Did you know that smoking is behind 85 out of 100 deaths from lung cancer each year? This shocking fact shows why we must find good ways to predict lung cancer risk. Lung cancer is a top killer worldwide, making the hunt for risk factors and prediction tools crucial. This piece looks into key ways to guess lung cancer risk. We talk about models for predicting, markers in the body, and new imaging ways. Better finding methods mean we can help patients sooner.
Now, machine learning is changing how we screen for and guess lung cancer risk. It lets researchers look at big data to find patterns. These patterns help spot individuals who might get lung cancer sooner. This shows how fighting lung cancer can get better with these advanced predictive tools.
Key Takeaways
- Smoking causes 85% of lung cancer deaths every year.
- Secondhand smoke, radiation, and polluted air also play a big role.
- Having a family history of lung cancer raises your risk.
- Machine learning is key in spotting and predicting lung cancer risk.
- Finding the disease early is vital for better treatment results.
- Predictive models are important for choosing patients for studies.
Introduction to Lung Cancer Risk
Lung cancer is a top cause of cancer deaths worldwide. Knowing the risk factors helps find it early. Smoking is the main cause of lung cancer.
Non-smokers also risk lung cancer from second-hand smoke and pollution. It’s important to know these risks to prevent and screen effectively. For example, CT scans can spot lung cancer early, especially in those at high risk.
To catch lung cancer early, it’s vital to know who’s at high risk. The USPSTF advises screening for people 55 to 80 who’ve smoked a lot. In 2021, they said to start screening at age 50 and for those who’ve smoked 20 years.
Using risk models, doctors can better predict who might get lung cancer. This makes screening more accurate. Groups now push for screenings that reflect personal risk, trying to reach everyone equally.
There are hurdles to using risk-focused screening widely. But it’s key to catching lung cancer sooner. With better screening methods, we can fight lung cancer more effectively.
Understanding Lung Cancer: The Importance of Early Detection
In the United States, lung cancer is the second most common cancer. It’s also the top cause of cancer-related deaths. Early detection is key to better outcomes for patients. Techniques like low-dose computed tomography (LDCT) scans are effective for early-stage lung cancer detection. They offer a chance for timely treatment. Sadly, only 21% of lung cancers are found while still localized. This shows the need for early and proactive screening.
The American Cancer Society suggests yearly LDCT scans for those 50 to 80 years old with a heavy smoking history. They calculate this risk using pack-years. One pack a day for a year is one pack-year. This method aims at those most at risk. Early detection can greatly improve chances of survival.
- LDCT scans can save lives by spotting lung cancer early.
- Potential drawbacks include false positives and the need for additional tests.
- Individuals receive exposure to a small amount of radiation, more than a chest x-ray but less than a standard CT scan.
- Insurance often covers lung cancer screening, providing greater accessibility to this life-saving procedure.
If a scan shows abnormal results, seeing a team of experts is crucial. They ensure proper follow-up. Also, quitting smoking greatly cuts lung cancer risk and boosts health. Knowing these facts shows early detection isn’t just good; it’s critical. It opens up better treatment options and improves patient outcomes.
