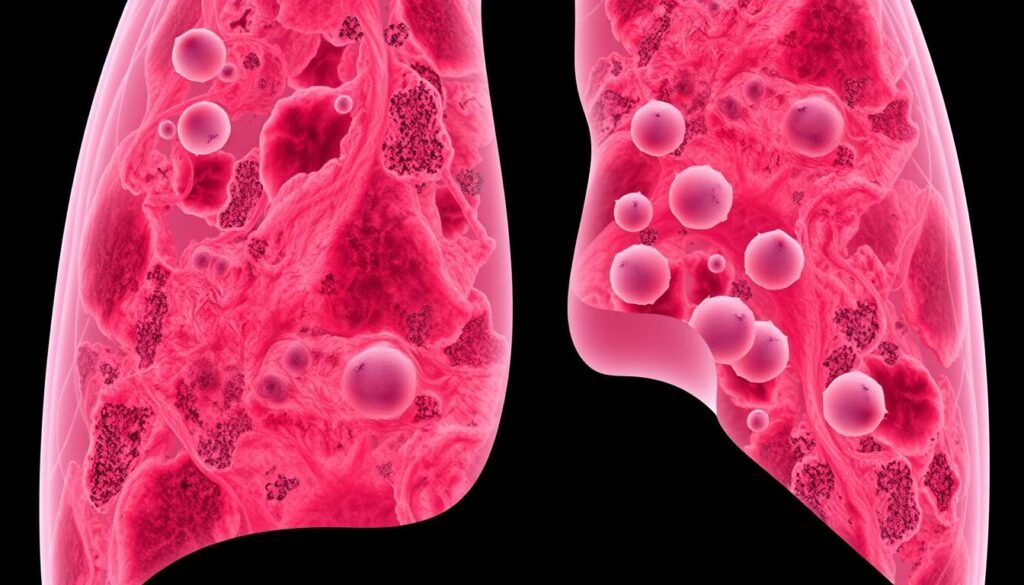
About 30% of lung cancer patients have signs of pulmonary scarring. This fact suggests a strong link that may change what we know about lung cancer risk. The role of scarring and inflammation is critical in lung cancer development. These changes make the lungs a place where cancer can start. Studies have shown that lung scarring from conditions like fibrosis is closely related to lung cancer. We need to look more into how inflammation can lead to cancer.
Scarring seen in chest X-rays is often connected to a higher risk of lung cancer, especially if the scar is on the same side as the cancer. This link stays over time, showing the importance of understanding it in chronic lung diseases. The interaction between scarring and inflammation can lead to cancer in the lungs. Recent studies offer in-depth analysis on this. They show why it’s vital to consider these factors for preventing and treating lung cancer effectively.
Key Takeaways
- 29.2% of lung cancer patients show evidence of pulmonary scarring.
- The prevalence of scarring is higher among male patients compared to females.
- Smoking is closely associated with the presence of scarring in lung cancer patients.
- Scarring is often found in the same lobe as the primary tumor, suggesting a direct relationship.
- Understanding the impact of fibrosis on cancer progression is crucial for effective treatment strategies.
Introduction to Lung Cancer Risks
Lung cancer is a major health issue, leading in cancer deaths in America. It’s crucial to know the risks for prevention and early spotting. Smoking is a big risk factor, closely tied to lung diseases. The substances in cigarettes change cells, increasing cancer risk.
Environmental exposure also raises risks. Being around pollutants, radon, and asbestos makes lung cancer more likely. People with existing lung conditions like COPD face higher risks. These diseases change lung structure and function.
In 2010, around 239,320 new lung cancer cases were reported in the U.S. This shows the importance of understanding risks. Early detection is key but can be tricky since lung cancer is often diagnosed late. This makes treatment harder and lowers the chances of survival.
To fight lung cancer, we need multiple strategies. Stopping smoking, staying informed about environmental hazards, and managing lung diseases can help. These steps can lead to better lung cancer outcomes.
