Did you know about 30% of mediastinal tumors are found in people aged 30 to 50? These tumors might be rare but can impact vital chest structures. This can lead to serious health problems.
Mediastinal lung cancer starts in the mediastinum. That’s the area between the lungs with many critical organs. Knowing about this cancer is important for spotting its signs. Also, it helps in understanding different tumor types and treatment options.
Early detection is key for managing this disease. It’s vital for people to know the signs. For more details, go to Mediastinal Tumors Overview.
Key Takeaways
- Mediastinal lung cancer typically occurs in adults aged 30-50.
- Most mediastinal tumors are benign, but they can still lead to serious complications.
- Early detection is crucial for better outcomes in managing mediastinal malignancies.
- Thymoma is the most common anterior mediastinal mass encountered in practice.
- Minimally invasive robotic surgery can be a treatment option for specific mediastinal tumors.
Understanding Mediastinal Lung Cancer
Mediastinal lung cancer is a major health issue. It develops in the mediastinum’s anterior, middle, and posterior parts. It comes from different tissues like lymph nodes, the thymus, and large blood vessels. This cancer’s location near vital organs makes it very serious.
Knowing about mediastinal lung cancer is key in thoracic oncology. Its symptoms can be quiet, which makes finding it early hard. Tests like CT and PET scans are critical for spotting tumors. Screening for lung cancer spread to chest lymph nodes is crucial.
Staging the lymph nodes in the mediastinum involves EBUS and Mediastinoscopy. Patients should avoid certain meds like Aspirin and Warfarin before these tests. They also need someone to help them get home safely after.
If you have lung issue signs, including those of mediastinal lung cancer, talk to a doctor. Early help can make a big difference in treatment success. Learn about the first symptoms of lung cancer
What are Mediastinal Tumors?
Mediastinal tumors are growths in the mediastinum, the area in the middle of the chest. These tumors can be either benign (not cancer) or malignant (cancer). They might start in different tissues like the thymus, lymphatic system, or soft tissues. Adults often find these tumors in the front part of the mediastinum, with lymphomas and thymomas being most common.
Thymic carcinoids make up about 2% of these tumors. Neurogenic tumors, about 25%, usually need surgery. Germ cell tumors come from cells that went wrong during gestation, in the sex organs.
Some people with mediastinal tumors may feel chest pain, cough, fever, or have trouble breathing. Yet, many don’t show symptoms and find out they have a tumor through chest imaging, like CT scans. In adults, over half of the tumors in the front part of the mediastinum don’t cause symptoms.
People often get diagnosed with these tumors between 30 and 50 years old. Adults are more likely to have malignant tumors, while kids often have benign ones. Treatments vary, with options including surgery, chemotherapy, and radiation. Because of the tumor’s complexity, specialized care from cancer centers is crucial.
Types of Mediastinal Tumors
Mediastinal tumors fall into three main areas: anterior, middle, and posterior mediastinum. Each area has certain types of tumors and masses. Knowing these helps figure out the right treatment.
Anterior Mediastinal Masses
Thymomas are the main type of anterior mediastinal tumors. These arise from the thymus gland. Mostly, thymomas are found in adults and can be either benign or harmful. If it’s thymic carcinoma, it’s more dangerous and spreads fast.
Other important tumors in this area include:
- Lymphomas, starting in the lymphatic system
- Germ cell tumors, usually in the reproductive organs
About 59% of tumors in the front mediastinum are malignant. For people with myasthenia gravis, 10-30% have thymomas. It’s key to know about these tumors for proper treatment.
Middle Mediastinal Masses
Middle mediastinal masses include different types, like bronchogenic cysts. These are mostly harmless growths from birth. Lymphadenopathy here means big lymph nodes, a sign of health problems. You might also find:
- Pericardial cysts, fluid sacs around the heart
- Tracheal or esophageal tumors, which can be benign or malignant
Recognizing these leads to the right treatment plans. Treatments and outcomes can vary greatly.
Posterior Mediastinal Masses
Posterior mediastinal masses mainly include neurogenic tumors. These tumors come from nerve tissue and are usually not harmful. Also, you might find swollen lymph nodes here. Other things could include:
- Extramedullary hematopoiesis, where bone marrow grows outside its usual place
Identifying these masses correctly is crucial. If ignored, they can seriously affect nearby structures.