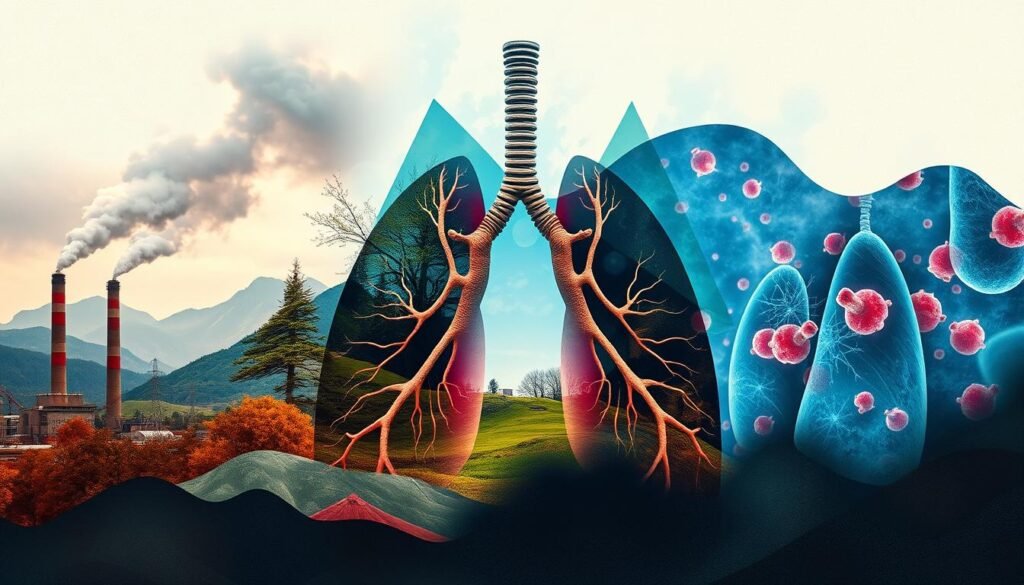
Key Risk Factors for Lung Cancer
Lung cancer is a major global health issue. It caused nearly 20% of all cancer deaths in 2018. Cigarette smoking is the leading cause of lung cancer. In some areas, it’s linked to 86% of cases. Even non-smokers can get lung cancer from second-hand smoke. This shows how smoking seriously affects lung cancer rates.
Another big factor is the environment. Things like air pollution and being around harmful substances at work raise the risk. If you’re exposed to asbestos or silica, your lung cancer risk goes up. Also, how your body reacts to these risks can depend on your genes.
Having a family history of lung cancer is a big risk too. If your family members had it, your own risk might be higher. Research has found genetic markers in some groups, like the Chinese, that make them more prone to lung cancer.
To fight lung cancer, we need good prevention methods. Stopping smoking and cutting down pollution are key steps. We also need to educate people on these risks. For more info on lung cancer risks, check out this resource.
Essential Tools and Methods for Predicting Lung Cancer Risk
Knowing how to predict lung cancer risk is key for early detection. Today, we have advanced models and machine learning to help. These tools use big datasets, helping doctors decide on patient care and treatments.
Risk Prediction Models
Risk prediction models are vital for figuring out who might get lung cancer. In the past five years, over 25 models have been made. They look at things like age, whether you smoke, and your genes. The accuracy of these models can vary a lot. Making sure they are calibrated well is important for correct risk numbers.
Machine Learning Algorithms
Machine learning is changing how we predict lung cancer risk. It can find patterns in big data sets that we might not see otherwise. For example, CanPredict uses data from 19 million adults to better identify at-risk individuals. By considering factors like smoking, weight, and health conditions, these models give detailed risk levels.
Biomarkers in Lung Cancer Prediction
Biomarkers are key in fighting lung cancer. They help find the disease or its risk. As research grows, so does our ability to customize patient care.
Checking for biomarkers means searching for DNA changes and protein levels. Lung cancer has many biomarkers, like ALK and EGFR. They help us understand each cancer better.
Advanced sequencing methods are changing the game. Dr. Heather Wakelee highlights their role in improving treatments. Certain biomarkers predict how well treatments might work.
For instance, high CEA levels usually mean a tougher fight against lung cancer. This is especially true in some stages of non-small-cell lung cancer.
- Serum biomarkers such as CEA are very accurate in diagnosing lung cancer.
- A new technique achieved a 93.3% success rate in spotting early lung cancer.
- About 20% of non-small-cell lung cancer cases show specific mutations. This affects treatment options.
Biomarkers are becoming a bigger part of lung cancer care. They help improve early detection and treatments. With ongoing research, we’re getting closer to beating lung cancer. This could reduce the number of lives it takes every year.
Advancements in Imaging Techniques
Imaging techniques have greatly improved lung cancer screening. These advancements make diagnosis more accurate. They are key in finding cancer early, which is crucial for better patient outcomes. One important breakthrough is using low-dose CT scans. Experts now see these scans as the best way for checking lung cancer.