Understanding Pulmonary Fibrosis
Pulmonary fibrosis causes lung tissue to scar and thicken. This makes gas exchange in the lungs hard. People with this condition might feel short of breath, have a constant cough, and feel tired often. These symptoms can make life harder. Knowing about pulmonary fibrosis is key because it can lead to lung cancer.
What is Pulmonary Fibrosis?
Pulmonary fibrosis is a disease that scars the lungs and gets worse over time. It can happen for many reasons, but sometimes, doctors don’t know why. Usually, it affects older adults, but kids can get it too. Scarring in the lungs can cause high blood pressure in the lungs and respiratory failure. These issues might lead to lung cancer and other serious lung problems.
Causes of Pulmonary Fibrosis
Different things can cause pulmonary fibrosis, like working in mining, farming, or construction. In these jobs, people breathe in harmful stuff like asbestos and silica dust. Smoking is also bad for the lungs. Moreover, certain medicines, like those for cancer or inflammation, can hurt lung tissue. This can make pulmonary fibrosis worse.
- Common causes include:
- Environmental pollutants
- Occupational exposures
- Radiation therapy
- Cigarette smoking
- Genetic predisposition
- Often, the exact cause of idiopathic pulmonary fibrosis is not known.
- Some families have genetic mutations. This makes pulmonary fibrosis affect both kids and adults in these families.
- Issues like GERD can also lead to idiopathic pulmonary fibrosis.
It’s important to understand what causes pulmonary fibrosis. This helps identify people at risk of serious conditions, including lung cancer. For more on how allergies affect lung cancer risk, check out this resource.
The Link Between Chronic Obstructive Pulmonary Disease and Lung Cancer
Chronic Obstructive Pulmonary Disease (COPD) increases the risk for lung cancer significantly. The ongoing inflammation from COPD damages lung tissue. This damage makes it easier for lung cancer to start.
Many studies show that the link between COPD and lung cancer involves complex cell actions. These actions harm tissue and its repair process, paving the way for cancer.
Research highlights concerning facts about lung health. Lung cancer is the top killer among cancers worldwide, with only a 16% survival rate over five years. Smokers are at a much higher risk. In fact, 50% of smokers shorten their lives due to smoking.
Just one cigarette can cut 11 minutes off your life. This shows how harmful tobacco is to our health.
In the US, between 2000 and 2004, smoking-related diseases like lung cancer and COPD claimed around 443,000 adult lives. Having COPD not only affects breathing but also increases lung cancer risk significantly. There’s a 17.2% chance for men who smoke to get lung cancer and 11.6% for women.
The strong link between COPD and lung cancer highlights the need for prevention. If you have symptoms like a chronic cough or breathing issues, check them out. Managing COPD well can lower lung cancer risk. Being proactive in caring for your lungs can protect you in the long run.
| Health Metric | Statistics |
|---|---|
| Lung Cancer Survival Rate | 16% |
| Smokers’ Lifetime Risk of Lung Cancer (Males) | 17.2% |
| Smokers’ Lifetime Risk of Lung Cancer (Females) | 11.6% |
| Smoking-Related Deaths (2000-2004) | 443,000 |
| Average Life Reduction per Cigarette | 11 minutes |
| COPD’s Global Rank in Causes of Death (2010) | 3rd |
The Role of Scarring and Inflammation in Lung Cancer Development
Scarring and inflammation play key roles in lung cancer. They impact how the disease grows. Conditions like pulmonary tuberculosis (PTB) lead to scar tissue. This is found in about 75% of lung cancer cases linked to scarring. Those with a history of PTB face a higher cancer risk. Around 3% of them get lung cancer later on. This shows how scarring makes one more prone to cancer.
Scar tissue changes the lung’s structure. This makes areas where cancer cells can grow. Scar carcinoma, which is especially rare, often happens to men. It is mainly linked with adenocarcinoma, often in the lung’s upper part. Incredibly, 72% of scar carcinoma cases are adenocarcinomas. Additionally, 15% of these cases are peripheral lung cancers. Also, 45% of peripheral lung cancers come from scar tissue.
Studies show people with lung scars are 1.8 times more likely to get lung cancer. Those without scars are less at risk. Interestingly, people with PTB who get lung cancer have a higher death rate. This stress the big effect lung scarring has on health. The reasons behind this involve complex inflammation. This may cause genetic changes in lung cells, making cancer more likely.

