In the United States, lung cancer is the second most common cancer in women and is the top cause of cancer deaths. This fact makes it very important to understand what causes lung cancer in women. Women have a 1 in 17 chance of getting this serious disease in their lifetime, so knowing the factors that increase its risk is key.
Not all women with lung cancer have smoked. In fact, a large number of female lung cancer cases are in non-smokers. This shows how important it is to know about all the lung cancer risk factors, not just smoking. Understanding what leads to lung cancer, especially in women, is key to ending wrong ideas about the disease.
Lung cancer deaths are more than just numbers. They represent the stories of many people and families impacted by this disease. Looking into the causes and risk factors shows the importance of focusing on research and education. This can lead to early detection and better survival chances for women.
Key Takeaways
- Lung cancer is the leading cause of cancer-related deaths among women.
- A significant number of women diagnosed with lung cancer have never smoked.
- Understanding risk factors is essential in paving the way for improved lung cancer awareness.
- Women have a higher lifetime risk of developing lung cancer compared to men, irrespective of smoking habits.
- Early detection significantly impacts survival rates for female lung cancer patients.
Introduction to Lung Cancer in Women
Lung cancer is a significant health issue, particularly for lung cancer in women. It’s the second most common cancer found in females in the U.S. This has sparked important conversations about its prevalence. Notably, lung cancer affects women beyond just those who smoke or have been around smoke.
Studies show clear gender differences in lung cancer. Women often have different symptoms. They can also progress to more serious stages quicker with certain types, like adenocarcinoma. The rise in cases among younger women highlights an urgent need for awareness.
Over the last 43 years, women’s lung cancer diagnoses surged by 84%. Meanwhile, men’s cases have dropped by 36%. It’s crucial to spread knowledge on risk factors such as genes and the environment. This can help in cutting down the disease’s impact.
Current Statistics on Lung Cancer in Female Patients
Lung cancer is the top cause of cancer deaths in the United States, especially among women. About 118,270 new cases are expected in women in 2024. This shows lung cancer’s impact, being the second most common cancer for both men and women.
Projected lung cancer deaths in women are about 59,280 for the year. This figure points out lung cancer’s high prevalence in women. It causes more deaths than colon, breast, and prostate cancers combined.
The average age for lung cancer diagnosis is around 70, mainly in those 65 and older. Though women have a 1 in 17 lifetime risk, versus 1 in 16 for men, there’s hope. The five-year survival rate for women has risen to 15% from 11% for men.
Black men are 12% more likely to get lung cancer than White men. Black women, however, have a 16% lower rate than White women. These differences highlight lung cancer’s varied impacts on different groups.
More people quitting smoking has led to fewer new lung cancer cases. Yet, 10-15% of all lung cancer in the U.S. occurs in nonsmokers. Women are more affected by this.
| Statistic | Number |
|---|---|
| Estimated new lung cancer cases (women, 2024) | 118,270 |
| Estimated lung cancer deaths (women, 2024) | 59,280 |
| Lifetime risk of developing lung cancer (women) | 1 in 17 |
| 5-year survival rate (women) | 15% |
| Lung cancer attributed to nonsmokers | 10-15% |
Understanding the Causes of Lung Cancer in Females
Lung cancer in females is caused by many factors. These factors show us how complex the disease is. Some women have a genetic risk, especially if lung cancer runs in their family.
Things like air pollution and harmful substances also play a big part. For women who don’t smoke, secondhand smoke is a huge concern. This is especially true for women living with smokers.
Genetic Factors in Lung Cancer Development
Some women have genes that make them more likely to get lung cancer. The EGFR gene mutation is one example. If a woman’s family has had lung cancer, she is at greater risk.
Knowing this, women can make better choices for their health. They can also take steps to prevent the disease.
Environmental Exposures and Their Role
The environment around us can increase lung cancer risks for women. Air pollution, especially in cities, is a big problem. Also, radon gas and chemicals can raise these risks.
Women who live near factories or are exposed to these dangers need to be careful. These environmental challenges put them at a higher risk.
How Secondhand Smoke Contributes to Risk
Secondhand smoke doesn’t just affect smokers. It’s a big problem for women living with smokers too. Every year, it causes many lung cancer cases in the U.S.
This shows why we need to be aware and protect everyone from secondhand smoke. It’s important for women’s health.
| Category | Details |
|---|---|
| Genetic Risk Factors | Mutations in genes like EGFR; family history increases susceptibility |
| Environmental Risk Factors | Air pollution; radon exposure; industrial chemical exposure |
| Secondhand Smoke Effects | Thousands of cases annually; especially dangerous for women in non-smoking households |
The Impact of Smoking on Female Lung Cancer Rates
Smoking is a leading cause in the rise of lung cancer among women. The history of women’s smoking sheds light on major trends. After World War II, more women started smoking, which has been linked to more lung cancer cases. This change has had a profound effect on women’s health.
