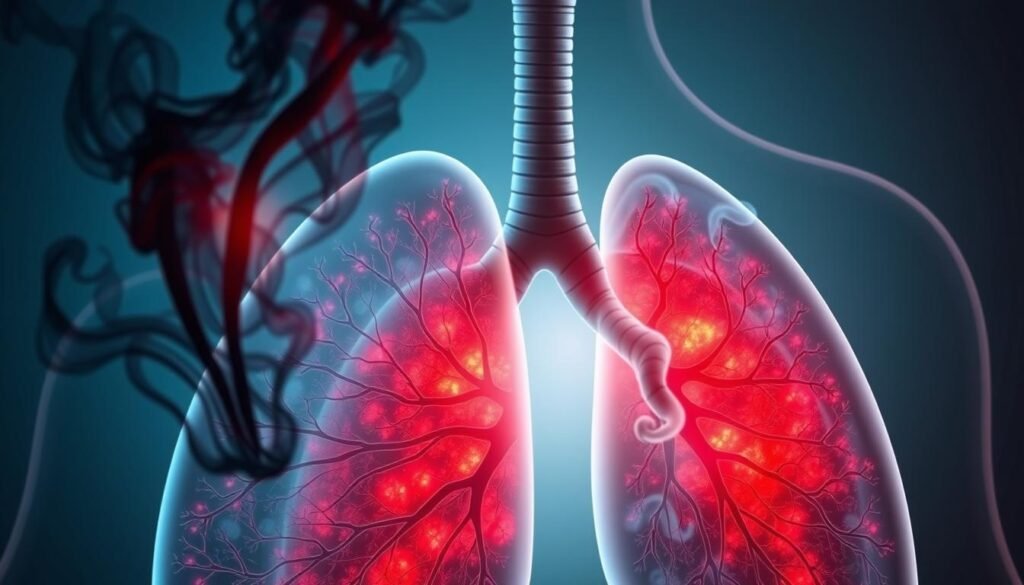
Every year, lung cancer takes over 1 million lives around the world. It’s the top cause of cancer deaths. Shockingly, smoking is behind 90% of lung cancer cases in men and 70-80% in women. This fact clearly shows how smoking and lung cancer are linked. Smokers have a risk of getting lung cancer that’s up to 30 times higher than non-smokers.
The harmful substances in tobacco smoke are major culprits in lung cancer. They cause chronic inflammation. This doesn’t just hurt the lungs. It also works with our genes and changes them in ways that boost the risk of cancer. For deeper insights, check out information on lung cancer risk factors.
Key Takeaways
- Lung cancer is the leading cause of cancer deaths globally.
- Approximately 90% of lung cancer cases in men are linked to smoking.
- Smokers are at a 30-fold greater risk of lung cancer compared to non-smokers.
- Tobacco smoke contains numerous carcinogens, including over 60 known cancer-causing agents.
- Chronic inflammation from smoking contributes to tumor progression and increases lung cancer risk.
- Quitting smoking can significantly lower the chances of developing lung cancer.
- Exposure to secondhand smoke is a significant risk factor for lung cancer.
Understanding Lung Cancer
Lung cancer is a major cause of cancer deaths worldwide. There are two main types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Both types have different features but are often linked to the same causes. Smoking is the biggest cause of lung cancer.
Small cell lung cancer is common among heavy smokers. Smoking damages lung tissue, which can lead to cancer. The more someone smokes, the higher the risk. Secondhand smoke also increases the risk. It’s important to think about the air quality around smokers.
Genes and age play a role in lung cancer risks. A family history of cancer increases your chances. Being exposed to things like radon and asbestos, especially at work, can cause lung cancer too. It’s good to check your home for radon, especially in areas where it’s common.
Living a healthy lifestyle can help lower your lung cancer risk. Eating lots of fruits and veggies and staying active are both beneficial. Knowing these tips is key to keeping yourself healthy and reducing cancer risks.
| Risk Factor | Impact on Lung Cancer |
|---|---|
| Smoking | Primary cause of lung cancer, affects lung tissue |
| Secondhand Smoke | Increases risk for non-smokers significantly |
| Genetic Factors | Family history raises likelihood of disease |
| Environmental Exposure | Radon and asbestos linked to higher risks |
| Diet | Healthy foods may lower risk |
| Physical Activity | Regular exercise linked to reduced risk |
Statistics of Lung Cancer in the United States
Lung cancer is a major health issue in the US. It is the top cause of cancer deaths. Annually, over 160,000 people die from it. This number is about 31% of all cancer deaths in men and 26% in women.
Projections estimate about 234,580 new cases of lung cancer in 2024. This shows the growing concern over lung cancer rates.