In short, scarring and inflammation are key in lung cancer’s development. These elements make tumor growth easier. They also change how cells act, leading to more cancer progression.
Role of Airway Inflammation in Carcinogenesis
Airway inflammation is key in lung cancer development. It causes a setting that helps tumors grow by changing the local immune response. This leads to cells transforming into cancer.
Research shows a strong link between long-term inflammation and cancer. About 20% of cancer deaths globally are due to chronic inflammation, with lung cancer being a major one. Smoking makes it worse, releasing thousands of harmful chemicals. These substances, like PAHs and nitrosamines, directly harm lung cells and increase cancer risk.
People with chronic lung diseases like COPD are more likely to get lung cancer. Their risk can be up to six times higher. Inflamed lungs don’t regulate cell growth well, which can lead to cancer. This shows how dangerous airway inflammation can be in causing cancer.
Cytokines and Their Impact on Inflammation
Cytokines are key players in the immune system, helping fight lung cancer inflammation. They are important for both starting the immune response and aiding tumor environments. By studying these cytokines, we get clearer insights into cancer progression.
Types of Cytokines Involved
There are many cytokines involved in lung cancer and inflammation. The main ones are:
- Interleukin-6 (IL-6): It helps tumors grow and survive.
- Tumor Necrosis Factor-alpha (TNF-alpha): It causes widespread inflammation and helps cancer cells live longer.
- CCL-2: This chemokine brings more immune cells to the tumor, creating an environment that helps the cancer.
Effects on Tumor Microenvironment
The way these cytokines work can make the tumor environment better for lung cancer. They help cancer cells interact with nearby cells, which can make the tumor grow and spread. This leads to several issues:
- It makes it harder for usual treatments to work because of more inflammation.
- It increases the chance of genetic mutations that can lead to cancer.
- It creates a supportive space for the tumor to grow by bringing in helpful immune cells.
This shows why it’s essential to find treatments that can change cytokine levels. Such treatments could make a big difference for lung cancer patients.

| Cytokine | Function | Impact on Lung Cancer |
|---|---|---|
| IL-6 | Promotes inflammation and survival of tumor cells | Linked to poor prognosis and tumor growth |
| TNF-alpha | Facilitates systemic inflammation | Supports cancer cell survival and proliferation |
| CCL-2 | Recruits immune cells to the tumor site | Contributes to an inflammatory microenvironment that favors tumor development |
Identifying Risk Factors for Lung Cancer
Lung cancer is a major health issue in the United States. It is caused by several risk factors. Smoking is the top cause, linked to about 72% of cases in Canada. People around smoke have a higher chance of getting this disease. Knowing these risks helps people take steps to prevent it.
Things in the environment can also cause lung cancer. Radon gas is the main reason non-smokers get lung cancer. It’s also the second biggest cause for smokers. Being around asbestos makes it worse, especially for those who smoke. Plus, air pollution is a big problem, tightly connected to lung cancer.
Having a medical history with certain diseases increases lung cancer risk. Diseases like COPD or pulmonary fibrosis make people more prone to it. The numbers show a clear link between these conditions and lung cancer risk:
| Condition | Relative Risk (RR) |
|---|---|
| COPD | 2.22 |
| Chronic Bronchitis | 1.52 |
| Emphysema | 2.04 |
| Overall (COPD, Chronic Bronchitis, Emphysema) | 1.80 |
| Pneumonia | 1.43 |
| Tuberculosis | 1.76 |
Being around dangerous toxins like arsenic in water raises risks for smokers. Having HIV/AIDS or lupus also makes lung cancer more likely because of weaker immune systems. People at risk should get regular check-ups to stay safe.
The Immune Response and Lung Injury
The immune system is key in defending the body against diseases, including cancer. When lung injury lasts for a long time, the immune system’s response can go off track. This creates a setting where tumors can grow. Lung conditions like pulmonary fibrosis and COPD change how immune cells work over time. It’s very important to understand this to help people with lung damage and cancer.
