Did you know the five-year survival rate for localized non-small cell lung cancer (NSCLC) can be up to 61%? This fact highlights how key accurate lung cancer staging is. It affects treatment choices and outcomes for patients. Knowing the stages of NSCLC is vital for everyone involved.
Exact NSCLC staging guides treatment plans. It helps patients sort through their treatment options. The stages show how much the cancer has spread and what the prognosis might be. Knowing the stage of the cancer helps patients get the right treatment for their case.
In this article, you’ll learn about the key parts of lung cancer staging, including the TNM classification system. You’ll see how correct staging affects cancer care. With the latest research and resources like this article, you’ll be better prepared to face NSCLC.
Key Takeaways
- Accurate staging is critical for assessing prognosis and treatment options in NSCLC.
- The TNM system categorizes lung cancer based on its extent of spread.
- Higher TNM stage numbers indicate increased cancer advancement.
- Evolving treatment strategies are crucial due to advancements in management approaches.
- Early-stage detection significantly improves survival rates for lung cancer patients.
Understanding Lung Cancer Staging
Lung cancer staging shows how much cancer is in the body. It helps doctors choose the best treatment. They look at the tumor’s size, where it is, and if it has spread. Knowing this, doctors can plan better treatments.
Definition of Lung Cancer Staging
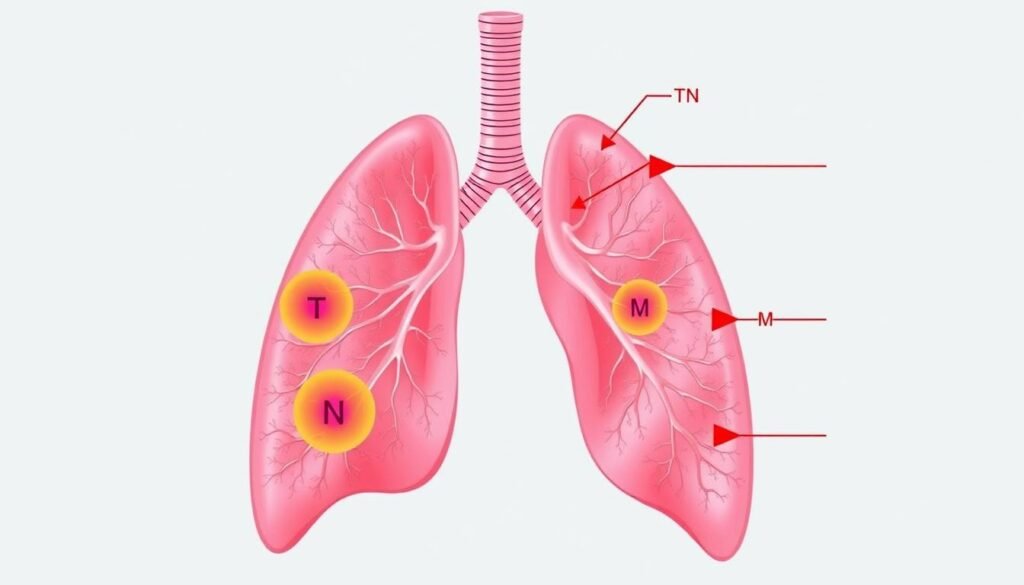
The TNM system is used for lung cancer staging. It looks at tumor size (T), lymph nodes (N), and metastasis (M). Stages range from I to IV. Each stage has more details on how far the cancer has progressed.
Importance of Accurate Staging
Getting the stage right is key for good treatment. Wrong staging can lead to the wrong treatment. This can harm survival and quality of life. Early-stage cancers have better survival rates. So, correct staging is the first step in effective treatment.
| Stage | Characteristics | Subcategories |
|---|---|---|
| Stage 0 | Cancer cells present but confined to origin | Adenocarcinoma in situ, Squamous cell carcinoma in situ |
| Stage I | Small tumors in one lung without metastasis | IA, IB |
| Stage II | Localized lung cancer possibly involving adjacent structures | IIA, IIB |
| Stage III | Spread within the chest but not to distant areas | IIIA, IIIB, IIIC |
| Stage IV | Cancer has spread to other areas far from the lungs | IVA, IVB |
What is Non-Small Cell Lung Cancer (NSCLC)?
