Lung cancer is the top cause of cancer deaths in the US, making up almost 25% of all cancer deaths. This fact shows how crucial it is to catch lung cancer early through screening. Because of Medicare, those aged 50 to 77 can now get a low-dose CT scan, expanding access to these vital checks. This guide will talk about lung cancer screening ICD 10. It will share why preventive healthcare is so important and how Medicare can help.
With lung cancer being a major health threat, it’s important to know about screening rules. Patients and healthcare workers both need to understand who can get screened and how Medicare will cover it. By spreading the word about early screening for cancer, we hope to save more lives. We want to make sure more people get the help they need, when they need it.
Key Takeaways
- Medicare now covers LDCT lung cancer screening for patients aged 50 to 77.
- The smoking history requirement has been reduced from 30 to 20 pack-years.
- CPT® 71271 is the new billing code for LDCT lung cancer screening.
- Coinsurance and Part B deductible are waived for LDCT lung cancer screening as a preventive service.
- Understanding ICD-10 codes is essential for Medicare reimbursement.
- Screening eligibility includes a requirement for no lung cancer symptoms.
Understanding Lung Cancer and Its Impact
Lung cancer is a top cause of cancer deaths in the United States. Knowing the numbers and risk factors is key. This helps us tackle its effects.
Statistics on Lung Cancer Prevalence
About 13% of all new cancer cases each year in the U.S. are lung cancer. This equals over 200,000 people diagnosed annually. The high number of cases highlights the need for more awareness. Early screening is vital, especially for those at greater risk.
Risk Factors Associated with Lung Cancer
Smoking is the main risk factor, linked to about 85% of cases. But other risks are also important:
- Age – Older individuals are more at risk.
- Family History – A family history of lung cancer increases your risk.
- Environmental Exposures – Being around radon and asbestos can be harmful.
- Gender and Ethnicity – Some groups of people are more likely to get lung cancer.
By understanding these risk factors, we can better screen and prevent lung cancer. Helpful screening resources are available for those interested. Making everyone aware is a big step in fighting lung cancer.
Lung Cancer Screening: The Importance of Early Detection
Early detection of lung cancer can greatly improve a patient’s outcome. It not only boosts the chance of survival but also the prognosis. Lung cancer is a top cause of cancer deaths worldwide. So, effective screening is key in healthcare today.
Benefits of Early-stage Lung Cancer Detection
Using low-dose computed tomography (LDCT) for screening has been successful in finding lung cancer early. When found early, the survival rate can reach up to 55.2%. This is much higher than the 16% for late-stage diagnosis. It shows why screening is so critical for timely treatment.
- Reduced lung cancer mortality rates: Screening can lower lung cancer deaths by 20%.
- Early intervention opportunities: Finding cancer early leads to better treatment options.
- Increased awareness: Pushing for screening helps high-risk groups take charge of their health.
How Screening Can Save Lives
Regular screening greatly boosts survival rates in people at high risk. Yearly LDCT screenings have especially lowered death rates from lung cancer in women by 61%. The United States Preventative Services Task Force recommends screening for adults 55-80 years old who have a heavy smoking history.
Good communication between doctors and patients is vital. Tools for shared decision-making help patients understand the benefits and risks of screening. This way, they can make well-informed decisions about their health. By valuing early detection and screening, we can save lives and make a big impact in the battle against lung cancer.
Lung Cancer Screening ICD 10: Medicare Coverage Guide
Understanding lung cancer screening for Medicare is tricky. It needs a good grip on ICD 10 codes and coverage rules. This knowledge helps medical experts bill correctly for screenings. Thus, ensuring patients get right care and payment for lung cancer tests.
Overview of ICD 10 Codes for Lung Cancer Screening
For lung cancer screening billing, ICD 10 codes are vital. Key codes include:
- Z87.891 – History of tobacco use
- F17.21 – Nicotine dependence, current smoker
- V15.82 – History of tobacco use, applicable for coding & billing
Using these codes, doctors follow Medicare rules correctly. Without right ICD 10 codes, there’s a risk service claims might get denied. It shows the need for precise coding in lung cancer screening billing.
Medicare’s Approach to Coverage and Reimbursement
Medicare covers lung cancer screening with LDCT for those 50-77 years old. They need a history of 20 pack-years of smoking. Here’s the payment outline for these services:
| Service | Location | Reimbursement Amount |
|---|---|---|
| Counseling Visit (G0296) | Hospital Outpatient Setting | $69.65 |
| Counseling Visit (G0296) | Physician’s Office | $28.64 |
| Low-Dose CT Scan (G0297) | Hospital Outpatient Setting | $112.49 |
| Low-Dose CT Scan (G0297) | Physician’s Office | $254.93 |
Medicare bills lung cancer screening once a year. It requires 11 full months between screenings. This shows Medicare’s dedication to offering vital services. They aim to make it easy for those eligible, while dealing with lung cancer test billing challenges.