| Type of Tumor | Common Characteristics | Occurrence |
|---|---|---|
| Thymoma | Slow-growing, may be linked to myasthenia gravis | Most common anterior mediastinal mass |
| Thymic Carcinoma | Fast spreading, very aggressive | Rare but has big effects |
| Bronchogenic Cyst | Harmless birth growth | Sometimes seen in the middle mediastinum |
| Neurogenic Tumors | Usually harmless, from nerve tissue | Often in the posterior mediastinum |
| Lymphadenopathy | Big lymph nodes mean health issues | Seen in every mediastinal area |
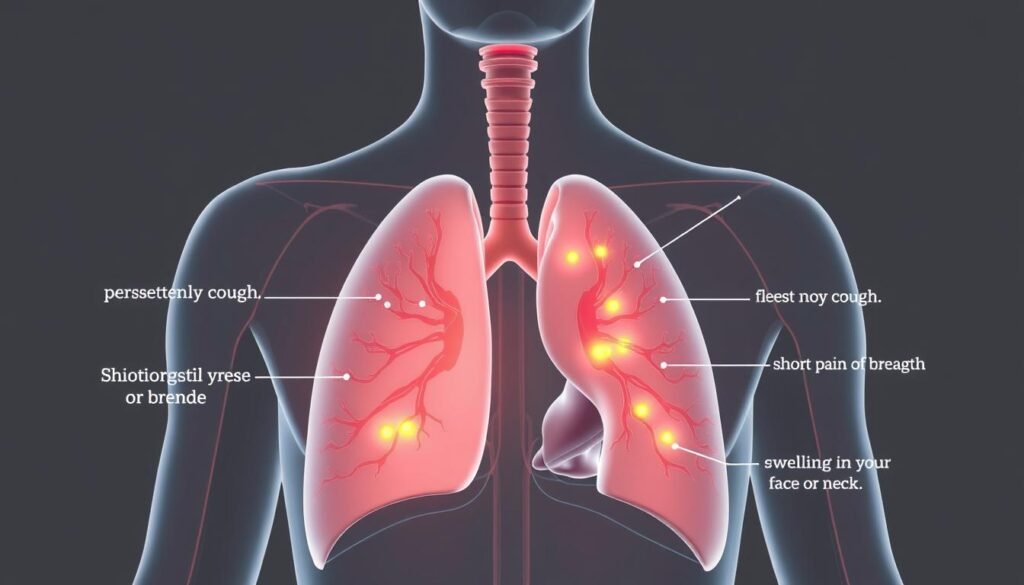
Signs and Symptoms of Mediastinal Lung Cancer
Mediastinal lung cancer shows symptoms in different ways. It depends on the tumor’s location and type. Spotting these symptoms early can play a big part in diagnosis and how well treatment works.
Common Symptoms
The symptoms seen most often include:
- Persistent cough
- Shortness of breath
- Chest pain
- Unexplained weight loss
These symptoms usually come from the tumor pushing against important areas like the lungs or heart. Fever, chills, and a hoarse voice are also common. They may show the cancer is getting worse or causing other problems. Seeing a doctor is key if you have these symptoms.
Less Common Symptoms
Some symptoms are not as easy to recognize, including:
- Night sweats
- Coughing up blood
- Significant fatigue without an obvious reason
These rare symptoms could signal serious health issues. They remind us of the need to get medical help quickly. Always watch out for new symptoms and talk to a doctor if they come up. To learn more about mediastinal tumors, check out detailed cancer research articles.
| Symptom | Commonality |
|---|---|
| Persistent cough | Common |
| Shortness of breath | Common |
| Chest pain | Common |
| Night sweats | Less Common |
| Coughing up blood | Less Common |
| Unexplained weight loss | Common |
Causes and Risk Factors
Risk factors for mediastinal lung cancer include many important aspects. These aspects heavily influence someone’s chance of getting this disease. Knowing them helps in finding and preventing the disease early.
Age and Gender
Adults, especially those aged 30 to 50, often face mediastinal tumors. Gender differences are seen as well, with certain cancers more common in specific genders. For example, lymphomas are found in young people, ages 15 to 40. Thymomas usually occur in those 40 to 60. Age and gender play huge roles in this cancer.
Family History and Immune System Disorders
Having a family history of mediastinal lung cancer raises your risk. People with family members who had lymphomas or thymomas are more at risk. Also, immune system problems, such as autoimmune diseases or HIV, increase your chances of getting these cancers. It’s important to know these risks, especially if you have family history or immune issues.