Non-Small Cell Lung Cancer (NSCLC) is a big group of lung cancers. It makes up about 80-85% of all lung cancer cases. There are several types of NSCLC, each with its own features and ways of growing.
Overview of NSCLC Types
The primary subtypes of NSCLC include:
- Adenocarcinoma: The most common type, often found in smokers but also in non-smokers. It starts in the outer parts of the lungs.
- Squamous Cell Carcinoma: Mostly linked with smoking, it develops in the central parts of the lungs.
- Large Cell Carcinoma: It grows and spreads quickly, can start in any part of the lung, and is tough to treat.
There are also rare lung tumors, like carcinoid tumors, making up less than 5% of cases. They grow slowly compared to NSCLC. Knowing these types is vital for choosing the right diagnosis and treatment.
How NSCLC Differs from Small Cell Lung Cancer
NSCLC is the most common lung cancer, but small cell lung cancer (SCLC) is different. SCLC makes up about 10-15% of cases. It’s known for growing quickly and spreading early. Knowing the difference between NSCLC and SCLC is crucial because their treatment plans are very different.
https://www.youtube.com/watch?v=IWOzzqA3l7c
The TNM Staging System for Lung Cancer
The TNM staging system is key in handling lung cancer. It looks at tumor size (T), lymph node involvement (N), and whether the cancer has spread (M). These details are vital in deciding how to treat NSCLC.
Explanation of TNM Classification
The T category grades tumors from TX (unassessable) to T4 (large, affecting other parts). Here’s a breakdown:
- T1: Tumor ≤ 3 cm. It’s then split into T1a, T1b, and T1c, depending on size.
- T2: Tumor > 3 cm but ≤ 5 cm. It’s divided into T2a and T2b, based on which structures are involved.
- T3: Tumor > 5 cm but ≤ 7 cm or is spreading to nearby areas.
- T4: Tumor > 7 cm or significantly involves local structures.
For lymph nodes (N), the scale goes from N0 (no spread) to N3 (cancer in distant nodes). Metastasis (M) is categorized from M0 (confined to lung) to M1 (spread to other body parts).
How TNM Staging Informs Treatment Options
Knowing the TNM stage is crucial for the right NSCLC treatment approach. Treatments vary based on stage, cell type, genes, and overall health. Options include:
- Chemotherapy
- Radiotherapy
- Surgery
- Targeted drugs
- Immunotherapy
Clinical trials are vital in finding new treatments and boosting survival rates. TNM staging helps doctors tackle lung cancer more effectively.
