demographics, diagnosis stages, and survival rates are key to improving treatments and patients’ lives. This dedication to innovative lung cancer solutions is promising for the future.
Key Takeaways
- Lung cancer is responsible for nearly 20% of all cancer-related deaths in the U.S.
- Ongoing research has produced 31 review articles focusing on various aspects of lung cancer management.
- Collaboration among 125 experts has led to advancements in treatments and surgical techniques.
- Recent studies emphasize the role of machine learning and targeted therapies in lung cancer prediction and management.
- Improving lung cancer screening guidelines is essential for early detection and better survival rates.
- The impact of demographic factors highlights necessary strategies to reduce lung cancer disparities.
- Understanding the significance of current lung cancer impact factor data is crucial for developing effective treatment plans.
Introduction to Lung Cancer and Its Impact
Lung cancer is the top cause of cancer deaths in the United States. Every year, about 225,000 new cases are found. It’s vital to understand this since almost 160,000 people die from it annually.
Smoking is the main reason behind lung cancer, linked to 90% of cases. Men who smoke are at a greater risk. Being around smoke can also increase your chances by 20 to 30%. Exposure to things like asbestos and radon adds to the risk.
Around the world, lung cancer makes up 12.4% of all cancer diagnoses. In the U.S., more men die from it than women. Sadly, many cases are in poorer countries, showing a need for better awareness and action.
Lung cancer is mainly divided into NSCLC and SCLC types. NSCLC is the most common, making up 80% to 85% of cases. It includes types such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Knowing these types is key for choosing treatments.
The impact of lung cancer isn’t just physical. It deeply affects patients’ and their families’ emotional wellbeing. So, discussing lung cancer means looking at both the numbers and the personal stories.
Lung Cancer Statistics Overview
Lung cancer statistics are key in understanding the disease’s impact. The number of people affected by lung cancer is huge worldwide. Recent statistics highlight trends and future estimates of lung cancer cases.
Current Rates of Lung Cancer Incidence
The numbers from 2022 show a grim picture. Around 2,480,675 people worldwide were diagnosed with lung cancer. The United States saw 226,033 of these cases, with a rate of 31.9 per 100,000 people.
Men are more likely to be diagnosed than women. Globally, 1,572,045 men got lung cancer, at a rate of 32.1 per 100,000. Women had 908,630 cases, with a rate of 16.2 per 100,000. Turkey had the highest rate for men at 68.0 per 100,000, showcasing regional differences in lung cancer rates.
Projected Lung Cancer Cases for 2024
In 2024, about 234,580 new lung cancer cases are expected in the U.S. This will be 11.7% of all new cancer cases. It’s vital for healthcare professionals to understand these numbers for better prevention and treatment.
| Region | New Lung Cancer Cases (2022) | Age-Standardized Rate (ASR) per 100,000 |
|---|---|---|
| Global Total | 2,480,675 | N/A |
| United States | 226,033 | 31.9 |
| Men (Global) | 1,572,045 | 32.1 |
| Women (Global) | 908,630 | 16.2 |
| Highest ASR (Turkey, Men) | N/A | 68.0 |
The Significance of Lung Cancer Impact Factor
Understanding the lung cancer impact factor is crucial in evaluating research quality. Researchers and medical institutions measure scientific studies’ influence in lung cancer through this metric. It acts as a quality benchmark and encourages further studies for better treatment and early diagnosis.
Understanding the Impact Factor Metrics
Impact factor metrics measure a journal’s importance to the scientific community, especially in lung cancer research. For instance, the Translational Lung Cancer Research journal reached an impact factor of 5.132 in 2019. This shows the journal’s academic strength and its role in pushing forward lung cancer research.
TLCR, peer-reviewed and recognized by SCIE and PubMed/PubMed Central, focuses on new developments in lung cancer and related diseases. It adopts clear reporting guidelines and transparent peer review, ensuring high publishing standards. This improves research quality significantly.
Impact factor metrics shape funding decisions and future research directions. Funding bodies and policymakers use this data to allocate resources effectively. They aim at research with the potential to deepen our lung cancer understanding. By focusing on high-impact journals, researchers can contribute to significant discoveries in the field.
Evaluating research through impact factors shows current priorities and identifies areas needing advancement. High-quality research is vital in combating lung cancer, the leading cause of cancer deaths worldwide.