Low-Dose Computed Tomography (CT)
Low-dose CT is a critical tool against lung cancer. It uses less radiation than regular CT scans but is still great at spotting lung issues. This means cancers are found sooner, which can save lives. The National Lung Screening Trial showed that these scans reduced lung cancer deaths by 20% in high-risk people. They compared it to those who just had regular chest X-rays.

Research shows that using low-dose CT reduces lung cancer deaths by 20-30%. This is particularly true for women. As these technologies get better, doctors get valuable information faster. This helps them care for patients better and more promptly.
The Role of Genetic Factors in Lung Cancer
Genetic factors play a big role in lung cancer, especially if it runs in the family. About 8 to 20 percent of the risk is due to genetics. Scientists have found 50 spots in our DNA that might be linked to lung cancer. But, they are still figuring out what these genes do.
It’s important to know that lung cancer isn’t just a smoker’s disease. 10 to 25 percent of people who get it never smoked. This fact shows how inherited risk can make a person more likely to get lung cancer. In South Korea, 80 percent of women with lung cancer never smoked. This fact shows we need to look more into genetic risks.
Researchers have discovered 12 new genetic variants. These are found mainly in Asian people and may increase lung cancer risk. Studies are finding specific genes that make people more prone to lung adenocarcinoma. This type of cancer is the most common, making up 85 percent of cases.
Studies of lung cancer patients show big differences in genetic markers between smokers and non-smokers. These differences show how complex genetic factors are in lung cancer. They underline the need for more personalized screening and prevention. By understanding these genetic details, we can create better treatments and preventive steps.
Environmental Exposure and its Impact on Lung Cancer Risk
Environmental factors majorly influence lung cancer development. Studies show pollution is a key factor increasing lung cancer risk. Hazardous substances like chemicals and heavy metals in the air are of concern. High pollution areas see more lung cancer cases.
Lung cancer death stats are shocking. In 2018, it caused 1,761,007 deaths globally, being the top cancer killer. The incidence and mortality rates were 22.5 and 18.6 per 100,000. Fine particulate matter (PM2.5) exposure caused about 14% of lung cancer deaths in males and 16.3% in females.
Radon exposure is also significant, with a global risk of 16.5%. In the United States, 21,100 lung cancer deaths in 1995 were radon-related. This shows how harmful this natural gas can be.
Before banning asbestos in Italy in 1992, countless workers faced exposure. About 1.1% of male lung cancer deaths were due to asbestos. This has led to serious health issues over time.
To highlight the impact of environment on lung cancer, here are some key stats:
| Environmental Factor | Contribution to Lung Cancer Mortality (%) | Specific Findings |
|---|---|---|
| PM2.5 | 14.0% (M), 16.3% (F) | Approx. 250,000 deaths globally in 2015 |
| Radon | 3.9% (M), 1.6% (F) | 21,100 deaths in the U.S. in 1995 |
| Asbestos | 1.1% (M), 0.5% (F) | Pre-1992 Italy had over 350,000 exposed workers |
It is vital to tackle these environmental risks with strong public health policies. By reducing pollution and improving air quality, we can cut lung cancer risk for the coming generations.
Utilizing Smoking History for Risk Assessment
Looking at someone’s smoking history is key in figuring out lung cancer risk. How long and how much someone has smoked matters a lot. Knowing this helps focus on how to prevent lung cancer.
This system for judging risks from smoking considers things like how old you are, when you started or stopped smoking, and how heavily you smoked. It shows that more smoking means a higher chance of dying from lung cancer. This method is simple and useful in hospitals and clinics.
A good risk assessment tool spots those at high risk better than old ways. The Pittsburgh Predictor looks at how long and heavily someone smoked and their age. Studies prove these models, which include smoking history, are better at finding who’s at risk.
| Factor | Impact on Lung Cancer Risk |
|---|---|
| Smoking Intensity | Increased risk of lung cancer correlates with the number of cigarettes smoked. |
| Quit Age | Later quit age is associated with a higher risk of lung cancer. |
| Start Age | Earlier starting age leads to a greater risk of developing lung cancer. |
| Cumulative Exposure | The longer the exposure to tobacco, the higher the mortality risk. |
By studying smoking history for risk assessment, doctors can create custom help for quitting smoking. Early and right evaluations lead to strong steps in preventing lung cancer. This means better health for people likely to get sick.
