Surgery plays a big role in treating non-small cell lung cancer (NSCLC). It’s more often used than for small cell lung cancer. Understanding different surgical methods is key. The stage of cancer at diagnosis and the patient’s health are important. Early-stage diagnosed patients have a better chance for a cure through surgery.
But, not all patients can easily undergo surgery. Issues like existing health problems and smoking history affect this. Stopping smoking before surgery improves survival rates and lowers cancer recurrence risks.
Thoracic surgery has seen advances lately. Techniques like video-assisted thoracic surgery (VATS) make surgery less invasive. This can lead to quicker recovery times. Knowing the risks and benefits of these options is vital for better cancer outcomes. We’ll look into NSCLC surgery choices, their advantages, and what to expect before and after surgery.
Key Takeaways
- Surgery is more common for non-small cell lung cancer compared to small cell lung cancer.
- Early detection is critical for a better prognosis, allowing for more treatment options.
- Patients who quit smoking before surgery often experience improved outcomes.
- Video-assisted thoracic surgery offers a less invasive alternative for lung procedures.
- Understanding cancer staging is essential to determining appropriate surgical interventions.
Understanding Non Small Cell Lung Cancer
Non small cell lung cancer (NSCLC) is the main type of lung cancer, covering about 85% of all cases. It has different histological subtypes like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Each of these has unique features, which means treatment needs to be specific.
Within NSCLC, there are various cancer types, highlighting the need for correct diagnosis. For instance, adenocarcinoma makes up 40% of NSCLC cases. On the other hand, squamous cell carcinoma is 25% to 30%. And large cell carcinoma consists of 10% to 15% of cases. Knowing these differences helps in finding the right treatment.
Risk factors significantly influence the chances of getting lung cancer. The biggest risk is smoking tobacco. Other risks include secondhand smoke, environmental toxins like asbestos, and a family history of lung cancer. As people get older, their risk of lung cancer also increases.
Common signs of non small cell lung cancer include a persistent cough and difficulty breathing. Chest pain, blood in sputum, or losing weight without trying are also signs. It’s crucial to get medical help early if you have these symptoms. Early diagnosis greatly increases the chances of a better outcome.
To diagnose this cancer, doctors use chest X-rays, CT scans, and biopsies. These tests help determine the cancer’s stage. This is key for deciding how to treat it. Raising awareness about lung cancer is important. It helps at-risk individuals and educates the public on preventing this serious disease.
Importance of Early Detection and Treatment
Lung cancer is a major health issue in the U.S. It’s the second most common cancer. It is also the top cause of cancer deaths. Knowing the stage of cancer helps doctors treat it effectively. It’s crucial to catch non-small cell lung cancer (NSCLC) early. This can help patients live longer. Studies show that low-dose CT (LDCT) scans are good at finding lung cancer early. They also reduce the risk of dying from lung cancer.
The American Cancer Society suggests yearly LDCT scans for people 50 to 80 years old. These people should have smoked a lot in the past. Specifically, they should have a 20 pack-year smoking history. LDCT scans are better than old chest X-rays because they show clearer images. This makes it easier to find lung cancer early. Early treatment can then start sooner.
Screening needs to happen at specialized places. These places have the right equipment and experts. Catching NSCLC early, like at stage IA1, gives a patient about a 92% chance of living five more years. But finding it at stage IV drops the chance to only 10%. This shows why early detection is key for choosing the right treatment.
It’s important for people at high risk to think about making healthy changes. For example, quitting smoking can help a lot. Luckily, Medicare and most insurance plans cover lung cancer screening now. So, more people can get screened. Healthy people benefit the most from screenings. Finding cancer early means better options for treatment. For more info on lung cancer screening and treatment, check out American Cancer Society and Care Your Lungs.
Surgery for Non Small Cell Lung Cancer
Surgery is a key option for those with non small cell lung cancer (NSCLC). It depends on if the cancer is resectable or not. Knowing the difference helps patients choose their treatment.