Trends in Lung Cancer Survival Rates
Lung cancer survival rates have improved thanks to better early detection and treatments. These changes tell us a lot about patient outcomes and healthcare success.
Analysis of Five-Year Relative Survival Data
The national five-year survival rate for lung cancer is now 26.6%. This number is remarkable given the disease’s difficulties. The survival rate for people of color has increased by 17% in two years.
This shows efforts to reduce healthcare gaps are working. From 2015 to 2019, lung cancer survival rates jumped by 22%.
| Year | Five-Year Survival Rate | Population Group |
|---|---|---|
| 2015 | 21.9% | Overall |
| 2019 | 26.6% | Overall |
| 2021 | 39.4% | People of Color |
Improvements Over Time in Survival Rates
Lung cancer survival has positively grown over the years. This is due to better screening and treatments. However, only 26.6% of cases are caught early while 44% are found late.
Late diagnoses hurt survival rates. Our goal is to catch cancer earlier so more people can get timely help.
Even with hurdles, new treatments are making a difference in survival rates. More awareness, screenings, and fair treatment access are vital. They will help continue this positive trend in survival rates.
Lung Cancer Diagnosis and Early Detection
Finding lung cancer early is key to increasing survival rates. Tests that spot the disease early are very important. They improve treatment options and the overall health of people at risk.
The Importance of Diagnostic Screening
Screening tests are critical for catching lung cancer early. Using low-dose CT (LDCT) scans has lowered death rates in high-risk groups. This is better than using regular chest x-rays. The National Lung Screening Trial (NLST) shows LDCT screening cut deaths by 20.0%.
But, LDCT screening isn’t perfect. It has a 23.3% chance of false positives. This can lead to unnecessary stress and medical follow-ups.
Recent Changes in Screening Guidelines
The American Cancer Society now advises yearly LDCT scans for those 50 to 80 years old with a heavy smoking history. This advice is for those who’ve smoked 20 pack-years or more. The new guidelines aim to diagnose lung cancer earlier for more people.
Yearly screenings are usually paid for by Medicare and many insurance companies. This makes it easier for more people to get tested. As LDCT screening becomes more common, we need skilled doctors and better machines.
New techniques and equipment are making it easier to find lung cancer early. Tests like white light bronchoscopy, PET/CT, and liquid biopsies are promising. Thanks to technology, our main goal stays the same – to save lives by finding cancer early.
Lung Cancer Treatment Advances
Lung cancer treatment has seen big improvements recently, bringing new hope to patients. Innovations include targeted therapies and immunotherapies. These have yielded promising outcomes. Also, personalized medicine has grown in importance. It uses biomarker testing to find the best treatments for each person’s disease.
Emerging Treatments and Therapies
New treatments for lung cancer are making a big difference. They work for specific kinds of cancer. Drugs like pembrolizumab and nivolumab are leading the way for advanced lung cancers. They have helped double survival rates for many patients, marking a major leap in treatment success.
- Targeted therapies for certain gene mutations are more common now.
- Less invasive surgical methods mean quicker recovery for patients.
- Radiotherapy, especially SABR, has shown much better survival rates.
Role of Biomarker Testing in Treatment
Biomarker testing is key in fighting lung cancer. It helps doctors customize treatment for each patient’s cancer type. This approach identifies the genetic makeup of the tumor. It helps in choosing the best treatment. By using biomarker testing, treatments become more effective, leading to better results for patients.
“The integration of biomarker testing in the treatment plan has led to significant advancements in personalized care for lung cancer patients.”

| Treatment Type | Survival Rate | Key Notes |
|---|---|---|
| Immunotherapy | Up to 80% for eligible patients | Targets advanced NSCLC with positive outcomes. |
| Stereotactic Radiotherapy | 70% at 2 years | Minimally invasive, focused radiation approach. |
| Surgery (Video-Assisted Thoracoscopic) | 80.1% at 5 years | Less invasive, lower recovery time compared to open lobectomy. |
| Targeted Drugs | Varies by mutation | Effective for specific genetic mutations. |
New therapies and biomarker testing are changing lung cancer care. They open a new chapter in oncology. As research goes on, the hope for patients keeps growing. This means better survival chances and quality of life.
