Did you know nearly 65% of stage 1 lung cancer patients live for five years or more? This fact shows how vital it is to understand lung nodule cancer survival rates. While these statistics offer key insights, remember, outcomes can differ. Factors like cancer stage, health, and treatment play big roles.
In this article, we’ll explore lung nodule cancer survival rates in detail. We want you to know what to expect. It’s important to talk about your prognosis with medical experts. Doing so helps you understand your situation and what lies ahead. Knowing your prognosis offers hope and a way to face the future.
Key Takeaways
- Survival rates vary significantly depending on the stage of lung cancer at diagnosis.
- General estimates include 65% five-year survival for stage 1 and only 5% for stage 4 lung cancer.
- Non-small cell lung cancer (NSCLC) shows a five-year relative survival rate that differs by stage.
- Overall lung cancer survival data indicates trends based on large population studies.
- Individual prognosis can be influenced by various factors, making professional consultations essential.
- Advancements in treatment may lead to better outcomes than previously recorded statistics.
Understanding Pulmonary Nodules
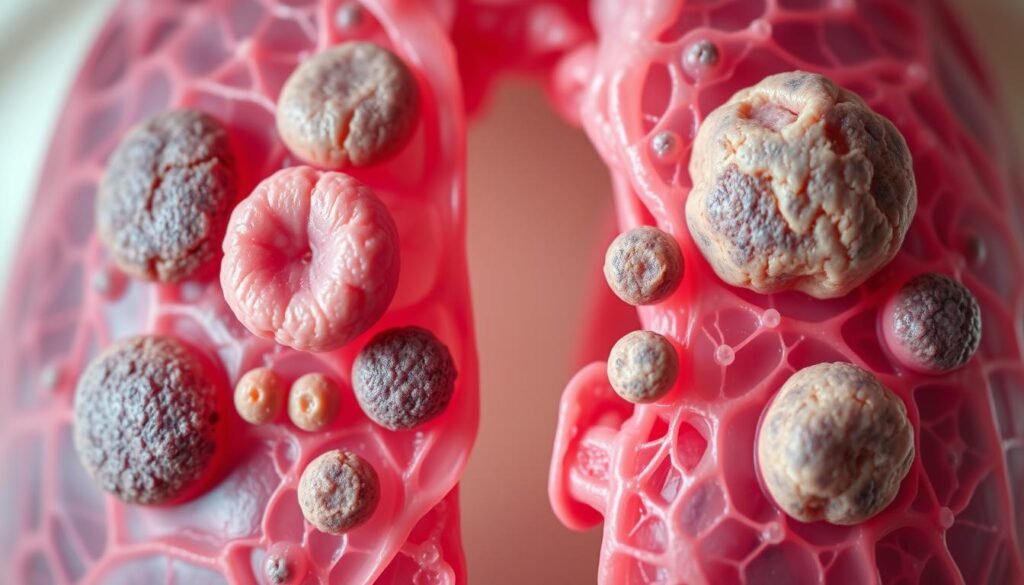
Pulmonary nodules are small, round growths in the lungs. They can be either non-cancerous or cancerous. Often, they’re found during imaging tests before any symptoms show up. It’s critical to know what they are for lung cancer detection. Thankfully, research shows that less than 5% of these nodules are cancerous. This means most are not harmful.
Many patients find out about these nodules by accident. This makes it very important to understand them clearly. Studies say only 3 to 4 out of 100 nodules are cancerous. Regular check-ups are advised to keep an eye on them. Periodic checks are recommended every 3, 6, or 12 months. This depends on the nodule’s size and features.
- Solid pulmonary nodules over 8 mm in diameter usually undergo thorough evaluation.
- Those smaller than 8 mm also require careful consideration but may have different follow-up protocols.
- Functional imaging, such as PET scans, plays a crucial role in characterizing larger solid nodules.
Clinicians look at many factors, including smoking history and age, to estimate cancer risk. Smoking is a leading cause of lung cancer in the United States. So, smokers with nodules need careful checking. Deciding on chest CT scans for monitoring relies a lot on these factors. It’s vital to keep an eye on nodules that might be cancerous.