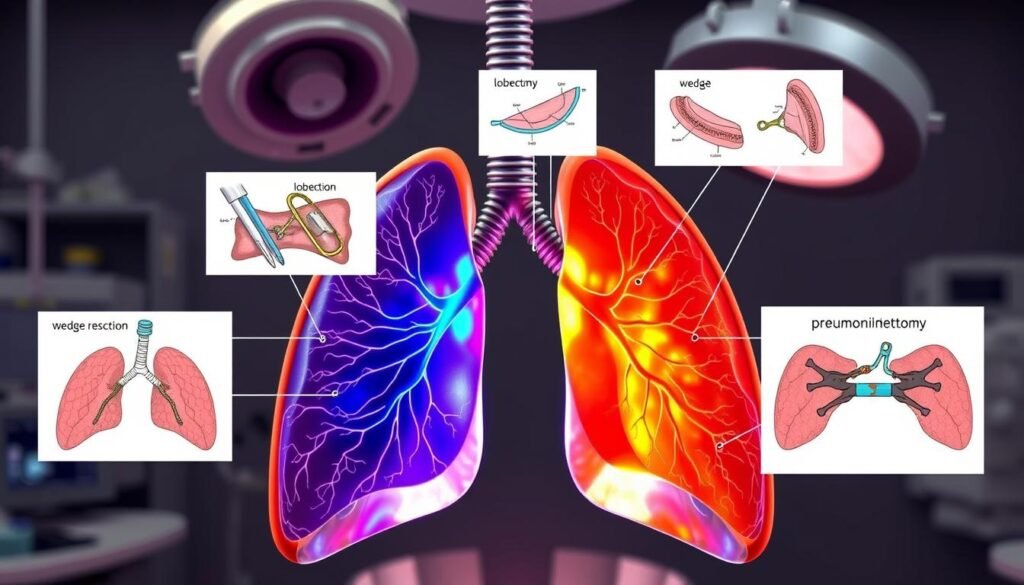
Overview of Surgical Options
There are many surgical methods for treating NSCLC. These methods include:
- Lobectomy: Removing a whole lung lobe with the tumor.
- Segmentectomy: A less invasive method that removes part of the lobe.
- Pneumonectomy: Taking out an entire lung, used in severe cases.
- Wedge resection: Cutting out a small, tumor-containing piece of lung.
Studies show lobectomy and lung-saving surgeries have good results. They both have about 80% survival rates after five years.
Defining Resectable and Unresectable Cancer
Tumors that can be fully removed are called resectable. It means surgery can get rid of the cancer cells. Unresectable cancer can’t be fully taken out, maybe because it’s too big or has spread. Doctors look at tumor size, location, and lung health to decide if surgery is possible. Early-stage NSCLC patients who had lobectomy were less likely to see their cancer return than those who had part of their lobe removed.
Choosing the right surgery can make a big difference in outcomes. Talking with doctors about what’s best for your case is crucial. This helps in planning the fight against non small cell lung cancer.
Types of Lung Surgery
There are many surgeries to treat non-small cell lung cancer (NSCLC). The kind of surgery needed depends on the tumor, health, and lung function. Here are the main surgical options.
Pneumonectomy: Removing an Entire Lung
Pneumonectomy means taking out one lung. It’s done when the tumor is too big to leave any healthy lung behind. After this surgery, patients need careful watching because their breathing is greatly affected.
Lobectomy: Resection of a Lung Lobe
Lobectomy involves removing a lung lobe. It strikes a balance between taking out cancer and saving lung function. Recovery is usually easier, making it a go-to when the tumor is in just one lobe. The anatomical lobectomy has a 68% chance of no disease after five years for early-stage NSCLC.
Segmentectomy and Wedge Resection
Segmentectomy and wedge resection cut out small lung parts. Segmentectomy removes a lobe segment, and wedge resection takes out a wedge-shaped tissue piece. They’re good for smaller tumors or when lung function is low. These methods help keep as much lung as possible.