| Risk Factor | Description |
|---|---|
| Age | Most common in adults aged 30-50, with variation among specific tumors. |
| Gender | Certain tumors such as lymphomas and thymomas show differences based on gender. |
| Family History | Individuals with family members who had lymphomas or thymomas may face heightened risk. |
| Immune Disorders | Conditions like autoimmune diseases and immunodeficiencies increase susceptibility. |
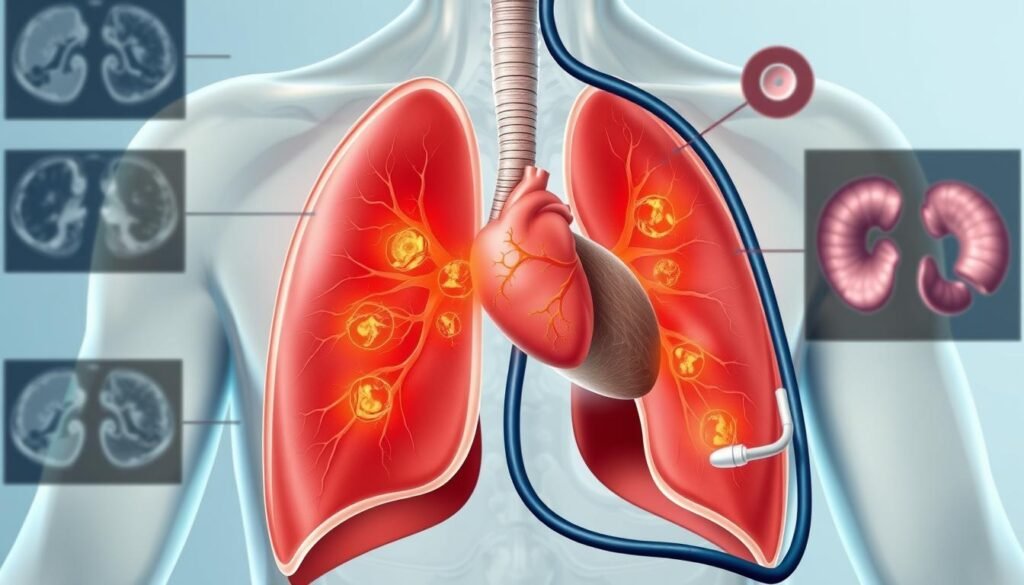
Diagnosis of Mediastinal Lung Cancer
The process starts by thoroughly checking the patient using different tests and scans. Finding mediastinal lung cancer early greatly improves treatment success. There are many ways to make sure the diagnosis is accurate.
Diagnostic Tests
Diagnostic tests are key in confirming mediastinal lung cancer. It usually begins with chest X-rays and CT scans. For closer looks, doctors use PET scans and MRIs. EBUS and EUS are especially good at finding cancer in lymph nodes, with both having an 89% success rate. Using them together even boosts this rate to 91%. Mediastinoscopy is another method, being 78% effective in identifying lymph node spread.
Importance of Early Detection
It’s very important to catch the cancer early. Early diagnosis means early treatment, which can change the disease’s path. Going for check-ups early and noticing symptoms means you’re more likely to get help sooner. Those who find out they have cancer early often have better health outcomes. This shows how vital early detection is.
Treatment Options for Mediastinal Lung Cancer
Treatment options for mediastinal lung cancer depend on the tumor and the patient’s health. Doctors often use a mix of surgery, chemotherapy, and radiation. This mix helps tackle the cancer from all sides.
Surgical Approaches
Surgery plays a key role in treating some mediastinal lung cancer cases. The aim is to remove the tumor and any nearby affected tissue. Removing all the tumor, known as R0 resection, can lead to better survival rates.
Doctors decide on surgery based on each patient’s case, especially those ready for aggressive treatments.
Radiation Therapy and Chemotherapy
Radiation therapy is a crucial part of the treatment. It uses high-energy waves to kill cancer cells. It’s used after surgery or for tumors that can’t be operated on.
Chemotherapy uses drugs to target cancer cells, taken orally or through injections. Using radiation and chemotherapy together often works better.
| Treatment Method | Purpose | Administration | Effectiveness |
|---|---|---|---|
| Mediastinal Lung Cancer Surgery | Remove tumors and excess tissue | Operative procedure | High potential for cure if R0 resection is achieved |
| Radiation Therapy | Destroy cancer cells | External radiation beams | Effective for inoperable cases or as adjunct therapy |
| Chemotherapy | Kill remaining cancer cells | Oral or intravenous | Maximizes treatment efficacy when combined with radiation |
Doctors work together closely to create a plan that best fits each patient with this disease.