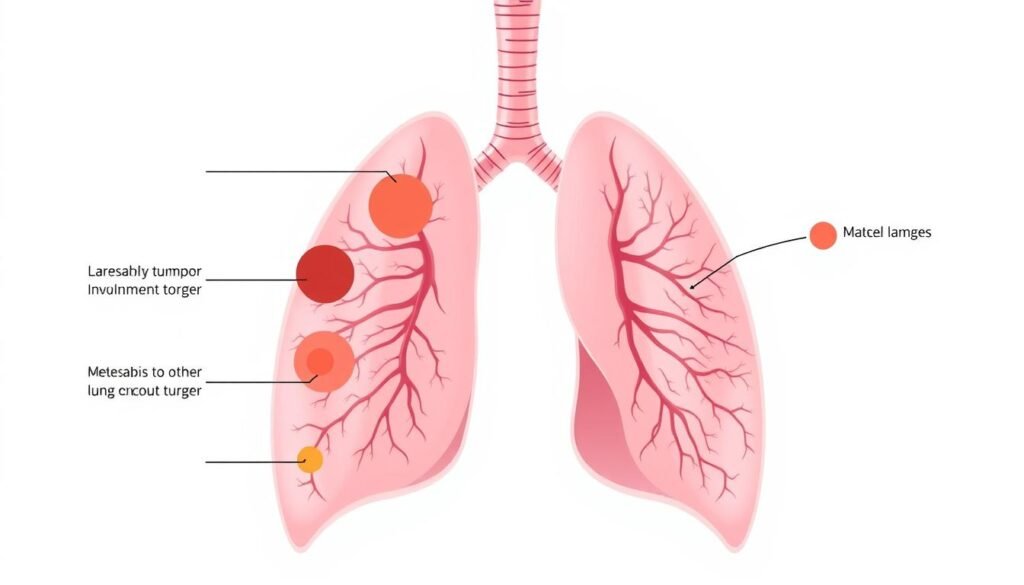
Stages of Non-Small Cell Lung Cancer
It’s important to know the stages of NSCLC for patients and doctors alike. Every stage tells us how far the cancer has grown. This guides the choice of treatment. Non-small cell lung cancer has stages from 0 to IV. Each stage has details that affect treatment choices and chances of getting better.
Detailed Breakdown of Stages 0 – IV
Lung cancer stages include:
| Stage | Characteristics | Typical Treatment |
|---|---|---|
| Stage 0 | Carcinoma in situ, where odd cells are there but haven’t spread to nearby tissue. | Surgery is usually the fix. |
| Stage I | Tumors are 4 cm or less and stay in one place, with no spread to lymph nodes. Most people can have less invasive surgery. | The surgery could be removing a lung lobe or just a small part. |
| Stage II | Tumors are mostly bigger than 4 cm or there is spread to nearby lymph nodes. | Doctors suggest surgery and chemo together. |
| Stage III | The cancer has reached further lymph nodes or big tumors are there. | Treatment might include surgery, chemo, radiation, and maybe targeted therapy. |
| Stage IV | The cancer has spread to other parts like bones or brain. Signs of advanced NSCLC are there. | Treatments like chemo and immunotherapy are used. |
Key Features of Each Stage
Understanding NSCLC stages is key for planning treatment. Stage 1 means the tumors are just in one spot, offering a good chance for surgery to work well. Stage 2 shows lymph nodes are involved, needing a stronger treatment plan. Stage 3 talks about more spread cancer, with several treatment options available. Stage 4 is tough with cancer spreading far, needing a big plan to manage it.
Staging Non-Small Cell Lung Cancer: What You Need to Know
Knowing how non-small cell lung cancer (NSCLC) is staged is key for both patients and caregivers. It involves understanding crucial details that shape treatment choices and the outlook of lung cancer. Stages range from 0 to IV, with stage IV showing the cancer has spread a lot.
The TNM system is used to stage NSCLC, looking at tumor size (T), if lymph nodes are involved (N), and if there’s metastasis (M). Each part of staging gives insights into how far the cancer has advanced. This helps doctors create personalized treatment plans. For example:
| Stage | Description |
|---|---|
| Stage 0 | Localized cancer, known as “in situ,” which has not spread. |
| Stage I | Small tumors in one lung without any lymph node or distant organ involvement. |
| Stage II | Similar to stage I but with some lymph node involvement. |
| Stage III | Cancer has spread within the chest but remains localized from distal organs. |
| Stage IV | Advanced stage indicating the cancer has metastasized to other parts of the body. |
It’s important for patients to talk with their doctors about their cancer stage. Understanding your stage helps illuminate possible treatment options and gives a clearer sense of the lung cancer prognosis. This knowledge allows patients to make informed decisions about their treatment and look for the best options.
Early Stage Lung Cancer Detection
Finding lung cancer early is key to treating it well. Catching non-small cell lung cancer (NSCLC) when it starts boosts survival chances. Knowing about lung cancer screening methods helps people get the importance of regular checks.