Sleeve Resection: Preserving Lung Function
Sleeve resection takes out part of the lung and airway, then puts the rest back together. It’s good for tumors in big airways. This way, patients keep more lung function and recover better. It’s key for those having lung surgery.
Preparing for Lung Surgery
Getting ready for lung surgery involves a lot of steps to ensure everything goes well. This stage is important because it prepares you for a successful operation and healing. Knowing the tests you’ll need and making some lifestyle changes can greatly improve your experience with surgery.
Essential Tests and Evaluations
Before surgery, patients need to complete essential tests to check their health and readiness. These tests include:
- Blood tests
- Swab tests
- Electrocardiogram (ECG)
- Lung function tests
- Echocardiogram
- Chest X-ray
- Cardiopulmonary exercise test
These tests look for any issues to make sure patients are ready for surgery. Usually, these checks are done about a week before the surgery.
Quitting Smoking for Better Outcomes
Stopping smoking is key to better surgery results. It’s best to quit smoking at least four weeks before surgery. This reduces the chances of problems like infections and complications while recovering. Quitting smoking not only helps with the surgery but also boosts your overall health.
Importance of Overall Health Assessment
Checking your overall health is critical before lung surgery. This review looks at your physical condition, what you eat, and how you feel mentally. Joining programs to improve these areas can make you more ready for surgery. It’s also good to plan for taking time off work and getting someone to help you at home. Making a checklist of things to bring to the hospital, such as pajamas and toiletries, is helpful for a smooth stay.
Minimally Invasive Surgery Options
Minimally invasive surgery introduces new ways to treat non-small cell lung cancer for early-stage patients. Techniques like Video-Assisted Thoracoscopic Surgery (VATS) and Robotic-Assisted Thoracic Surgery (RATS) have big benefits over old methods.
Benefits of Video-Assisted Thoracoscopic Surgery (VATS)
VATS uses video tech for better surgical accuracy with smaller cuts. This method cuts down recovery to just two to three days. It also makes post-surgery pain much lower, helping patients get back to life faster.
Robotic-Assisted Thoracic Surgery (RATS)
RATS brings top-notch robotic tech to lung surgery. This offers better movement and seeing for the surgeon. Patients usually get better in three weeks, faster than the traditional four to six weeks. RATS causes less damage to nearby tissues, meaning less pain and speedier healing.

| Aspect | Traditional Surgery | VATS | RATS |
|---|---|---|---|
| Hospital Stay Duration | Approximately 4 days | 2-3 days | 2-3 days |
| Recovery Time | 4-6 weeks | 3 weeks | 3 weeks |
| Post-Surgery Pain Levels | Higher | Lower | Lower |
| Surgical Precision | Standard manual techniques | Video-assisted | Robotic-assisted |
VATS and RATS are great for doing needed surgeries with less trouble for patients after. These options are key for those eligible and battling non-small cell lung cancer as they evolve.
Recovery and Post-Surgery Care
Recovery is key after lung surgery for non-small cell lung cancer (NSCLC). It’s important to know what to expect during this time. Patients usually stay in the hospital for 3 to 7 days after surgery.
Expected Recovery Time
Care after surgery starts right away. Most patients start walking within 12 hours post-operation. Depending on the surgery, you might have three small or one long incision. Stitches that dissolve are often used, but some may need to be removed after about 10 days. Usually, you can go back to daily activities, like driving, in 4 to 6 weeks.
Managing Side Effects After Surgery
It’s crucial to manage side effects for a smooth recovery. Pain, tiredness, and difficulty breathing are common. Taking your prescribed medicines and doing deep breathing exercises can help. Always talk to your healthcare provider if you’re worried or see new symptoms before your next visit, usually 2 to 6 weeks after surgery.
