Many are surprised to learn about the lung cancer risk in breast cancer survivors. Those who have radiotherapy are 1.59 times more likely to develop lung cancer. This fact sheds light on the serious issue of lung damage from radiation. It is vital for doctors and patients to understand how radiation hurts the lungs.
About 38 out of 1,565 patients treated for breast cancer suffered lung injury. This statistic highlights the need for careful planning of radiotherapy. It’s especially important for people with lung disease history. With millions affected by breast cancer in the U.S., it’s critical to find safer radiotherapy methods. Techniques like IMRT could help lower risk. For more details, check out the full study here.
Key Takeaways
- The incidence of lung damage from radiation therapy in breast cancer patients is significant.
- Radiation-induced lung injury can lead to severe long-term complications, affecting overall survival rates.
- Risk factors include a previous pulmonary medical history and the volume of lung exposed to radiation.
- Modern techniques like IMRT show promise in reducing radiation doses to the lungs.
- Understanding the mechanisms of lung injury is critical for improving patient care.
Understanding Radiation Therapy and Its Importance in Breast Cancer Treatment
Radiation therapy is key in battling breast cancer, especially after surgery. It aims to lower the chance of the cancer coming back. High-energy rays target cancer cells to destroy them. The use of radiation therapy is vital as it boosts the success rates of treatment.
Radiotherapy brings many benefits, improving patient outcomes. It can shrink tumors before surgery, allowing for less invasive operations. This results in fewer complications and shorter recovery times for many women. The most often used method is external radiation. Patients usually undergo this treatment over several weeks for the best outcome.
However, there are side effects to consider with radiation therapy. Patients might experience lymphedema, skin irritation, and sunburn-like effects. A long-term concern is the chance of developing secondary cancers, like lung cancer or sarcomas. Advances in technology have made treatment safer, minimizing harm to nearby organs.
Treatment methods are constantly improving, with new, shorter schedules that are just as effective. Hypofractionated schedules offer larger doses over a shorter period. They have shown to be as good as longer treatments. The medical field works tirelessly to better breast cancer treatment and minimize risks for patients.
Common Types of Radiotherapy for Breast Cancer
Breast cancer treatment uses different radiotherapy types to fight the disease. External beam radiotherapy is one common method. It uses high-energy X-rays to kill cancer cells. Patients usually have treatments Monday to Friday, for 1 to 3 weeks, based on their specific needs.
Intensity-modulated radiation therapy (IMRT) is another advanced method. It varies radiation doses to target cancer more precisely and protect healthy organs like the lungs. This shows how breast cancer treatments have improved over time.
Radiation might start 4 to 8 weeks after surgery to remove the cancer. It’s a key option after mastectomy, especially if there’s a high relapse risk or lymph nodes were affected. Doctors may use boost radiotherapy for those at higher risk to lower the chance of cancer coming back.
Learning about these methods through resources helps understand personalized treatment benefits. Techniques like accelerated partial breast irradiation (APBI) and high-dose rate (HDR) brachytherapy focus radiation on the tumor’s area. This reduces side effects and aids in a quicker recovery.
Intraoperative radiation therapy (IORT) is a quick method given right after removing the tumor. It often replaces the need for more radiation in early-stage breast cancer patients.
Radiotherapy aims to lower unintended damage and enhance the treatment’s success. It’s reassuring for patients to know that the radiation won’t make them radioactive. They can safely be around others, including pregnant women and kids.
Potential Side Effects of Breast Cancer Radiotherapy
Radiotherapy is key in breast cancer care but has side effects. Symptoms like skin irritation, redness, and tiredness may start two weeks into the treatment. These issues often worsen around two weeks after finishing treatment but they usually get better over time.
The common problems from radiotherapy include:
- Skin tenderness and soreness in the treated area might last two weeks post-therapy.
- Swelling in the breast, or lymphedema, often goes away in weeks.
- Hair loss in the underarm or treatment zone may need months to grow back.
- Joint stiffness and pain in the arm and shoulder, which usually get better after treatment.
Weakness and fatigue may impact patients, peaking during therapy. Rest, drinking water, and good nutrition can help ease these effects. Taking care of the skin properly can also reduce soreness in the affected area.