Current Lung Cancer Screening Recommendations
Lung cancer is a top reason for cancer deaths in the U.S., with more than 236,000 new cases expected by 2022’s end. Screenings are key for finding it early, which helps save lives. The U.S. Preventive Services Task Force suggests yearly screenings with low-dose CT scans. This is for people 55 to 80 who have smoked a lot, including those who smoke now or quit in the last 15 years.
Screenings are proven to lower the chance of dying from lung cancer. For example, a big study showed a 20% drop in deaths among heavy smokers who got screened with CT scans. This shows how key it is to screen people who are at high risk.
When we screen for lung cancer, we must look at the person’s age, race, and smoking history. Now, tech like artificial intelligence helps predict cancer risks better. This, along with efforts to include more people in research, aims to make screening fairer for everyone.
Not enough people are getting screened for lung cancer. To change this, we need better ways to reach out and teach people about screening. Following the latest guidelines can make a big difference in finding lung cancer early. While we’ve made progress, we need to use new prediction tools more to get everyone screened equally. Check out the U.S. Preventive Services Task Force for more info.
| Screening Method | Effectiveness | False Positive Rate | Mortality Reduction |
|---|---|---|---|
| LDCT | High | 20% (NLST), 10.4% (NELSON) | 20%-24% among high-risk individuals |
| Chest X-ray | Low | 5%-10% | No significant reduction |
| Sputum Cytology | Low | N/A | No significant reduction |
Future Research Directions in Lung Cancer Prediction
Research in lung cancer is working on better prediction models. These models aim to more accurately assess risk. They have been in development since the early 2000s, mainly in the United States.
Analysis shows that twenty-two studies have made multiple and single-use models. These studies used a variety of methods. This shows the broad approach researchers are taking.
The analytics from studies show a range in the area under the curve (AUC) from 0.57 to 0.87. This big difference means there’s room to make predictions better. The C statistic also varies, showing model performance needs more work.
Key factors in creating these models include age and how long someone has smoked. These were important in six studies. Adding family history of lung cancer in five models points to the complexity of the disease.
Even with progress, controlling bias and proving models work well is tough. These challenges highlight areas to improve in future research.
The deep learning model Sybil looks promising. It can predict lung cancer risk with one scan. In its first year, Sybil is accurate, though its success decreases over time. It also has fewer false positives than Lung-RADS. But, it needs more tests in different groups and settings.
Today’s screening mainly targets heavy smokers, but we need to include more people. The focus should also include those who have never smoked or smoke less. Working together globally can help make sure everyone has equal access to cancer prevention.
The following table summarizes key aspects of recent lung cancer predictive models:
| Model Type | Year Developed | Country of Origin | AUC Range | C Statistic Range | Validated Studies |
|---|---|---|---|---|---|
| Multiple-use Models | 2003-2016 | United States | 0.57 – 0.87 | 0.59 – 0.85 | 6 External Validations |
| Single-use Models | 2003-2016 | United States | 0.57 – 0.87 | 0.59 – 0.85 | 3 Cross-validations |
Adding advanced AI into lung cancer research offers new paths to explore. As technology gets better, focusing on new ideas, fairness, and thorough studies will guide lung cancer research into the future.
Conclusion
Lung cancer risk prediction is complex but getting better thanks to technology and studies. Doctors use risk models and biomarkers to measure the chance of getting the disease. Catching lung cancer early is vital because it can greatly increase the chances of survival.
New tools, like AI, are making lung cancer screening better. They help spot lung nodules with less radiation. These innovations also let doctors tailor check-up times for those at higher risk. A major study showed early screening reduces lung cancer deaths by 20%, highlighting early detection’s importance.
The outlook for predicting lung cancer risk is hopeful. Advances may lead to better ways of spotting and treating the disease, aiming for better patient results. Efforts are ongoing to enhance screening tools and survival rates, focusing on catching the disease early.