The five-year survival rate for lung cancer patients is about 15%. This low rate highlights the need for better prevention and early detection. Studies show that cigarette smoking causes 80% to 90% of lung cancer cases. Smokers have up to a 30 times higher risk of developing lung cancer than non-smokers.
Radon and secondhand smoke also increase lung cancer risk. Up to 20% of lung cancer cases are in people who never smoked. The risk of lung cancer in never smokers is around 1.8% for males and 1.3% for females. This risk is much higher in current and former smokers. For example, former smokers have a 7.2% risk (men) and 5.8% (women). Current smokers have a 14.8% risk (men) and 11.2% risk (women).
There are efforts to improve early detection through advanced CT screenings. These screenings are key for better outcomes, particularly in those with a heavy smoking history. They could be life-saving for people between 50 to 80 years old.
Raising awareness can lead to improved prevention and treatment. For more info on lung cancer and quitting smoking, please visit this resource. Also, learn about early detection at this link.
How Smoking Contributes to Lung Cancer Development
Understanding how smoking leads to lung cancer is key. Tobacco smoke is packed with harmful stuff, like cancer-causing substances. These bad actors can mess up the DNA in lung cells. This causes changes that can lead to cancer.
Impact of Tobacco Carcinogens
Tobacco carcinogens are big players in lung cancer development. They harm the DNA in lung cells, leading to mutations. Studies show that men who smoke are 23 times more at risk than nonsmokers. The danger smoking poses to lung health is enormous. For deeper insights, consider diving into research by experts.
Disease Progression in Smokers
Smoking makes lung cancer get worse because of chronic inflammation. Smokers may face diseases like COPD, which brings more inflammation. This situation worsens DNA damage, encourages tumor growth, and speeds up cancer. Smoking’s link to lung cancer is strong, causing about one in every three cancer deaths in the US. This fact underlines the importance of fighting smoking.
| Factor | Impact on Lung Cancer |
|---|---|
| Tobacco Carcinogens | Induce genetic mutations and increase cancer risk |
| Inflammation | Promotes ongoing DNA damage and tumor growth |
| COPD | Linked to elevated cancer risk and disease progression |
The Role of Chronic Inflammation in Lung Cancer
Chronic inflammation is a key factor in the risk of lung cancer. The link between inflammation and cancer is complex and includes conditions that can either advance or halt disease growth. Studies show that lung inflammation can lead to lung cancer, highlighting the need to understand inflammation’s role in this process.
Inflammatory Conditions and Cancer Risk
Long-term inflammation, from diseases like COPD or asthma, increases lung cancer risk. High levels of certain proteins, like interleukin (IL)-1β, make cells grow uncontrollably and avoid death. This can turn healthy cells into cancerous ones. Research from the PLCO trial shows that high C-reactive protein (CRP) levels also raise lung cancer risk.
Knowing how chronic inflammation leads to lung cancer could help find new prevention methods. Inflammation affects the tumor’s environment, which may improve treatment options. With inflammation’s critical role in lung cancer, focusing on how to manage it could bring new ways to fight the disease. For more information on how allergies affect lung cancer, visit this link.
| Inflammatory Markers | Association with Lung Cancer Risk |
|---|---|
| C-Reactive Protein (CRP) | Positive correlation with increased lung cancer risk |
| Interleukin (IL)-1β | Increases cellular proliferation; linked to cancer promotion |
| ROS Levels | Impairment in cell function; facilitates inflammatory processes |
| Chronic Infection Markers | Elevation suggests increased susceptibility to lung cancer |
Cellular Mutations and DNA Damage
Smoking significantly speeds up DNA damage in lung cells. This is a key step towards getting lung cancer. Tobacco smoke is full of harmful compounds that cause cellular mutations. They also change our genes. Smokers who go through a pack a day face about 150 extra mutations in each lung cell every year. This fact shows the terrible effects of smoking at the cellular level.
Moreover, smoking’s role in DNA damage raises the chance of lung cancer. Studies show that smokers with a lot of DNA damage are greatly at risk. They have much higher chances of getting lung cancer. Specifically, those with serious DNA damage face nearly 4 times the risk compared to those with less damage.
Smoking changes important genes, like the p53 gene which helps control cell growth. When this gene mutates, cells can grow wildly. This shows how smoking-induced DNA damage leads to a series of changes. These eventually result in lung cancer.
Secondhand Smoke Risks
Secondhand smoke is harmful to people who don’t smoke. It has many dangerous substances that cause serious health problems like lung cancer. Knowing the risks of secondhand smoke is key to improve public health.