Methods for Early Detection
There are many ways to spot early lung cancer. Most doctors use low-dose CT scans for those at higher risk. If you’re 55 to 74 and smoked before, yearly screenings are advised. Below is a list of methods for detecting lung cancer early:
| Method | Description | Indications |
|---|---|---|
| Low-Dose CT Scan | A specialized imaging technique that exposes the patient to minimal radiation. | Recommended for high-risk groups including smokers. |
| Sputum Cytology | Analysis of mucus samples to check for cancerous cells. | Used for symptomatic patients or those at elevated risk. |
| Biopsy | Extraction of tissue samples for laboratory analysis to confirm cancer. | Essential for accurate staging and treatment planning. |
| Blood Tests | Tests to identify specific markers associated with lung cancer. | Supplemental information for diagnosis. |
Why Early Detection is Crucial
Early detection greatly boosts chances of beating lung cancer. People with stage 1 NSCLC, when found early, have about a 64 percent chance of living five more years. This shows how important quick action is. Without regular checks, many early cancers go unnoticed.
Those at risk should be extra careful. This includes smokers, people exposed to radon or asbestos, or those with a family history. Getting screened often can catch cancer early. This means you can get treatment quickly and have better results. Check out more on early stage lung cancer detection.

Advanced Stage Lung Cancer Characteristics
As non-small cell lung cancer moves to advanced stages, it is key to know the signs. In stages III and IV, patients face tough symptoms that change their lives greatly. This part talks about common NSCLC symptoms and looks into advanced lung cancer’s future.
Understanding Symptoms of Advanced NSCLC
Those with advanced lung cancer often share several worrying signs. These symptoms are important:
- Persistent cough: A cough that stays and may get worse.
- Chest pain: Pain or discomfort in the chest, varying in how severe it is.
- Unintended weight loss: Losing weight without trying, a common sign among patients.
- Shortness of breath: Hard to breathe or feeling short of breath with little effort.
- Fatigue: Feeling tired all the time, even after resting or sleeping.
These NSCLC symptoms greatly impact daily life and show a need for quick medical help.
Prognosis at Advanced Stages
The future for those with advanced lung cancer changes a lot based on the disease’s traits. Stage III non-small cell lung cancer has three parts: 3A, 3B, and 3C. Each part has different tumor sizes and affects lymph nodes differently:
| Stage | Tumor Size | Lymph Node Involvement |
|---|---|---|
| 3A | 3 cm to >7 cm | Has spread to nearby lymph nodes |
| 3B | Varies | Affects lymph nodes in several places |
| 3C | More than 5 cm | Gone to lymph nodes on the other side |
Stage IV, marked by cancer spreading far, usually has a tougher prognosis, with fewer treatment choices. The outlook relies on the patient’s health, tumor details, and how well treatment works. Even with these hurdles, treatments like surgery, chemotherapy, and immunotherapy aim to better the lives of those with advanced lung cancer.
The Role of Imaging Tests in Staging
Imaging tests are crucial for accurately staging non-small cell lung cancer (NSCLC). They determine the tumor’s size and its position relative to nearby structures. They also assess lymph node involvement and the presence of cancer in distant parts of the body.
Common Imaging Techniques Used
The most common imaging techniques for detecting lung cancer include:
- CT scans: Doctors highly recommend a CT scan of the chest with contrast for those suspected of having lung cancer. This method provides clear images, showing the tumor’s characteristics in detail.
- PET scans: Specifically used for NSCLC staging, PET scans offer vital insights into the metabolic activity of tissues. Research shows a sensitivity of 80-100% in identifying malignant lesions with FDG-PET.
- Bronchoscopy: Almost 100% accurate for tumors in the center of the chest, bronchoscopy enables doctors to see and biopsy the tumor directly.
