Did you know lung cancer causes over 1 million deaths around the world yearly? It’s the reason for 31% of all cancer deaths in U.S. men and 26% in women. Smoking is the main cause, linked to 80% of these deaths. Smokers face a risk up to 30 times higher of getting this disease than non-smokers. We will explore how smoking and lung cancer are connected. We’ll also look at the risks of smoking and the need for prevention strategies.
Key Takeaways
- Lung cancer causes over 1 million deaths globally each year.
- Approximately 80% of lung cancer deaths in the U.S. are linked to smoking.
- Smokers have a 30-fold increased risk of lung cancer compared to non-smokers.
- Lung cancer accounts for a significant proportion of cancer-related fatalities in both men and women.
- The majority of lung cancer diagnoses occur in former smokers.
- Effective prevention and cessation strategies are crucial to reducing lung cancer risks.
The Prevalence of Lung Cancer in the United States
Lung cancer is a major health issue in the United States. It causes about 31% of cancer deaths in men and 26% in women. The disease leads to over 160,000 deaths each year.
Smoking is deeply linked to lung cancer deaths. It causes 80% to 90% of them. Smokers are 15 to 30 times more likely to get lung cancer than non-smokers.
Quitting smoking can greatly lower your risk. Secondhand smoke and environmental hazards like radon also increase risk. These dangers are significant for non-smokers too.
To fight lung cancer effectively, understanding its impact is crucial. It’s a top cause of cancer deaths. Better prevention and treatment are key goals for public health.
| Risk Factors | Impact on Lung Cancer |
|---|---|
| Cigarette Smoking | 80% to 90% of lung cancer deaths |
| Secondhand Smoke | Increases lung cancer risk in non-smokers |
| Indoor Radon Exposure | Important cause of lung cancer |
| Occupational Exposure (Asbestos, Arsenic) | Elevated lung cancer risk |
| Previous Radiation Therapy | Increases lung cancer risk in survivors |
The Relationship Between Smoking and the Development of Lung Cancer
The link between smoking and lung cancer is strong and varied. Many studies show that smoking causes lung cancer. This is mainly due to tobacco smoke. Over 80% of lung cancer deaths come from using tobacco. This makes it the main risk. These facts show the clear link between smoking and the increase in lung cancer worldwide.
Statistical Evidence Linking Smoking to Lung Cancer
Studies on animals and humans show smoking causes lung cancer. For instance, in South Korea, the National Health Insurance Service sued tobacco companies. This was after paying many patients who smoked a lot and got certain lung cancer types. This shows how smoking seriously ups the risk of serious health issues.
Understanding Carcinogens in Tobacco Smoke
Tobacco smoke has many carcinogens that kick start genetic changes, often leading to cancer in lung tissues. Carcinogens like polycyclic aromatic hydrocarbons and nitrosamines are key in this. They cause inflammation, which helps lung cancer develop. It’s key to know these risks as they help us understand the big health effects of smoking.
https://www.youtube.com/watch?v=ihCnDjyJv5c
| Type of Cancer | Associated Smoking History | Percentage of Lung Cancer Cases |
|---|---|---|
| Small Cell Lung Cancer | 20 pack-years | Varies; significant correlation |
| Squamous Cell Lung Cancer | 30 years of smoking | High prevalence among smokers |
| Non-Smokers with Lung Cancer | No smoking history | Emerging evidence of risk factors |
How Smoking Causes Genetic Changes
Smoking is key in changing our genes, which affects lung cancer. The bad stuff in tobacco creates major DNA changes. This can lead to mutations making lung cancer more likely. Knowing this helps us understand smoking’s dire effects on our health.
Effects of Tobacco Carcinogens on DNA
Tobacco smoke has many substances that harm DNA. Studies show these can cause DNA lesions, leading to cancer. Smokers, especially those with a lot of DNA damage, face higher cancer risks.
For example, smokers with moderate DNA damage have a 2.37 times higher lung cancer risk than nonsmokers. This shows how tobacco changes genetics in significant ways.
Inflammation and its Role in Lung Cancer Development
Inflammation from smoking is a big factor in lung cancer. The body’s defense against smoke can worsen lung cell damage. This can cause cancer.