The Historical Context of Smoking Among Women
In the mid-20th century, views on smoking among women shifted. What was once frowned upon became a sign of freedom and style. This led to more women smoking. From 1975 to 2014, the number of women who smoked jumped from 20% to over 30%. This change went hand-in-hand with a rise in lung cancer cases among women.
Recent data highlights this troubling trend. Between 2010 and 2018, lung cancer among women went up by 5% each year. This is a stark contrast to the rates in men, which have stayed more or less the same.
Gender Differences in Smoking & Lung Cancer Risk
When it comes to lung cancer, men and women face different risks. Research shows women might process harmful substances from tobacco differently. This means they could be more at risk, even if they smoke less than men. For women, the risk of lung cancer is high, with a relative risk figure of 6.99 compared to 7.33 for men. These differences highlight how smoking has a unique impact on women’s lung cancer rates.
| Year | Women Smoking Prevalence (%) | Lung Cancer Incidence (per 100,000 person-years) |
|---|---|---|
| 1975 | 20 | 23.2 |
| 2014 | 30 | Increasing |
| 2010-2018 | – | 5% Annual Increase |
Risk Factors for Lung Cancer in Women
Lung cancer is a major health risk for women. It’s important to know the factors that can lead to it. This knowledge can help with prevention and awareness.
Age and Its Effect on Lung Cancer Incidence
As people get older, their risk for lung cancer goes up. After 70, this risk increases significantly. This happens because older people have been around more harmful substances.
Family History and Genetic Predisposition
Having lung cancer in your family raises your own risk. If lung cancer is common in your family, you’re more likely to get it too. Also, certain genes like KRAS can make tumors grow faster. Women with family members who got lung cancer young need to be extra careful.
Occupational Hazards Associated with Lung Cancer
Some jobs can put you at a higher risk for lung cancer. For example, working with asbestos is very dangerous. Smoking can make this danger even worse. Other risky substances include radioactive ores, chemicals, and diesel exhaust. Knowing about these risks is important for women in these jobs.
| Risk Factor | Impact |
|---|---|
| Age | Significantly increases risk, especially after 70 |
| Genetic Predisposition | Higher likelihood with a family history of lung cancer |
| Occupational Hazards | Substantial risk from asbestos and other carcinogens |
Common Symptoms of Lung Cancer in Women
It’s critical to know the symptoms of lung cancer in women for early detection. Many symptoms might be overlooked or wrongly attributed to other illnesses. This delay can make diagnosis harder. It’s important for women to know these signs since some are more common in females.
How Symptoms May Present Differently in Women
Women’s lung cancer symptoms can differ from men’s. The common signs include:
- Fatigue
- Shortness of breath
- Persistent cough, although this is less common
- Unexplained weight loss
- Chest pain, particularly if lung cancer invades the pleura
- Coughing up blood, found in about 21% of patients
- Back pain or shoulder pain when metastases occur
- Recurring respiratory infections
Spotting these early signs is crucial for improving treatment success. Early diagnosis helps treatments work better. For details on lung cancer risk factors, check out this resource.
Importance of Recognizing Early Warning Signs
Being aware of early warning signs is key for lung health. Symptoms like hoarseness, new wheezing, or signs of cancer spreading demand urgent medical attention. Advocating for in-depth checks is important. Many women with lung cancer, including 20% non-smokers, didn’t show early disease signs. Symptoms such as fatigue and frequent bronchitis need quick action.

Lung Cancer Diagnosis and Screening Methods
Lung cancer diagnosis relies on various screening methods for proper detection and care. Finding lung cancer early greatly improves chances of beating it. Hence, knowing about these methods is very important. People over 50 who smoked a lot, or quit in the past 15 years, should get checked regularly.
Diagnosis starts with imaging tests. Tools like CT scans show images in slices, while MRI scans give clear pictures of soft tissues. These tests help figure out tumor size and if the cancer has spread.
Imaging aside, biopsies are crucial for confirming lung cancer. Methods like needle biopsies and bronchoscopies get tissue samples. These are needed to find cancer cells. Using endobronchial ultrasound (EBUS) is a less invasive way to check the lungs.
Lung cancer is staged from 1 to 4, showing tumor growth and spread. Knowing the stage helps tailor treatment and offers prognosis insight. Early detection through screenings is key to finding lung cancer at treatable stages.
Effective screening methods are vital for high-risk groups. They allow for early intervention. This fight against lung cancer underlines the value of early detection and continuous medical care.