Eligibility Criteria for Lung Cancer Screening Under Medicare
Medicare has specific rules to see if someone can get lung cancer screening. These rules help make sure people who are at high risk get the right care and help.
Age and Asymptomatic Requirements
People aged 50 to 77 can get screened for lung cancer if they have no symptoms. It’s important because it targets those with a higher chance of getting lung cancer.
Tobacco Smoking History Explained
For Medicare, your smoking history matters a lot when checking if you can get screened. You need to have smoked the equivalent of 20 pack-years or more. One pack-year means smoking a pack a day for a year.
Both current smokers and those who’ve quit in the past 15 years can get a scan. Before their first scan, they need to talk about their smoking and health with a doctor. This talk helps figure out if they can get screened, gives important info, and encourages quitting smoking.
Medicare Coverage Details for Lung Cancer Screening
Medicare’s role in lung cancer screening is crucial for catching the disease early and improving outcomes. It’s essential to know how Medicare coinsurance and deductibles in healthcare work. This knowledge helps patients handle the costs of screenings better.
Understanding Coinsurance and Deductibles
Low-dose computed tomography (LDCT) is a key tool Medicare uses for lung cancer screening, making it easier for those who qualify to get screened. Luckily, this screening does not usually involve Medicare coinsurance or deductibles in healthcare. This removal of cost barriers helps at-risk patients get screened without worry about expenses.
Eligibility for this screening covers people aged 50 to 77, sometimes up to 80, depending on the guidelines. A history of heavy smoking is a major eligibility factor. This ensures high-risk individuals get the focus and care they need.
Requirements for Shared Decision-Making Visits
Before their first lung cancer screening, Medicare requires patients to have a shared decision-making in lung cancer screening visit. This visit is for confirming if someone is eligible, talking about the screening’s risks and benefits, and discussing the importance of quitting smoking for those who currently smoke or have recently quit.
This shared decision-making visit creates a space for patients to talk about their health choices. It also confirms that patients understand what the screening entails before they proceed.
By following these steps, people using Medicare for lung cancer screenings are well-informed. They can make the best choices for their health with the right support.
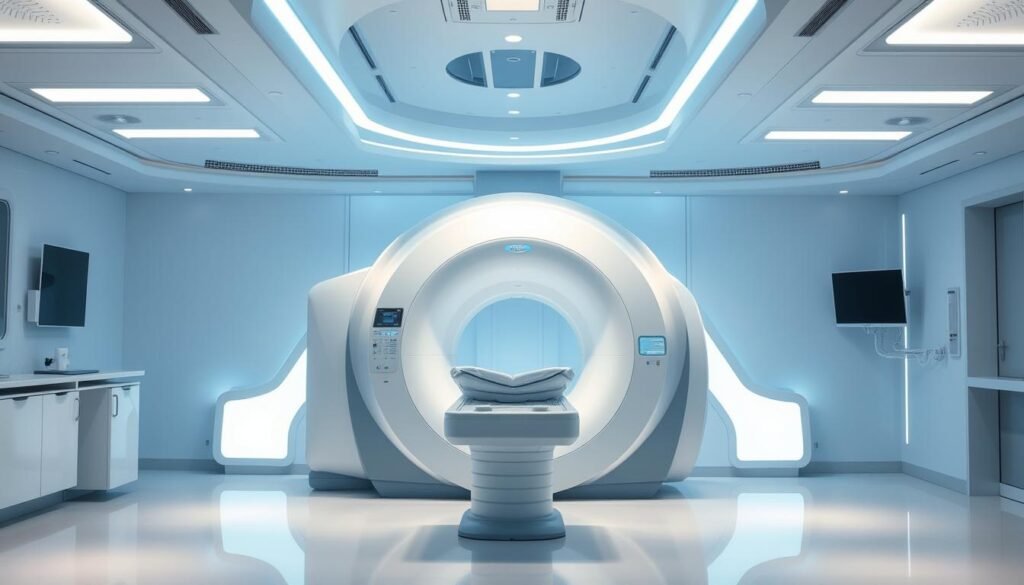
Low-Dose CT Scan and Its Role in Screening
The low-dose CT scan is key in spotting lung cancer early. It uses less radiation but still gives clear images for correct diagnosis. It’s quick, simple, and centers on patient comfort.
What to Expect During a Low-Dose CT Scan
Getting a low-dose CT scan means lying on a table that moves through a large device. It takes only minutes, but you must stay still for good images. Staff will explain each step to keep you at ease. They capture detailed lung images to spot any problems early.
How Low-Dose CT Scans Differs from Other Imaging Procedures
Low-dose CT scans stand out from other scans in key ways:
| Aspect | Low-Dose CT Scan | Traditional CT Scan |
|---|---|---|
| Radiation Exposure | Lower radiation exposure | Higher radiation exposure |
| Purpose | Primarily for lung cancer screening | General imaging for various conditions |
| Image Quality | Maintains high quality for detection | Standard quality images |
These scans are special because they lower health risks. They are especially useful for checking for lung cancer, considering things like age or smoking history. For more on who should get screened, look at lung cancer screening guidelines.