Long-term smoking inflammation can lead to cell changes and unstable lung tissue. This highlights inflammation’s role in lung cancer. To learn more, see details on how genes and smoking affect the lung.
The Impact of Nicotine Addiction
Nicotine addiction makes it hard for people to stop smoking. This addiction keeps people hooked on tobacco. They face many health challenges.
Understanding Nicotine’s Role in Continued Smoking
Nicotine makes the brain release chemicals that feel good. Smoking quickly gets nicotine to the brain, making people want to keep smoking. A lot of lung cancer comes from this addiction. It keeps people wanting more nicotine.
Studies show 59.5% of smokers with lung cancer find it hard to quit. This shows how strong nicotine addiction can be.
Sociocultural Factors Influencing Smoking Habits
Smoking is also shaped by society and culture. Peer pressure, what we see in media, and social norms play big roles. These factors start and keep smoking habits going. Especially in young people, making quitting even harder.

Nicotine addiction and lung cancer are closely linked. Community support is very important. It helps fight against nicotine addiction by changing societal views.
| Factor | Influence on Smoking Behavior |
|---|---|
| Peer Pressure | Increases likelihood of starting and continuing smoking |
| Media Exposure | Normalizes smoking, particularly among youth |
| Social Norms | Shapes perception of smoking as acceptable behavior |
| Accessibility | Easy access to tobacco products encourages use |
Secondhand Smoke Exposure and Lung Cancer Risks
Secondhand smoke is very harmful, especially for people who don’t smoke. Being around it can raise your chances of getting lung cancer by up to 30%. This risk is even higher if you’re around smoke both at home and at work. It’s worse for those exposed before 25 years old, as early exposure is linked to a greater risk of lung cancer later.
How Secondhand Smoke Affects Non-Smokers
Many studies have looked at how secondhand smoke impacts non-smokers. They found that non-smokers who were around secondhand smoke when they were young are more likely to get lung cancer. The data shows a clear increase in risk:
- Overall lung cancer risk for never smokers exposed to secondhand smoke: 1.31 (95% CI: 1.17–1.45)
- Adenocarcinoma risk: 1.26 (95% CI: 1.10–1.44)
- Small cell lung cancer risk: 3.09 (95% CI: 1.62–5.89)
- Increased risk for women married to smokers: 20%
- Increased risk for men married to smokers: 30%
To deal with this, we need strong tobacco control policies. This will help reduce exposure to secondhand smoke.
Legislation and Policies Against Secondhand Smoke
Many places have made rules to control secondhand smoke because of its dangers. These rules are designed to limit smoking in public places. This protects people who don’t smoke from secondhand smoke. Important steps include:
- Designated non-smoking areas
- Prohibitions in workplaces
- Public awareness campaigns
These efforts are all about keeping the public healthy and more aware of secondhand smoke’s risks. We must keep pushing for these rules to be enforced strictly. This way, we can lower the risks of lung cancer from secondhand smoke.
Smoking Cessation Programs and Their Importance
Smoking cessation programs are key for people wanting to quit tobacco use. They significantly lower lung cancer risks. These programs help smokers quit and better their life quality. By looking into various programs and their success, people can choose the best way to get healthier.
Types of Smoking Cessation Programs Available
Different programs meet various needs and likes. These include:
- Counseling and Support Groups: They give support and motivation to quit smoking.
- Pharmacotherapy: This includes nicotine patches and gums, along with prescription drugs to fight tobacco addiction.
- Online Programs: These offer easy and flexible ways to learn quitting techniques at one’s pace.
- Comprehensive Programs: Mixing behavioral therapy with drug treatments often leads to higher success in quitting.
Success Rates of Different Cessation Methods
How well quitting programs work varies a lot by method:
| Method | Quit Smoking Success Rate |
|---|---|
| Counseling | 20-30% |
| Nicotine Replacement Therapy | 20-35% |
| Prescription Medications | 30-50% |
| Combination Therapy | 55-70% |
Mixing different methods increases chances of quitting. Notably, quitting before lung surgery saves costs and improves survival and life quality.

Lung Cancer Screening: Importance and Methods
Lung cancer screening is vital, especially for those at high risk like smokers. Early detection through screening methods boosts survival chances. This is because finding cancer early is key to successful treatment.