It’s vital for patients to tell their doctors about any new symptoms quickly. This helps adjust treatments and lessen discomfort. For tips on handling long-term risks, look at this guide about lung health during and after radiotherapy.
| Side Effect | Time Frame | Duration |
|---|---|---|
| Skin Irritation | 2 weeks after starting | Up to 2 weeks post-treatment |
| Breast Swelling (Lymphedema) | Post-treatment | Weeks |
| Hair Loss (Underarm) | 10 days after starting | Weeks to months |
| Fatigue | During treatment | May persist weeks |
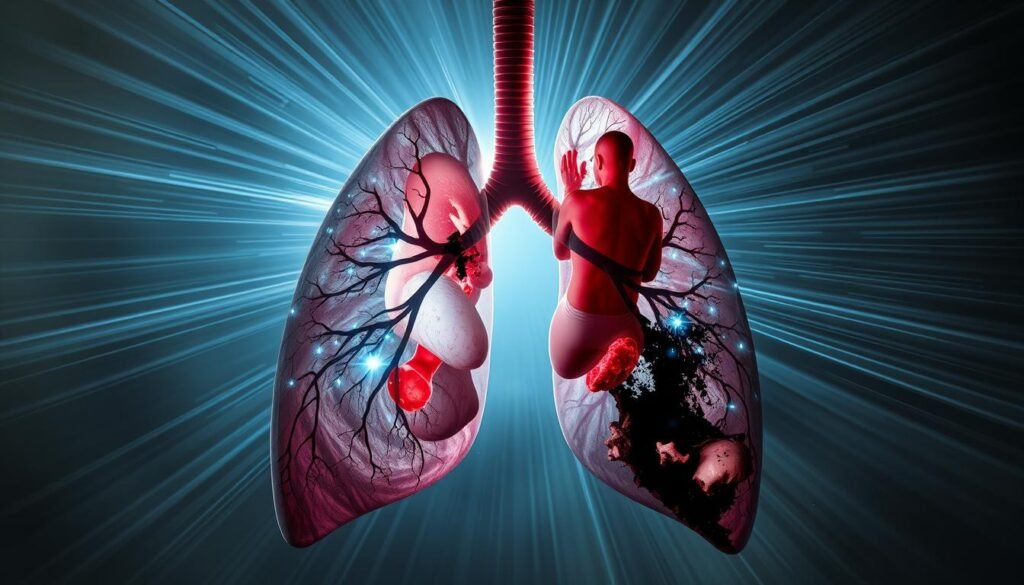
Lung Damage from Radiation Therapy for Breast Cancer
Lung damage from radiation therapy is a major concern in treating breast cancer. It’s important to look at how often lung injuries happen. Studies show a 1% to 3% injury rate in retrospective analyses. Prospective studies find it as high as 40%. This shows how complex it is to evaluate the risks of lung damage from radiotherapy.
Incidence and Prevalence of Lung Damage
About 2.4% of breast cancer patients suffer from radiation-induced lung injury (RILI). This was found in a study of 1,565 patients, where 38 faced RILI. The severity varies. For example, grade II events make up 39% of cases. Luckily, more severe grade V events haven’t been reported. This suggests severe lung injuries are rare.
Studies highlight risk factors making lung damage from radiation more likely. Patients with past lung problems are three times more at risk. Also, specific treatment details, like a dose over 15% of V30 Gy, increase the chance of getting RILI. This highlights the need for careful planning during radiation therapy.
Mechanism of Radiation-Induced Lung Injury
Radiotherapy exposes lung tissue to harmful radiation, causing cell damage and inflammation. This can lead to pneumonitis and chronic lung fibrosis. Pre-existing lung conditions can make these effects worse. Thus, knowing a patient’s medical history is crucial for safe treatment planning.
Risk Factors Associated with Lung Damage
Knowing the risks linked with lung damage in breast cancer radiotherapy is key. Different age groups, health conditions, and lifestyle choices can affect the risk of lung issues after treatment. It’s vital to understand these to create effective treatment plans.
Patient Demographics and Medical History
Age plays a big role in lung complications risk after radiotherapy. The very young and the elderly are especially at risk. A history of lung problems, like asthma, ups this risk. Smoking, directly or indirectly, also makes pulmonary issues more likely.
Radiotherapy Techniques and Dosimetric Parameters
The methods and measurement parameters in radiotherapy can predict lung damage risk. How much of the lung is exposed to radiation matters a lot. For example, higher lung exposure, as shown by V30 Gy, means greater risk. Plans tailored to each patient, considering their background and the radiotherapy technique, help lower lung damage risk.
| Risk Factor | Description | Impact |
|---|---|---|
| Age | Younger and older individuals have higher susceptibility to lung damage. | Elevated risk of long-term complications. |
| Lung History | Prior lung conditions like asthma increase risks of radiation-induced issues. | Greater chance of pulmonary problems post-treatment. |
| Smoking | Active smokers and those exposed to second-hand smoke face heightened risks. | Increased severity of potential lung damage. |
| Dosimetric Parameters | Higher doses and larger volumes of lung tissue exposed (V30 Gy). | Significantly raise the occurrence of lung injury. |
Assessing Lung Dosages in Radiotherapy Regimens
Knowing how much radiation the lungs get in breast cancer treatment is crucial. Doctors use this info to make safer treatment plans. They aim to protect the lungs, but still fight the cancer.
Mean Lung Dose (MLD) and Its Significance
MLD is key to understanding radiation therapy’s safety. It tells us the lung’s average radiation dose. This helps spot the risk of lung damage. With MLD, doctors know how to lessen the chances of pneumonitis, a lung problem after radiation.