Choosing the right way to manage nodules is also important. This might include non-surgical biopsy or surgery. Sometimes nodules are found in people without any symptoms, which is a challenge. Using guidelines to decide on management helps figure out which nodules may be cancerous. But, only about 40% of doctors follow these guidelines closely.
What Are Lung Nodules?
Lung nodules are small, abnormal areas in the lungs. They are less than three centimeters big. Often found during chest scans, like CT scans, they can appear for many reasons. For example, one in every 500 chest x-rays might show a nodule. More than 90% are found by chance during tests for other health issues.
Distinguishing between benign and cancerous nodules is crucial. Around 40% of lung nodules are cancerous. Benign ones often come from past infections, like tuberculosis. They look smooth and regular. But, cancerous nodules look rough and irregular, with color changes sometimes seen.
Knowing the difference helps doctors diagnose and treat effectively. It’s vital to watch nodules over time with more imaging tests. Cancerous nodules can grow fast, doubling in size within 25 days. People over 45 have a higher chance of getting lung nodules. This stresses the importance of careful screening.
Treating cancerous nodules may involve surgery after evaluating them closely. This might mean getting biopsies with a bronchoscope or needle. Pathologists look at these samples to check for cancer, infections, or other lung problems.
While most lung nodules are not cancerous, they could be from old infections or scars. Staying alert with regular scans and checks helps catch and treat problems early in lung care.
Lung Nodule Cancer Survival Rate
The survival rate of lung nodule cancer varies a lot. It depends on the disease stage at diagnosis and the nodule’s type. Statistics show early detection greatly affects outcomes. About 45% of patients live one year or more post-diagnosis. Only 20% live for five years or more. This shows how critical early detection and right treatment are.
General Statistics on Survival Rates
Looking at survival rates by stage gives a clearer outlook:
| Stage | Five-Year Survival Rate |
|---|---|
| Stage 1 | Approximately 65% |
| Stage 2 | About 40% |
| Stage 4 | Only 5% |
The numbers show the tough reality of lung cancer survival. Yet, those diagnosed by low-dose CT screenings have a better 20-year survival rate of 80%. Early diagnosis and regular screenings significantly enhance treatment success.
Implications of Survival Rate Estimates
Survival rates impact treatment choices and what patients can expect. Patients with nonsolid nodules have a 100% survival rate. But, those with solid nodules have a 73% survival rate. This stresses the need for careful monitoring, especially in high-risk cases.
Knowing about survival rates brings hope to diagnosed individuals. It also stresses the value of prevention, like yearly screenings. The International Early Lung Cancer Action Program’s work is promising. It has enrolled over 87,000 people, aiming to better lung cancer survival rates.
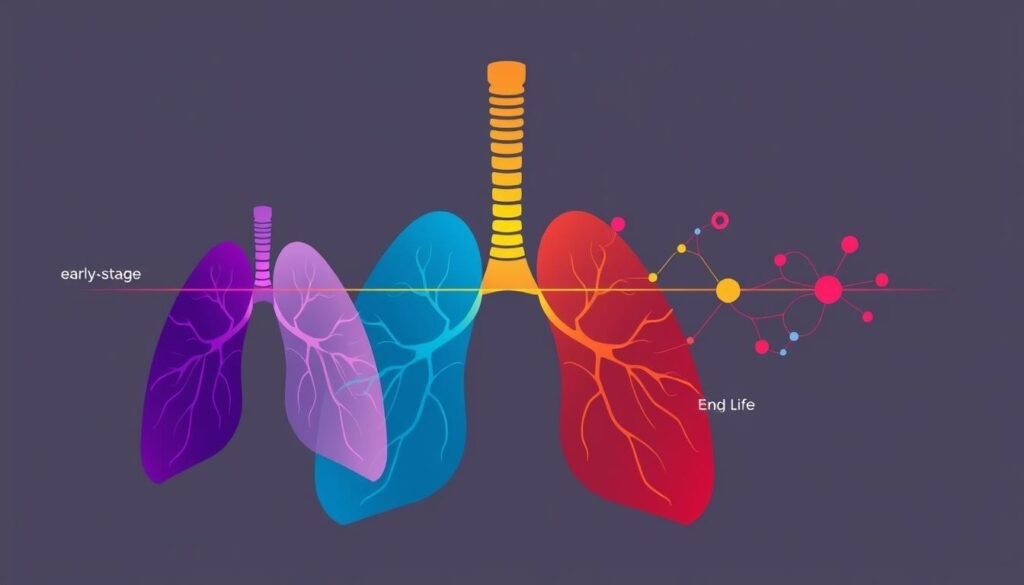
Cancer Staging and Its Impact on Survival
Cancer staging is crucial in lung cancer care. It affects survival chances and treatment choices. Staging focuses on the tumor’s size and its spread from the original spot. The TNM system of the American Joint Committee on Cancer’s 7th edition covers different lung cancers. This includes small cell carcinoma and carcinoid tumors. Knowing the stages helps predict treatment results. This is key for impacting lung cancer survival rates.