Lung Cancer Risk Factors
Lung cancer is linked with different risk factors and causes. Knowing them helps in prevention. Smoking and environmental exposures are major risks. Differences in race, ethnicity, and social factors also affect vulnerability.
Primary Causes of Lung Cancer
Many factors add to the risk of lung cancer. Smoking cigarettes causes about 80% of deaths from lung cancer. Other tobacco products also pose risks. Being around secondhand smoke is the third leading cause of lung cancer in the US.
- About 80% of lung cancer deaths are linked to smoking.
- Radon exposure ranks as the second-leading cause, particularly affecting smokers and non-smokers alike.
- Asbestos exposure significantly increases lung cancer risk, especially among workers in specific industries.
- Other environmental factors, such as outdoor air pollution, have been associated with 1% to 2% of lung cancer deaths.
- Radiation therapy for other cancers can elevate lung cancer risk in survivors.
New research suggests marijuana smoking and e-cigarettes may also increase lung cancer risk. Beta-carotene supplements could raise the risk in smokers as well.
Demographic Variances in Risk Factors
Demographic differences matter in lung cancer risks. Certain groups face more exposure to smoking and its effects. For example, working with hazardous materials like asbestos increases risk. High air pollution levels also make some more vulnerable.
| Demographic Factors | Risk Levels |
|---|---|
| Smoking Cessation Rates | Lower in some minorities |
| Exposure to Secondhand Smoke | Higher in urban areas |
| Occupational Hazards | Higher in specific industries (e.g., construction) |
| Access to Healthcare | Limited for ethnically diverse groups |
Recognizing these differences is key to improving prevention and treatment. It leads to better health outcomes for all.
Lung Cancer Symptoms to Watch For
It’s vital to recognize lung cancer symptoms early. Patients see a mix of signs, from common to rare. Knowing these helps people get medical attention for lung cancer early.
Common and Rare Symptoms of Lung Cancer
Persistent coughing is a top common symptom. It may come with chest pain and breathing problems. People might also feel tired, wheeze, and have a hoarse voice.
Small cell lung cancer brings extra troubles like losing appetite, coughing up blood, and more shortness of breath.
Rarer symptoms show up as the cancer grows. These include:
- Bone pain in the back, pelvis, or limbs
- Brain metastasis causing headaches
- Jaundice from liver issues
- Lumps in the neck or collarbone
Watch for paraneoplastic syndrome too. It causes muscle cramps, weakness, high blood calcium, and odd fingertips.
When to Seek Medical Attention
Don’t wait to get medical attention for lung cancer if you see warning signs. Early spotting can boost survival chances. See a doctor if these apply:
- A cough that won’t quit for weeks
- Chest pain, especially with deep breaths
- Odd weight loss or less hunger
- Spitting up blood or rust-colored spit
The Lung Cancer Centers at City of Hope have experts like oncologists and surgeons. They give both medical and support care to help the whole patient.
For more on spotting lung cancer symptoms and next steps, check out reliable sources.
The Role of Lung Cancer Research
Lung cancer research is key in understanding this illness and making new treatments. It looks at ways to improve care and help patients live longer. These efforts are critical because they make treatments better.
Current Research Trends and Focus Areas
Research in lung cancer is very active right now. It focuses on many areas, such as:
- Creating new immunotherapies, like Atezolizumab and pembrolizumab, for early-stage non-small cell lung cancer (NSCLC).
- Using artificial intelligence to diagnose lung cancer more accurately, hitting a 97% success rate.
- Testing how targeted therapies and immunotherapy work together to improve how well patients do.
Impact of Research on Treatment Options
New treatments have really changed how we care for lung cancer patients. There’s strong proof that these treatments work:
| Treatment Type | Medication | Indications |
|---|---|---|
| Immunotherapy | Atezolizumab (Tecentriq) | Approved for early-stage NSCLC |
| Targeted Therapy | Alectinib (Alecensa) | Approved for ALK-positive NSCLC |
| KRAS Inhibitor | Sotorasib (Lumakras) | Advanced lung cancer with KRAS mutations |
| B-Raf Targeted Therapy | Dabrafenib (Tafinlar) and Trametinib (Mekinist) | Specific mutation in the BRAF gene |
As research continues, it will bring more options for treating lung cancer. This means better chances of survival and life quality for patients.