Studies show MLD’s impact on pneumonitis rates is big. They can range from 10% to 30% with thoracic treatments. Techniques like deep inspiration breath-holding (DIBH) make MLD smaller than when patients breathe freely. So, picking the right method is important for lung safety during treatment.
Comparative Studies on Dosage Across Techniques
Different radiotherapy techniques affect lung doses differently. Techniques like VMAT and proton therapy are better for lung health. They cause fewer lung problems than older methods. A Bayesian network analysis tells us how various methods, like 3D-CRT and IMRT, have different benefits.
This research helps doctors choose the best treatment. It’s clear that checking lung doses closely is key for patient care. This way, fewer patients suffer from severe side effects.

Impact of Smoking on Lung Health During Treatment
Smoking greatly affects lung health in people getting treatment for breast cancer. The mix of smoking and radiation therapy is worrying. It raises the chance of facing more health issues. Knowing about this link helps in improving how patients recover.
The Correlation Between Smoking and Radiation Effects
Studies show smokers on radiation therapy face a higher risk of cancer coming back. The chance of recurrence is 1.56 times more with radiation alone. And, it jumps to 4.28 times with chemoradiotherapy. Plus, smokers have lower chances of staying disease-free. The risk increases to 1.88 times with radiation and 1.92 times with chemoradiotherapy. These numbers show how bad smoking is for lung health during treatment.
Also, smoking ups the chance of suffering from radiation-caused harm. There’s a 1.84 times greater risk with radiation therapy. This suggests treatments without smoking might lead to better health results. Quitting smoking can reduce the risk of these severe troubles. Since 6.8% of breast cancer patients at The University of Texas MD Anderson Cancer Center are smokers, offering them help is key.
Managing Lung Damage Post-Radiation Therapy
It’s crucial to manage lung damage after radiation to improve patient outcomes. Taking steps early on to prevent lung injury is key for cancer survivors’ quality of life. Planning treatments carefully to limit lung exposure to radiation is essential. This is because lung tissue is very sensitive. Watching for any symptoms early can lead to better handling of the condition.
Preventative Strategies for Lung Injury
To prevent lung injury, planning and patient involvement are important. Here are several strategies:
- Personalized Treatment Plans: Creating treatment plans that consider the patient’s medical history can reduce lung exposure.
- Regular Follow-ups: Healthcare providers can keep an eye on lung health and make changes as needed.
- Patient Education: Teaching patients about lung injury signs helps them seek help quickly.
These strategies are effective for managing lung damage after therapy. Acting quickly can greatly help patients recover after cancer treatments.
Warning Signs and Symptoms to Monitor
Knowing what signs to watch for is key for lung health post-radiation. Patients should look out for these:
- Persistent cough or changes in cough pattern
- Shortness of breath, especially with activity
- Unexplained chest pain or a feeling of tightness
Watching for these signs can aid in early spotting of issues like radiation pneumonitis. For more details on dealing with radiation-caused lung issues, check out the latest treatment advances here.

Treatment Options for Lung Complications Post-Radiotherapy
After radiation therapy, patients might face lung issues. But there are many treatments available. These can greatly help improve their life quality. It’s key to act early and grasp the treatment methods for RILI for effective care. The goal of treatment is to lessen symptoms, boost lung function, and consider the patient’s health history.
Therapeutic Approaches and Medical Intervention
To treat radiation pneumonitis, doctors often use:
- Corticosteroids to control inflammation and reduce symptoms.
- Cough suppressants and bronchodilators to ease respiratory distress.
- Oxygen therapy for patients experiencing severe shortness of breath.
Rehabilitation programs also play a big role. They improve lung function and overall physical health after treatment. Patients should work with a team of doctors to create a plan just for them. Keeping up with regular check-ups is crucial to adjust treatment and monitor healing.
Self-care is also important for those with lung complications. If shortness of breath occurs, take it easy and try to sleep with the upper body raised. Wearing clothes that don’t fit tightly can reduce discomfort. Knowing when to get medical help is critical for handling complications well.
For more details on lung cancer risks after radiation, visit this resource.
Conclusion
Radiation therapy in breast cancer treatment can harm the lungs. It’s vital to carefully assess and manage these risks. Around 2.4% of patients may face radiation-induced lung injury (RILI). Knowing the risk factors, like a history of lung issues, is key to avoiding these problems. Many patients might not show symptoms, making regular checks and customized treatments important.
Spotting those at greater risk, especially with past lung problems or certain chemo treatments, helps keep patients safe. High radiation doses are linked to RILI. So, planning radiation doses with care for each individual is crucial. This approach helps prevent lung problems and makes the most of radiation’s benefits.
In summary, dealing with lung risks from radiation in breast cancer care while protecting lung health is a big challenge. Better understanding and close monitoring can protect breast cancer survivors. This leads to more successful and safer treatments down the line.