What Information is Gathered from Imaging
The information gained from different imaging techniques greatly improves understanding of lung cancer. It provides key insights such as:
| Imaging Technique | Key Information Provided | Accuracy Level |
|---|---|---|
| CT scans | Tumor size, location, and regional lymph node involvement | High |
| PET scans | Metabolic activity of the tumor | 80-100% sensitivity |
| Bronchoscopy | Direct biopsy and visualization | Close to 100% |
Accurate imaging is key for a full understanding of lung cancer stages. It helps doctors choose the best treatment methods. The stage of cancer affects patient care and treatment options. More details on lung cancer stages are available here.
Pathological vs. Clinical Staging
It’s important to know the difference between pathological and clinical staging for NSCLC. Each type plays a role at different stages of treating lung cancer. Clinical staging happens before treatment begins. Pathological staging, however, is done after surgery to closely examine the tumor and nearby lymph nodes.
Differences Between Pathological and Clinical Staging
Pathological and clinical staging differ in what they focus on and when they happen:
| Criteria | Pathological Staging | Clinical Staging |
|---|---|---|
| Timing | Post-surgery examination | Pre-treatment assessment |
| Basis of Evaluation | Direct examination of the tumor and lymph nodes | Imaging methods and clinical findings |
| Accuracy | Generally more accurate | May vary based on imaging quality |
| Examples of Staging | Includes stages from Tis N0 M0 to T4 N3 M0 | Involves categorizations based on CT, MRI, or PET results |
When Each Type of Staging is Used
Clinical staging is key for planning the first steps of treatment. It’s used to figure out the size of lung cancer before surgery. Pathological staging comes next, after surgery. It gives detailed info on the cancer, which helps decide on more treatments.
Staging and Treatment Options Available
It’s crucial to know how staging affects treatment for non-small cell lung cancer (NSCLC). Every stage has unique features that guide us to the right therapy. This means treatments are customized based on cancer stage, matching the many lung cancer therapies out there.
How Staging Influences Treatment Plans
Knowing the exact stage of cancer is key to choosing treatments. For example, stage 0 NSCLC might only need surgery. Other options, like photodynamic therapy or brachytherapy, can also work. When it comes to stage I, surgery could be enough. This could mean removing a lobe or a smaller part.
As cancer moves forward, treatments change too. Stage II often starts with chemotherapy to reduce tumors before surgery. By stage IIIA, the plan might involve chemotherapy, radiation, and immunotherapy. This shows how treatments get more complex as the disease advances.
Current Treatments for Each Stage of NSCLC
| Stage | Treatment Options |
|---|---|
| 0 | Surgery, photodynamic therapy, brachytherapy |
| I | Surgery (lobectomy, segmentectomy), adjuvant chemotherapy/immunotherapy |
| II | Neoadjuvant chemotherapy, surgery |
| IIIA | Chemotherapy, radiation, immunotherapy, surgery |
| IIIB | Chemotherapy, radiation, immunotherapy, targeted therapy |
| IVA/B | Surgery, chemotherapy, targeted therapy, immunotherapy, radiation |
For advanced stages, like stage IV, the goal is to better life quality and prolong survival. This involves a mix of therapies, showing the importance of NSCLC treatment plans that use various methods. Clearly, understanding lung cancer’s stages is vital for effective treatments.
Conclusion
Staging NSCLC is key for effective treatment and better outcomes. Each stage of non-small cell lung cancer has its own traits. These impact prognosis and guide the management plan. For example, stage I NSCLC patients might see a 60-80% survival rate after surgery. This shows why catching lung cancer early is so vital.
The accuracy of clinical staging is crucial in deciding on treatments. Accuracy often sits between 50-60%. It’s vital for doctors and patients to talk about clinical and pathological stages. This boosts lung cancer awareness and helps patients make educated choices about their treatment.
It’s important for patients and doctors to talk openly about lung cancer staging. Understanding the factors that impact prognosis and treatment helps improve patient outcomes. It also raises awareness about lung cancer control. Conversations like these are key to personalized care and better survival rates for lung cancer patients.