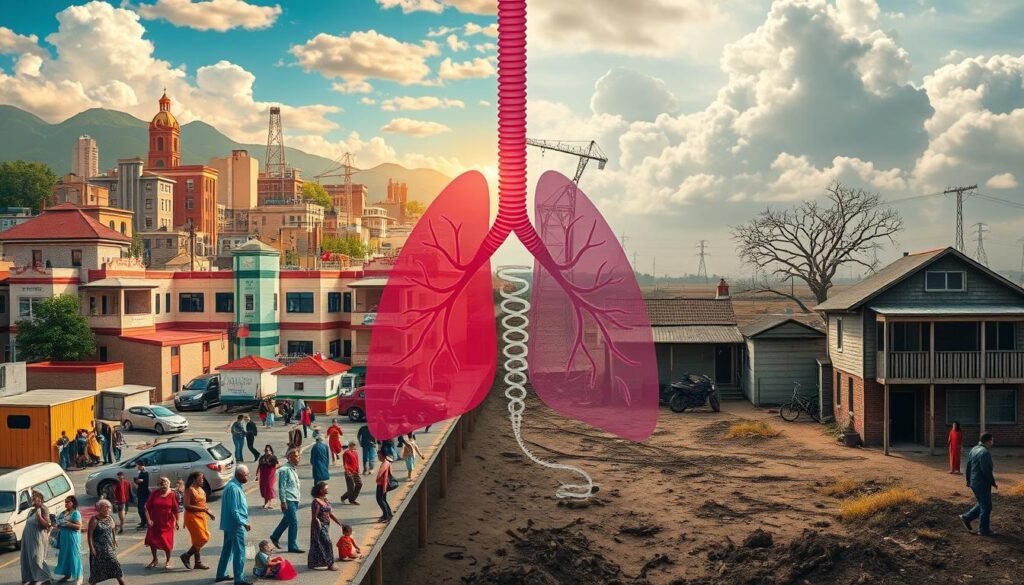
Addressing Disparities in Lung Cancer Outcomes
In the U.S., racial and ethnic minorities face worse lung cancer outcomes. Survival rates and access to treatment show deep systemic issues in our healthcare. We need to understand why care and outcomes differ so much among groups.
Impact of Racial and Ethnic Disparities
Studies show African American patients often have lung cancer found at later stages. They also have lower survival rates and don’t get screened as much as White people. There’s a troubling fact: Black patients are 16% less likely to find out early they have lung cancer. They are also 19% less likely to get surgery for lung cancer. The National Institute on Minority Health shows it’s vital to tackle these issues, considering factors like sex, income, and where people live.
Strategies to Improve Outcomes for Minority Groups
There are ways to help close these gaps. Improving early screening and treatment is key. For instance, low-dose CT scans can cut lung cancer deaths by 20-24%. But not many people get screened – only 3% to 20%, depending on the group. We must promote better use of screening.
Working together, healthcare systems can make screening more accessible and educate patients more effectively. By using strategies that meet racial and ethnic minorities’ specific needs, we can make a difference. Making big changes in policy and at the organizational level will help everyone have equal access to lung cancer care.
| Group | Early Diagnosis Likelihood | Surgical Treatment Access | No Treatment Likelihood |
|---|---|---|---|
| African American | 16% less likely | 19% less likely | 7% more likely |
| White | |||
| Hispanic | Lower risk | Higher risk | Lower mortality |
Conclusion
Lung cancer greatly affects people’s lives and understanding it is key. About 234,580 new cases are expected in the U.S. in 2024. It’s the top cause of cancer deaths. This makes it important for doctors and everyone else to know about lung cancer.
Making people aware and finding it early could help more people survive. Right now, only 15.6% live more than five years after finding they have lung cancer. This shows why we need to work on prevention and early detection.
The future looks bright for treating lung cancer. New research and treatments are coming out. They are changing how we treat patients by focusing on what each person needs.
This means care is getting better and more personal. But, it’s also important to make sure everyone gets the same chance at getting better, no matter their race or background.
To really fight lung cancer, we need to work together. Knowing about the disease, advancing research, and helping each other are key. As new information and treatments become available, our goal should stay the same. We want to see fewer people getting lung cancer and more people living longer, healthier lives after a diagnosis.