Different Cancer Stages Explained
Lung cancer stages vary from Stage 1 to Stage 4. Stage 1 means the cancer is only in the lung. By Stage 4, the cancer has spread far. Each stage affects survival rates and treatment differently.
- Stage 1: The cancer is only in the lung, with a five-year survival rate around 65%.
- Stage 2: The cancer starts to spread locally. Survival rates start to drop.
- Stage 3: Cancer has moved to nearby tissues and lymph nodes. This greatly reduces survival chances.
- Stage 4: Indicates advanced, widespread disease. Survival rates fall to about 5%.
Survival Rates by Stage
Survival rates for lung cancer depend greatly on some key factors. These include the cancer stage and tumor characteristics. Here’s a quick look at survival rates by stage:
| Stage | Five-Year Survival Rate |
|---|---|
| Stage 1 | 65% |
| Stage 2 | Approximately 50% |
| Stage 3 | Approximately 20% |
| Stage 4 | 5% |
There are more factors to consider. For instance, limited-stage small cell lung cancer usually has better results than extensive-stage cancers. Weight loss before treatment is often linked to poor outcomes. Additionally, patients with higher performance scores often do better. This shows the importance of overall health in managing cancer.
For detailed info on how updated cancer staging can change treatment options, visit this detailed analysis. Understanding these stages is vital for patients and healthcare professionals to make informed treatment choices.
Factors Affecting Lung Cancer Prognosis
It’s critical to know the lung cancer prognosis factors if you’re dealing with this disease. The success of treatment can depend on many things. These include the patient’s health, the presence of certain gene mutations, and the cancer type. That’s why it’s vital to have a treatment plan that’s tailored to you.
Being in good shape plays a big part in fighting lung cancer. Those who are healthier usually have better outcomes. Regular check-ups are key for catching issues early and improving your chances. It’s also important to watch for lung cancer symptoms to maintain quality of life.
Gene mutations also play a critical role in managing lung cancer. Research has found many markers that predict how well treatments might work. These discoveries help doctors create treatments that are just right for each patient.
| Factor | Description | Impact on Prognosis |
|---|---|---|
| Overall Health | Patients’ fitness levels and general well-being. | Better health often leads to improved treatment response. |
| Gene Mutations | Specific genetic changes associated with lung cancer. | Certain mutations can affect treatment options and outcomes. |
| Cancer Type | Differentiation between NSCLC and SCLC. | Different survival rates based on cancer type. |
| Age | Patients over 65 years experience higher risk factors. | Older age correlates with poorer outcomes. |
| Smoking Status | Current smokers versus former smokers. | Smoking cessation linked to better survival rates. |
Understanding lung cancer prognosis factors lets patients and caregivers take charge of managing the disease. Keeping an eye on these factors helps predict what might happen. It also allows doctors to provide care that fits the patient’s specific needs.