Recommended Screening Guidelines for Smokers
The American Cancer Society recommends a yearly lung cancer screening. This is for people 50 to 80 years old who have smoked a lot over the years. “Pack-year” measures how much someone has smoked. For instance, smoking a pack a day for 20 years equals 20 pack-years.
Screening is also suggested for those who quit smoking over 15 years ago. It’s important to catch cancer early to save lives, even long after stopping smoking.
How Early Detection Improves Survival Rates
Finding lung cancer early greatly improves the chances of survival. People found to have lung cancer early fare much better than those found later. Big studies have shown screening can really reduce death rates.
Screening has been proven to save lives, especially when smokers stop smoking too. Studies have shown combining both can lead to even fewer deaths. With lung cancer being a top cause of cancer deaths, following screening guidelines matters more than ever.
| Screening Population | Age Range | Pack-Year History |
|---|---|---|
| Current Smokers | 50-80 Years | ≥ 20 Pack-Years |
| Former Smokers | 50-80 Years | ≥ 20 Pack-Years & Quit > 15 Years |
Lung Cancer Staging: Understanding the Severity
Lung cancer staging is key in understanding how serious the disease is. It affects which treatments patients can get. Knowing about lung cancer staging helps doctors decide on the best way to manage it. This can change the outcome for people with this disease.
The Staging Process Explained
Staging looks at where the cancer is, how big the tumors are, and if it’s spread. Doctors use tests like scans and biopsies to figure this out. For a type called non-small cell lung cancer, stages go from 0 to IV. Stage 0 is early disease. Stage IV is very advanced. Another kind, small cell lung cancer, is either “limited” or “extensive.” “Limited” means it’s just in one lung. “Extensive” means it has spread more widely.
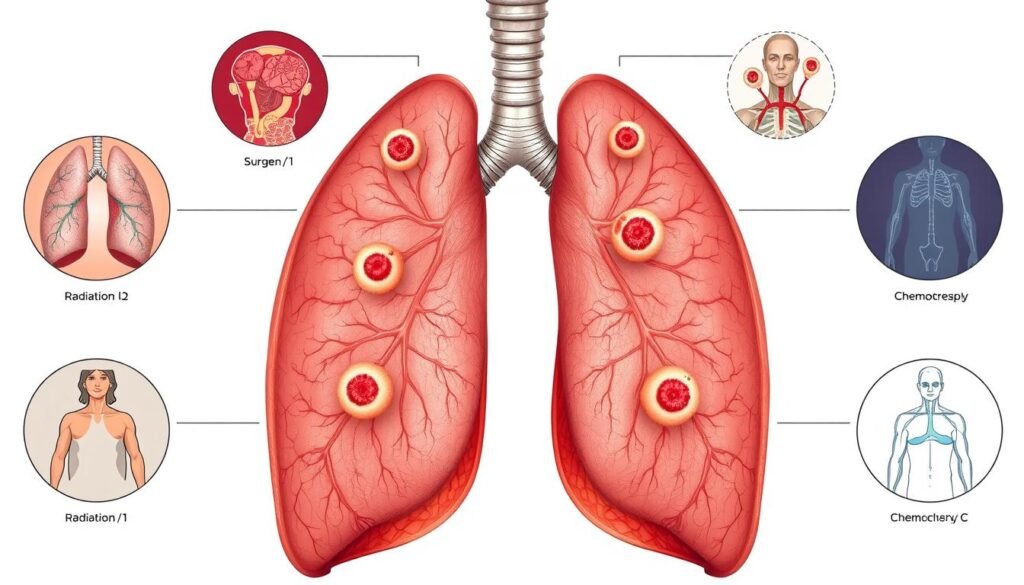
How Staging Affects Treatment Options
Knowing the lung cancer stage helps doctors pick the right treatment. The kind of treatment depends on the lung cancer type and its stage. Early-stage cases might need surgery. More advanced stages could require chemotherapy, radiation, or targeted therapies. This staging also plays a role in predicting how well treatments might work. It leads to better care for patients.
Current Lung Cancer Treatment Options
Lung cancer treatments depend on the type and stage of the cancer. Key options include surgery, radiation therapy, and chemotherapy. With medical advancements, patients now have better chances thanks to new tech and research.