Preventive Healthcare Services and Lung Cancer Screening
Preventive healthcare services are key to staying healthy. Medicare supports these efforts by covering screenings and assessments. This includes lung cancer screenings for those at high risk. The goal is to catch health issues early, especially lung cancer.
Broader Preventive Services Covered by Medicare
Medicare offers a range of preventive care. This includes yearly check-ups, shots, and screenings for various illnesses. A major part is the lung cancer screening for high-risk people. To qualify, individuals aged 50 to 80 with a heavy smoking history must meet the criteria set by the US Preventive Services Task Force (USPSTF). Early detection through this program could lower deaths from lung cancer.
The Role of Preventive Care in Managing Health Risks
Effective preventive care is crucial for those at risk of lung cancer. It’s important to review your smoking history. Screenings are necessary for those who’ve smoked 20 pack years or more. There’s also help for those wanting to quit smoking.
By discussing the pros and cons of screening, patients can decide wisely about their care. This discussion is a key part of managing lung health well.
Staying engaged with preventive healthcare is vital. It helps in spotting issues early and can vastly improve outcomes. Those eligible should use Medicare’s preventive services to keep their health on track.
| Criteria | Details |
|---|---|
| Age Range | 50-80 years |
| Smoking History | 20 pack years minimum |
| Shared Decision-Making | Mandatory counseling session |
| Screening Frequency | Annual screening recommended |
Tobacco Exposure and Lung Cancer Risk Factors
Tobacco exposure is a major player in lung cancer. Most lung cancer cases are directly tied to smoking. It’s crucial to know how these are connected to fight against lung cancer.
Understanding the Connection Between Smoking and Lung Cancer
Smoking is the top cause of lung cancer, making up about 85% of cases. Being around tobacco smoke can greatly up your chance of getting respiratory diseases. Signs like coughing, trouble breathing, and coughing up blood could show serious issues. Catching these symptoms early may help with getting the right treatment sooner. If you’ve been around a lot of smoke or used to smoke, getting regular check-ups is key.
Tobacco Cessation Interventions for High-Risk Individuals
Stopping smoking is crucial for those at high risk of lung cancer. Programs with counseling and meds have really helped people quit. These supports make a big difference in changing smoking habits. By tackling smoking head-on, doctors can play a big part in lowering lung cancer rates in people at risk. Efforts to cut down on tobacco use include education, support groups, and nicotine replacement options.
| Intervention Type | Description | Effectiveness Rate |
|---|---|---|
| Counseling | Individual or group sessions focused on behavior change. | 20-30% |
| Pharmacotherapy | Medications that aid in nicotine withdrawal symptoms. | 25-40% |
| Combination Approaches | Utilizing both counseling and medications together. | 35-50% |

Challenges in Lung Cancer Screening Implementation
Lung cancer screening saves lives. Yet, it’s not widely used due to various challenges. Addressing these barriers is key to better access. High-risk groups face issues like poor education and few resources, leading to less screening.
Common Barriers to Screening Accessibility
Several issues make lung cancer screening hard to get. These problems are:
- Misinformation: Misunderstandings about screening’s benefits and safety are common.
- Transportation Issues: It’s hard for some, especially in rural places, to reach care centers.
- Healthcare Access: Not enough providers know how to do lung cancer screenings well.
Only 4% to 15% of those who should get screened actually do. The Lung Cancer Screening Implementation Change Package offers ways to fix this.
Solutions to Improve Screening Rates Among High-Risk Patients
Boosting screening requires several steps. They include:
- Public Education Campaigns: These efforts aim to inform people about screening and fix wrong beliefs.
- Mobile Screening Units: They help reach people in places with fewer services.
- Community Outreach: This involves talking to local groups to raise awareness and get more folks screened.
By focusing on the needs of high-risk groups and using creative ideas, we can get more people screened. For more tips on lung cancer screening, check this resource.
| Barrier | Impact on Screening | Potential Solution |
|---|---|---|
| Misinformation | Decreased awareness and belief in efficacy | Education campaigns |
| Transportation Issues | Reduced access to screening locations | Mobile units |
| Healthcare Access | Limited screening options | Increase provider training and availability |
Conclusion
Lung cancer screening is crucial for catching the disease early, which can save lives. But in 2016, only 0.44% of Medicare users aged 55 to 77 got screened with LDCT. This number is a bit higher, at 2.21%, for those diagnosed with tobacco use. These stats show the need to boost awareness and encourage more people to get screened early.
Medicare has rules for lung cancer screening, but less than 5% of those eligible got screened within two years. This shows a big gap in screening among those at risk. Knowing who is eligible, like those with a history of smoking a lot, can help. With better awareness, we hope to see lung cancer death rates drop through prevention.
It’s key for doctors to work closely with patients to make them aware of the benefits of early screening. Catching lung cancer early greatly improves chances of survival. By pushing for preventive care and making sure people know Medicare covers screening, we can fight lung cancer more effectively.