Different Types of Lung Cancer Affecting Women
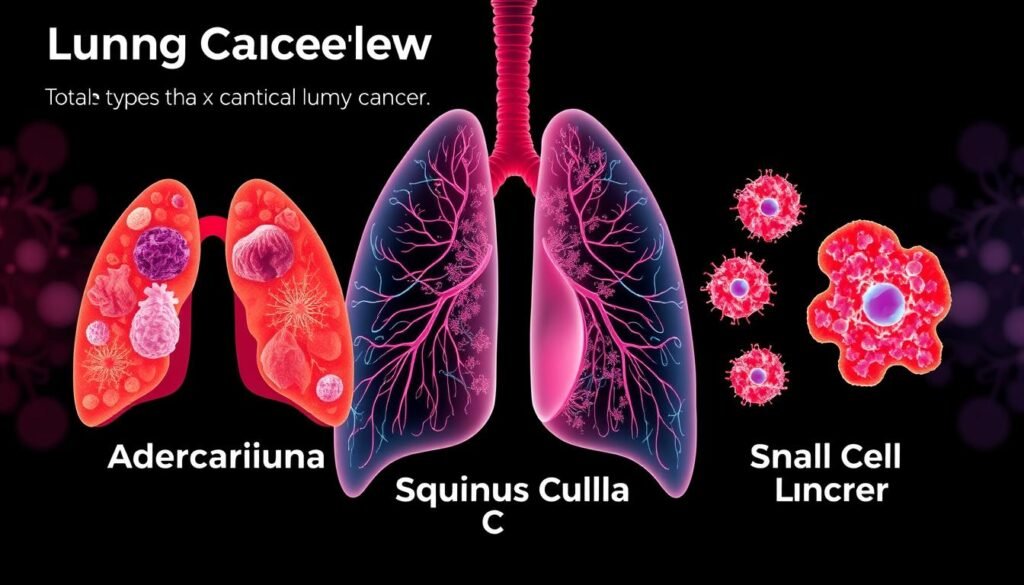
Lung cancer appears in many forms, impacting women significantly. It’s vital to know the differences for effective prevention and care. Non-small cell lung cancer and small cell lung cancer are most common in women. They grow differently and need unique treatments.
Small Cell Lung Cancer vs. Non-Small Cell Lung Cancer
Small cell lung cancer (SCLC) makes up 10% to 15% of lung cancers. It grows and spreads fast, leading to a tougher battle. Meanwhile, non-small cell lung cancer (NSCLC) is more frequent, accounting for 80% to 85% of cases. NSCLC grows slower and comes in types like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. It usually gives patients more options for treatment.
Adenocarcinoma and Its Rising Prevalence in Women
Adenocarcinoma is the lead in non-small cell lung cancer, especially among women. They’re getting diagnosed more often than men. This cancer represents 41.4% of lung cancer in women. Its increasing presence is alarming, as many find out they have it when it’s advanced. Other types, like squamous cell carcinoma, are mainly tied to smoking. Large cell carcinoma is known for fast growth and being hard to treat.
Treatment Options for Female Lung Cancer Patients
Treatment options for women with lung cancer might be like those for men. But, they can be adjusted to meet their unique needs. Treatments include chemotherapy, immunotherapy, targeted therapy, and surgeries. Each is key depending on the stage of cancer and the patient’s health.
For early-stage lung cancer, surgery might be all that’s needed for a cure. Some Stage 0 cases might use non-invasive methods like photodynamic therapy. For Stage I, surgery is often the go-to, but some cases might need more treatment.
Stage II may require chemo before surgery, sometimes with immunotherapy. By Stage IIIA, treatment often includes chemo, radiation, and possibly surgery. For Stage IIIB, surgery usually isn’t an option, leaving chemo and radiation.
In advanced stages, like IVA and IVB, treating lung cancer gets more complex. Here, a combination of surgery, chemo, targeted therapies, and radiation is used to extend life. The choice of therapy is heavily influenced by specific genetic mutations in the cancer cells.
Working together, specialized teams at top centers like the Lung Center at Brigham and Women’s Hospital boost treatment success. These teams bring together experts in various fields to give patients the best care. Knowing your treatment options helps in making informed choices and improving health outcomes.
For detailed information about treatments, including chemotherapy and targeted therapies, visit this resource.
Prevention Strategies for Lung Cancer in Women
Stopping lung cancer before it starts is key to lessening its impact on women. Making certain lifestyle changes can greatly reduce the risk of getting this disease. It’s important for those at risk to not smoke, eat healthily, and stay active.