Overview of Surgery, Radiation, and Chemotherapy
Surgery is very important, especially for early-stage non-small cell lung cancer (NSCLC). For example, surgery alone can often cure stage 0 NSCLC. There’s no need for chemotherapy or radiation. But for stage IIIA NSCLC, doctors typically use a mix of surgery, chemotherapy, and radiation.
Stage II cancer might get chemotherapy before surgery to improve results. Chemotherapy can be the first step for treating stage I NSCLC. It helps lower the risk of the cancer coming back. For stage IIIB NSCLC, chemotherapy with radiation therapy is common. Health decides the treatment plan. The chance of living five more years can be as high as 63% for those caught early.
Biological Therapy and Emerging Treatments
Biological therapy is now a key part of some treatment plans. It boosts the immune system to better fight cancer. Targeted therapies, like ones focusing on the EGFR gene, are hopeful. Drugs like osimertinib (Tagrisso) and lorlatinib (Lorbrena) are doing well against advanced lung cancer.
Those with advanced lung cancer should look into clinical trials. They offer new biological therapies. Studies show immunotherapies can work well with chemotherapy or other treatments. For symptom relief, treatments like laser therapy might help.
For more on how smoking affects lung cancer treatment, check out this resource.
| Stage | Treatment Options | Survival Rate |
|---|---|---|
| Stage 0 | Surgery | High |
| Stage I | Surgery, Chemotherapy, Immunotherapy | 63% |
| Stage II | Neoadjuvant Chemotherapy, Surgery | Varies |
| Stage IIIA | Surgery, Radiation, Chemotherapy | 35% |
| Stage IV | Combination of Surgery, Chemotherapy, Targeted Therapy | 8% |
Smoking Prevention Campaigns: A Necessity
Smoking prevention campaigns are key in fighting tobacco use and lung cancer. They help us understand what works and what doesn’t in stopping smoking. These efforts are crucial for building a health-conscious society aware of smoking’s dangers.
Evaluating the Effectiveness of Current Campaigns
Today’s campaigns against tobacco use various strategies. We look at smoking rates and how people engage with these campaigns to see if they’re working. They mostly educate on smoking’s dangers, including its connection to lung cancer. For example, the Cancer Center Cessation Initiative (C3I) has helped over 50,000 cancer patients try to quit smoking.
However, about half of non-small cell lung cancer (NSCLC) patients still smoke after diagnosis. This shows we have more work to do.
Engaging the Community in Tobacco Prevention
Getting communities involved is vital for smoking prevention. Health organizations, schools, and local communities working together can make a big difference. These efforts not only spread awareness but also give people the tools to stop smoking. When communities unite, they create a supportive atmosphere that celebrates quitting smoking.
A study found that 75% of patients who quit smoking were still alive three years later. This shows the power of community in saving lives through smoking cessation.
| Outcome | Patients Who Quit Smoking | Patients Who Continued Smoking |
|---|---|---|
| Median survival (months) | 66 (22 months longer) | 48 |
| Time before disease progression (years) | 5.7 | 3.9 |
| Alive after 3 years | 75% | 66% |
| Alive after 5 years | 61% | 49% |
Merging community engagement with tobacco prevention campaigns is key. The joint work of health experts and local groups can boost campaign success. This can lead to less smoking and better public health. For more on early detection and its importance, visit lung cancer screening guidelines.
Conclusion
It’s key to grasp how smoking leads to lung cancer for effective health strategies. Tobacco is behind about 90% of these cases. This shows we need focused efforts to cut down smoking.
Studies show that smoking a lot can greatly increase lung cancer risk. If you smoke heavily, your risk could go up by 17.89 times. Stopping smoking could prevent nearly 76.4% of lung cancer cases.
Adding genetic factors to smoking habits helps find those at higher risk. There’s new research on genes linked to nicotine addiction. This could lead to more tailored ways to prevent lung cancer.
We must work to remove the shame of smoking and promote quitting programs. Health drives need the latest research, like what you’ll find in this study. This will help prioritize preventing lung cancer.
By working together and using informed policies, we can lower lung cancer rates. This will improve health and wellbeing in our communities.