Types of Lung Cancer and Their Survival Rates
Lung cancer has different types, each with unique survival rates. It’s important for patients and their families to know these differences. There are two main types: Non-Small Cell Lung Cancer (NSCLC) and Small Cell Lung Cancer (SCLC). They have distinctive features and survival outcomes.
Non-Small Cell Lung Cancer (NSCLC)
NSCLC is the most common type, making up about 85% of cases. Its survival rates vary depending on the cancer stage at diagnosis. For early-stage NSCLC, the five-year survival rate is 65%. However, these rates decrease as cancer advances. For example, the rate drops to 37% when it reaches regional lymph nodes and to 9% for distant spread. Catching NSCLC early is crucial for a better chance of survival.
Small Cell Lung Cancer (SCLC)
SCLC is rarer and more aggressive than NSCLC. Its five-year survival rate is around 8.6%. Survival chances are higher when SCLC is found early. But, these rates fall as the cancer advances. Yet, new treatments are being developed that might improve SCLC survival statistics in the future.
The table below shows survival rates for both lung cancer types at different stages:
| Lung Cancer Type | Localized Survival Rate | Regional Survival Rate | Distant Survival Rate |
|---|---|---|---|
| NSCLC | 65% | 37% | 9% |
| SCLC | Variable (often higher than 8.6% depending on stage) | Lower than NSCLC | Around 4-8% |
Knowing the survival rates helps highlight the need for early detection and new treatments. There’s hope as therapy options evolve. For current data on lung cancer survival rates, check WebMD.
Diagnosis of Pulmonary Nodules
Doctors begin diagnosing pulmonary nodules with key imaging tests. They use x-rays and CT scans. These tests give insights into how fast the nodules grow and their qualities. This helps tell apart harmless from harmful findings. Often, doctors find nodules during routine checks or while looking for other issues.
After these imaging tests, a biopsy might be needed. It’s a way to get a clearer diagnosis. In this process, doctors take a small piece of the nodule to examine it closely. They may use needles or other tools for this, depending on where the nodule is.
Getting the diagnosis right is key. Wrong diagnoses can cause worry or delay the right treatment. So, keeping an eye on the nodules is a must. Doctors use regular scans to see any changes in the nodules. This helps them update the treatment plan if needed.
| Imaging Test | Description | Purpose |
|---|---|---|
| X-ray | A quick imaging technique using low doses of radiation | Initial identification of lung abnormalities |
| CT Scan | A detailed imaging method providing cross-sectional views of the lungs | Assessing nodule size, shape, and growth rates |
| Biopsy | A procedure to obtain tissue samples from suspicious nodules | Determining whether nodules are benign or malignant |
Doctors use a mix of imaging tests and biopsy to pinpoint pulmonary nodules. This careful approach is crucial. It helps decide the right treatment.
Treatment Options for Lung Cancer
Lung cancer treatment varies by type and stage. It often combines methods to improve outcomes. A plan might mix surgical procedures to remove tumors, especially in the early stages. For instance, surgery might cure stage 0 lung cancer, but stages I and II may need more therapy.
Surgical options are key when spotting lung nodules. The choice between minimally invasive methods like VATS or bigger surgeries depends on the tumor’s size and place. These strategies aim to get rid of cancer and might pair with other treatments later on. It’s vital for patients to talk about surgical choices with their doctors to find what’s best for them.
Surgical Procedures
When lung nodules are found, surgery is crucial in dealing with them. Depending on the nodule’s size and location, options range from minimally invasive like VATS, to major surgeries such as lobectomy or pneumonectomy. These try to remove the cancer and can be part of broader treatment plans in advanced cases. Discussing all surgical options with healthcare professionals is important to tailor the best approach.
Radiation Therapy and Chemotherapy Protocols
Radiation and chemotherapy are key in treating lung cancer. Radiation aims to shrink tumors or ease symptoms when surgery isn’t an option. Chemotherapy is vital against some lung cancers, paired with radiation. Thanks to personalized medicine, targeted therapies, and immunotherapy, there’s new hope. Learn more about detection and treatment at this resource. A team approach aims to improve patient survival and life quality.