Reducing Risk Through Lifestyle Changes
Making key lifestyle changes is a big step in preventing lung cancer. Not smoking is the most important, as it raises lung cancer risk a lot in smokers compared to nonsmokers. It’s also vital to avoid secondhand smoke because it can increase a nonsmoker’s risk of getting lung cancer by about 20%.
Eating lots of fruits and veggies can help your lungs stay healthy. But eating well can’t cancel out the harms of smoking. Being active and keeping a healthy weight can also help keep your lungs healthy and prevent lung cancer.
The Importance of Screening and Early Detection
Screening for lung cancer early, especially in women with risk factors like smoking, is crucial. High-risk individuals should get low-dose CT scans to catch issues early. This way, problems can be dealt with quickly.
Regular screening can change the course of the disease, by finding it early. Talking to a doctor about when and how to screen is a proactive step for any woman’s health.
Taking steps early can really improve your health. For more info on how to prevent lung cancer, visit this resource.
| Risk Factor | Impact on Lung Cancer |
|---|---|
| Smoking | Increases risk by approximately 20 times |
| Secondhand Smoke | Increases risk by about 20% |
| Radiation Exposure | Increases incidence and mortality |
| Occupational Carcinogens | Increases risk by more than fivefold |
| Indoor Radon Exposure | Higher risk, especially among smokers |
| Diet | Rich in fruits and vegetables may reduce risk |
| Physical Activity | Supports overall health and lung cancer prevention |
Stigma Surrounding Lung Cancer in Women
The stigma of lung cancer affects those diagnosed, especially women. Many believe it mainly hits smokers. This view overlooks non-smokers who also get lung cancer. It’s vital to raise awareness to dispel these myths.
In the U.S., over 226,000 new lung and bronchus cancer cases are expected this year. It’s shocking that lung cancer is the top cause of cancer death for both genders. The myth that only smokers get lung cancer harms 26% of diagnosed non-smokers. This stigma makes them feel ashamed and alone.
Educating the public can make a supportive environment for those with the disease. Studies show high psychological distress among lung cancer survivors, worsened by stigma. Bringing different smoking statuses together in focus groups can spark empathy and understanding.
We must address the stigma around lung cancer in women to support early detection and treatment. Recognizing that anyone can be affected, regardless of smoking history, will increase support. Enhancing awareness is key to reducing stigma and providing the care patients need.
Current Research and Advancements in Treatment
Current studies focus on new ways to treat lung cancer in women. They aim to find better treatments to help patients live longer, better lives. This research looks into many promising areas.
Recent work has shown that low-dose CT scans can find lung cancer early in people 50–80 years old who have smoked a lot. Also, machines that learn can now spot two types of lung cancer and certain genetic changes with 97% accuracy.
Immunotherapy is making big leaps forward. It helps some people with a type of lung cancer called NSCLC, especially after surgery for early-stage disease. Drugs like Alectinib (Alecensa) and Osimertinib (Tagrisso) are helping patients with certain genetic changes fight their cancer better.
Medicines such as Crizotinib (Xalkori) and Entrectinib (Rozlytrek) are targeting specific genes in advanced NSCLC. Plus, combining dabrafenib (Tafinlar) and trametinib (Mekinist) is proving effective for patients with certain gene mutations.
A comprehensive overview of some significant therapies is outlined in the table below:
| Treatment | Target | Year Approved | Indication |
|---|---|---|---|
| Alectinib (Alecensa) | ALK | 2024 | Adjuvant therapy for earlier-stage NSCLC |
| Osimertinib (Tagrisso) | EGFR | 2021 | After surgery for early-stage NSCLC with EGFR mutations |
| Crizotinib (Xalkori) | ROS1 | 2011 | Metastatic NSCLC |
| Entrectinib (Rozlytrek) | ROS1 | 2019 | Metastatic NSCLC |
| Dabrafenib (Tafinlar) + Trametinib (Mekinist) | BRAF | 2018 | NSCLC with specific BRAF mutations |
| Sotorasib (Lumakras) | KRAS | 2021 | Advanced lung cancer with KRAS mutations |
The study of lung cancer in women is very important. It looks at how cancer affects women differently. These studies are key to making medicine more precise and effective for everyone.
Conclusion
It’s key to know why lung cancer happens to fight it, especially in women. Even though lung cancer is 13% of new cancer cases in women, many don’t know the main risks and signs. We need to focus more on making people aware. This will help catch the disease early and treat it better.
Things like age, family history, and the environment can raise a woman’s lung cancer risk. But, there’s good news because research and treatment are getting better. It’s very important to teach people about lung cancer in women. By doing this, we can make sure they know how to find it and treat it effectively.
To help women with lung cancer live longer, we must keep researching and speaking out. If we all understand lung cancer better, we can make the future healthier. This means less suffering from this disease for women everywhere.