Health Implications for Non-Smokers
Non-smokers exposed to secondhand smoke are more likely to get lung cancer. Studies show secondhand smoke causes over 7,300 lung cancer deaths each year in the U.S. These numbers show a worrying truth:
| Health Impact | Statistics |
|---|---|
| Premature deaths from heart disease | 34,000 annually |
| Increased risk of lung cancer | 20-30% |
| Coronary heart disease risk increase | 25-30% |
| Stroke risk increase | 20-30% |
Secondhand smoke’s risks don’t stop at lung cancer. It’s linked to heart disease and stroke, increasing danger for those exposed. Kids and babies end up with health issues, like infections and sudden death. The need for public health actions and awareness is clear.

Benefits of Smoking Cessation
Quitting smoking brings many health benefits, especially against lung cancer. It boosts overall health and well-being. The benefits are both immediate and long-lasting.
Physical Recovery and Reduced Cancer Risk
Stopping smoking starts positive changes in the body. Those who quit see better lung function and less lung cancer risk. It shows the deep value of quitting beyond just breaking a habit.
Studies show survival rates differ among current, former, and never smokers with lung cancer. The stats show:
| Group | Death Rate |
|---|---|
| Current Smokers | 79% |
| Former Smokers | 67% |
| Never Smokers | 60% |
Smoking during cancer treatment leads to worse outcomes. The more time since quitting before a lung cancer diagnosis, the better the survival chances.
Quitting smoking doesn’t just improve personal health. It also reduces surgery complications for lung cancer patients, enhancing their life quality. Quitting even after a lung cancer diagnosis shows it’s always a good time for better health through smoking cessation.
Lung Cancer Prevention Strategies
Lung cancer prevention combines lifestyle changes and community efforts. Health campaigns are key, lowering smoking rates and spreading the word on smoking’s dangers. They educate on the risks of tobacco and secondhand smoke, helping prevent lung cancer.
Public Health Campaigns
Anti-smoking campaigns have cut down smoking, which leads to 87% of lung cancer cases in the U.S. Smokers face a lung cancer risk 20 times higher than non-smokers. These campaigns fight smoking and highlight the risks of secondhand smoke and radon.
Effective health campaigns have lowered lung cancer rates. Quitting smoking can cut lung cancer risk by 30% to 60% after 10 years. The American Cancer Society pushes for ongoing public health support. For more on how to prevent lung cancer, check out this resource.

| Prevention Strategy | Description | Impact on Lung Cancer Risk |
|---|---|---|
| Smoking Cessation | Quitting smoking significantly lowers lung cancer risk. | Decreased risk by 30% to 60% after 10 years. |
| Avoiding Secondhand Smoke | Reducing exposure to secondhand smoke protects non-smokers. | Lower risk in non-smokers. |
| Healthy Diet | Consuming fruits and vegetables enhances lung health. | Antioxidants can help protect against lung cancer. |
| Radon Testing | Testing homes for radon can identify dangerous levels. | Reduces the likelihood of lung cancer related to radon exposure. |
The Importance of Early Detection
Spotting lung cancer early can make a big difference in survival rates. A key method for this is the low-dose computed tomography (LDCT) scan. It helps find lung cancer when it’s still small. This early discovery lets doctors start treatment sooner, which can be more effective.
The American Cancer Society suggests yearly LDCT scans for people 50 to 80 years old who have smoked a lot. This screening can reduce the risk of dying from lung cancer by finding it early. But, chest x-rays are not as good at saving lives from lung cancer.
Still, LDCT screening isn’t perfect. It might miss some lung cancers, or find them late. Also, LDCT uses a bit of radiation. So, it’s important to be careful and think about the need for more tests. Screenings should be done by skilled people in accredited places for the best results.
But remember, stopping smoking is still the best way to fight lung cancer. Medicare and many insurance plans will pay for lung cancer screening. This makes it easier for those who need it to get screened.
Conclusion
The link between smoking and lung cancer is very clear. Many studies show that smoking leads to biological changes, raising lung cancer risks. This is especially true for people with certain genetic changes, like the 15q24 spot.
Smokers with this genetic change have a 30% to 80% higher chance of getting lung cancer. This fact shows how important it is to stop smoking and be aware of our health. Smoking is behind more than 30% of all cancer deaths, so it’s crucial to tackle this problem.
To fight lung cancer, it’s vital to have strong prevention campaigns. These campaigns should teach people about the dangers of smoking and secondhand smoke. Despite these efforts, over 60% of cancer patients used to smoke or still do. This fact shows the struggle to quit smoking, even after a diagnosis.
In the end, raising health awareness and having good programs to help people quit smoking can lower lung cancer rates. Making smart choices and backing preventive efforts can help battle diseases caused by smoking. Ongoing public health support is key to a healthier future.