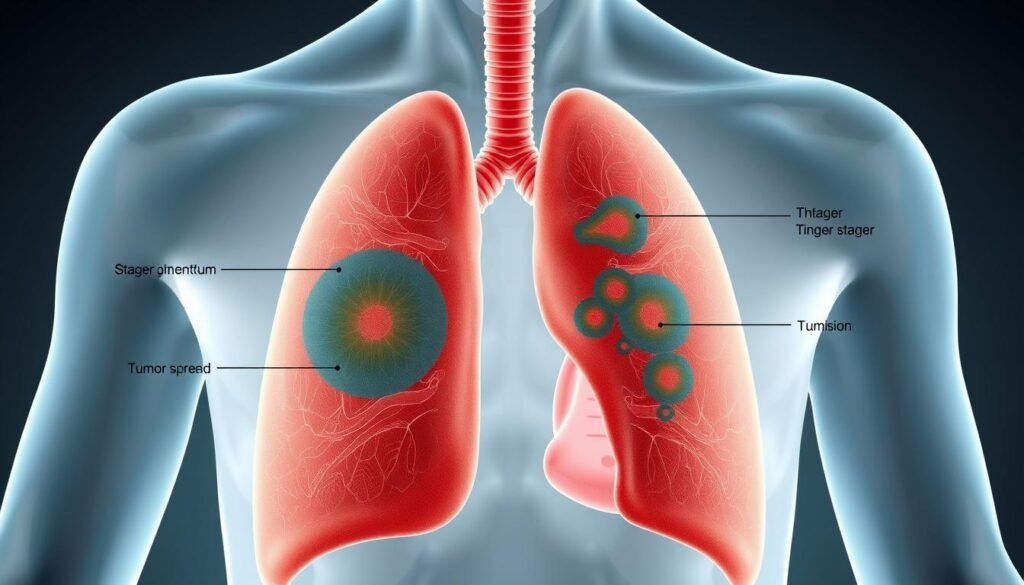
Lung Cancer Staging and Prognosis
Lung cancer staging is crucial for diagnosis and management. It shows how much the cancer has spread. This helps doctors decide on the best treatment. Staging ranges from Stage I, a localized cancer, to Stage IV, where cancer has spread widely. Knowing the stage is key for doctors and patients to choose the right treatment.
Understanding the Staging Process
The AJCC system is used for staging non-small cell lung cancer (NSCLC). It has six stages, from hidden cancer to stage IV. Each stage describes the cancer’s size and if it has reached the lymph nodes:
| Stage | Description |
|---|---|
| 0 | Localized carcinoma without spread. |
| I | No spread; further classified into I-A and I-B based on tumor size. |
| II | Involvement of nearby lymph nodes; classified into IIA and IIB. |
| III | Locally advanced cancer, likely involving mediastinal lymph nodes but no distant spread. |
| IV | Advanced cancer that has metastasized to other organs. |
Correct staging is key for picking the best treatment and predicting the patient’s outlook. Cancers found early have better survival rates. For example, localized cancers have about a 62.8 percent five-year survival. Regional cancers have around a 34.8 percent rate. However, distant cancers have a tough outlook, with an 8 percent survival rate.
Survival Rates
The outlook for lung cancer depends on the stage when found and the cancer traits. Small cell lung cancer is divided into limited and extensive stages. Limited means it’s in one lung. Extensive means it has spread. This affects survival rates. For more details, check out the American Cancer Society’s staging info.
Mediastinal Lung Cancer and Patient Support
Finding out you have mediastinal lung cancer can be really tough for both patients and their families. Having patient support is key to help during treatment and recovery. Oncology nurse navigators are there to guide patients. They help with the challenges of cancer care.
Oncology Nurse Navigators
Oncology nurse navigators are crucial for good patient care. They make sure patients get their medical appointments on time. They also provide needed information. They help by:
- Educating patients about their diagnosis and treatment options.
- Helping manage side effects and providing resources for symptom relief.
- Facilitating communication between patients and their healthcare teams.
- Offering emotional support and counseling services.
They focus on what patients need. This improves care and helps patients make choices about their health.
Supportive Care Options
Supportive care is vital for improving life quality for those with mediastinal lung cancer. It goes beyond just treatment. It includes things to help patients and their families:
- Nutritional Guidance: Tailored meal plans to support health during treatment.
- Counseling Services: Access to mental health professionals for emotional support.
- Pain Management: Ways and meds to reduce pain from cancer or treatment.
- Patient Support Groups: Meeting others with similar experiences, building community.
Using mediastinal lung cancer support resources makes the treatment journey better. It lets patients focus on healing and living well.
| Support Resource | Description | Contact Information |
|---|---|---|
| Oncology Nurse Navigator | Coordinates care and offers guidance through treatment. | Available through most treatment centers. |
| Counseling Services | Provides emotional support and counseling. | Check with local hospitals or cancer centers. |
| Nutritional Guidance | Custom meal plans to support recovery. | Offered by registered dietitians in healthcare settings. |
| Support Groups | Peer support for shared experiences in cancer treatment. | Available through cancer survivor organizations. |
Conclusion
Knowing about mediastinal lung cancer is key to raising awareness. It helps with quick diagnosis and treatment. Mediastinal staging tells doctors how to treat each patient.
Advanced imaging like PET-CT and CT scans help find cancer in lymph nodes. But, they have limits. Lymph nodes bigger than 10mm might not always show cancer accurately. So, it’s vital to use treatment insights from many experts and endoscopic exams to get a full picture of lung cancer.
Staying informed and getting regular check-ups can boost your chance of catching cancer early. The right mix of imaging, sampling, and pathology is crucial. It helps make treatment plans suited to each person’s needs and health situation.