The Immune System’s Role in Tumor Development
Lung injuries, caused by things like pollution or work-related hazards, can trigger up to 300 different inflammatory responses. These responses are linked to interstitial lung disease. Conditions like silicosis and asbestosis cause long-term inflammation. This inflammation can lead to lung scarring, which might encourage tumor growth. These inflammation signals make immune cells act in ways that could, unfortunately, support cancer rather than fight it.
- Pro-inflammatory cytokines, such as TGF-β1 and IL-10, play a huge role during lung inflammation and tumor growth.
- Studies using animals show that certain minerals, like silica, keep the immune system active for too long. This can cause fibrosis and increase cancer risk.
- Having both pulmonary fibrosis and lung cancer increases the chances of getting cancer by 7% to 20%. This shows why it’s important to watch out for people with chronic lung diseases.
Looking into how the immune system and lung injuries interact shows that controlling inflammation might help prevent cancer. For more information, check out the European Respiratory Society’s research. They highlight the need for detailed studies on chronic lung diseases and cancer together.
Impact of Fibrosis on Lung Cancer Progression
Fibrosis changes how lung cancer grows because of its effects on lung tissues. The lungs become stiffer, making it hard for air to flow and for the lungs to get oxygen. This scarring also makes it easier for tumors to grow.
Lung cancer is more common in patients with idiopathic pulmonary fibrosis, or IPF. Studies show that up to 48% of people with IPF might get lung cancer. This is much higher than in the general population. Also, these patients live a lot shorter if they get lung cancer after IPF, only about 1.6 to 1.7 years.
Scars from fibrosis cause myofibroblasts to grow and more extracellular matrix to build up. This creates an inflammatory environment that helps lung cancer get worse. For example, higher levels of TGF-β help both fibrosis and cancer thrive.
In IPF patients, lung tumors often appear in the lower lobes and are linked to honeycomb lesions. This shows how closely fibrosis and cancer are connected. The ongoing abnormal cell behavior in these areas makes lung cancer develop. Finding treatments that target these issues is crucial for managing fibrosis-related lung cancer.
Recent Research Findings on Scarring and Cancer
New studies show a strong link between pulmonary scarring and a higher lung cancer risk. People with scarring are 50% more likely to get lung cancer, mainly in the scarred lung. It’s important to figure out how scarring and cancer are connected, as 7.5% of people in these studies had scarring.
There’s a clear relationship between scarring and higher lung cancer risk. The risk of lung cancer is 1.8 times higher next to the scar. This risk continues over time, meaning scarring affects not just immediate risk but long-term health too.
Adults between 55 to 74 with chest scar seen on x-rays are twice as likely to develop lung cancer. This highlights the critical need for more research, especially since lung cancer rates in patients with idiopathic pulmonary fibrosis (IPF) can be as high as 48% in some studies.
Efforts by Dr. Tatsuya Tsukui at the University of California, San Francisco, aim to find new treatments by focusing on the fibroblast response in scarring. These efforts could lead to better care for people with lung conditions linked to scarring. Researchers are working hard to learn more about how inflammation and fibroblast behavior could lead to new ways to fight lung cancer. For more details, visit https://careyourlungs.com/how-genetics-influence-your-risk-of-lung-cancer/.
Conclusion
It’s key to know how scarring and inflammation link to lung cancer to improve prevention and treatment. Scarring from long-term inflammation can make a space where tumors grow. This focus is vital in understanding lung cancer. Researchers are looking at healing and cancer growth to find new treatment targets. These can help fight off cancer spread, the top reason for cancer deaths.
Also, long-lasting inflammation in tumor cells drives cancer spread, especially in lung cancer. Genomic instability often starts this inflammation. Understanding these processes can lead to better diagnosis methods and treatments. Learning about fibroblast activation shows us how complex these processes are. This emphasizes the need for more research.
The battle against lung cancer gets stronger as we learn more about how wrong healing leads to cancer. Knowing more about the cellular activities and signaling involved is crucial for new treatments. For a deeper look into fibroblasts’ roles in repair and cancer, check out this study. It explores their roles in various situations.