The Role of Rehabilitation in Recovery
Rehabilitation is very important in the recovery process. Pulmonary rehab can greatly improve lung function and recovery outcomes. About 3 to 5 weeks after surgery, you might start new treatments. This is part of your care. Your mental health is just as important. The stress of diagnosis and surgery can affect your mind too.
Good care after surgery looks at both your physical and emotional health for the best results. To understand more about how surgery helps NSCLC, check out this resource.
| Post-Surgery Care Aspect | Details |
|---|---|
| Hospital Stay | 3 to 7 days |
| Initial Mobility | Walking within 12 hours |
| Driving Resumption | 4 to 6 weeks |
| Follow-Up Appointments | 2 to 6 weeks post-surgery |
| Management of Side Effects | Pain, fatigue, shortness of breath |
| Rehabilitation | Pulmonary rehab programs recommended |
Long-Term Outcomes and Prognosis
It’s crucial for patients and families to understand what to expect with non-small cell lung cancer (NSCLC). This info helps them set realistic goals and plan for health management. Outcomes depend on various factors like cancer stage, tumor traits, and patient health.
Factors Influencing Cancer Prognosis
Several factors affect a cancer patient’s outlook. These include:
- Stage of Cancer: Early-stage NSCLC (stage I) patients have a five-year survival of about 70.2%. Stage II drops to 60.21%. Stage IIIA’s outlook falls to 49.9%.
- Type of Tumor: Adenocarcinoma, making up 40% of lung cancers, grows slowly. Squamous-cell carcinoma, linked to smoking, grows faster.
- Patient Health: Age and gender also play a role in survival, with notable differences in outcomes.
- Treatment Response: A positive response to initial treatments can significantly improve a patient’s prognosis.
Adjuvant Therapy Following Surgery
Adjuvant therapy is key after surgery to boost outcomes. It can include chemotherapy and targeted therapies to lower recurrence risk. It’s advised for stages I to IIIA NSCLC to help patients live longer. Regrettably, about 40% of cases are already stage IV at diagnosis, needing intense chemotherapy. The survival then averages 8-10 months.

Understanding how long-term outcomes and prognosis factors interlink aids patients in their cancer journey. Highlighting the role of custom adjuvant therapy can elevate survival chances and life quality post-surgery.
Complementary Treatment Options
After surgery, many with non-small cell lung cancer look at other ways to heal. These extra treatments can speed up recovery and make outcomes better. Options like extra chemotherapy and radiation are popular. They work to take out any leftover cancer and lower the comeback risk.
Adjunctive Chemotherapy and Radiation Therapy
Chemotherapy is key for beating cancer. It involves several cycles where patients get drugs to attack fast-growing cancer cells. This is often done with radiation therapy. Radiation targets tumors directly. It also aims to lessen the chance that the cancer will return locally. Depending on their plan, patients might get radiation therapy a few times a week for a while.
Exploring Targeted and Immunotherapy
Lately, new treatments like targeted therapies have shown great promise. These treatments attack cancer based on its unique traits, leading to care that’s more tailored to the individual. Immunotherapy is exciting too. It boosts the immune system’s fight against cancer. For some, this means getting shots every few weeks. Adding these new approaches to standard treatments can greatly improve care for patients.
Conclusion
The battle against non-small cell lung cancer highlights the vital role of surgery. Operations like lobectomy can really improve survival rates. They also lower the chance of the cancer coming back.
It’s key to spot cancer early. This makes surgery more effective. Timely surgery is crucial in managing non-small cell lung cancer.
Techniques that make smaller cuts, like VATS and RATS, are good options too. They can make recovery quicker and cut down on surgery risks. But, using RATS might cost more and come with its own risks.
Choosing the right treatment depends on the person and the cancer. That’s why a team of experts is so important.
Working with different healthcare pros means each patient gets care that’s just for them. This is key to tackling the challenges of non-small cell lung cancer. For more info on treatment options, check out this detailed article on NSCLC treatments.