Lung cancer causes more deaths in the U.S. than any other cancer type. In 2020, about 135,720 people died from lung cancer. This fact highlights the importance of getting screened. Even though lung cancer is the second most common cancer, many don’t know the right times to get screened. This article will tell you how often you should get tested for lung cancer. We will look at what experts like the U.S. Preventive Services Task Force (USPSTF) and the American Cancer Society say. If you’re at higher risk for lung cancer, knowing these guidelines can help you make good health decisions. This can lead to catching the disease early and improving your chances of getting better.
Key Takeaways
- Lung cancer is the leading cause of cancer-related deaths in the U.S.
- The USPSTF recommends annual LDCT screening for high-risk adults aged 50 to 80.
- Screening uptake remains low, with only 14.4% of eligible individuals screened recently.
- Early detection through screening can significantly improve survival rates.
- Shared decision-making is essential in discussing screening options with healthcare providers.
Understanding Lung Cancer
Lung cancer is a major health issue that affects many people and their families. In 2020, around 228,820 new lung cancer cases were reported. This led to about 135,720 deaths in the U.S. Knowing how widespread lung cancer is and its risk factors helps us fight it better.
Prevalence and Impact of Lung Cancer
Lung cancer is the top cancer killer for both men and women. By 2024, over 116,310 men and 118,270 women might get diagnosed. Sadly, tens of thousands are expected to die from it. However, deaths from lung cancer are decreasing by 4% each year from 2017 to 2021.
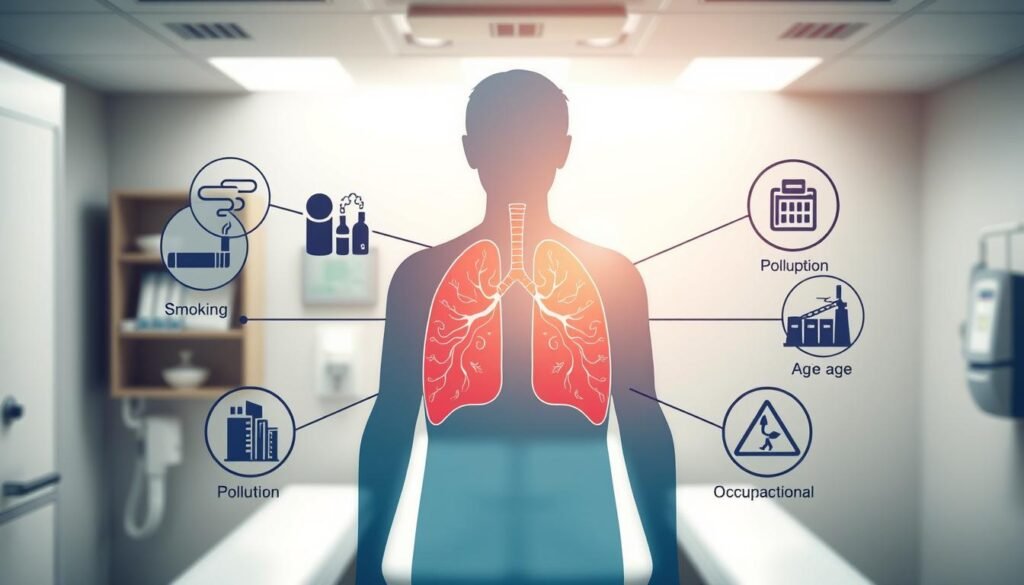
Main Risk Factors for Lung Cancer
Smoking is the main cause of lung cancer, responsible for about 90% of cases. Other risks include age, with the average diagnosis at 70 years, and environmental factors like air pollution. Radiation exposure, family history, and certain lung diseases also increase your risk.
- Age: The median age for diagnosis stands at around 70 years.
- Environmental exposures: Factors such as air pollution and occupational hazards play a role.
- Prior radiation exposure: Individuals who have undergone radiation therapy in the past may face increased risks.
- Family history: Genetics and hereditary factors contribute to lung cancer risk.
- Chronic lung diseases: Conditions such as COPD significantly elevate the risk.
To fight lung cancer, knowing these risks is important. Targeted screening is aimed at those at high risk. For detailed info on screening, click here to learn more about early detection.
The Importance of Early Detection
Finding lung cancer early can change a patient’s future. Detecting lung cancer when it first appears leads to better treatment success. Patients with early treatment enjoy healthier lives.
Survival Rates and Treatment Outcomes
About 20.5% of lung cancer patients live for five years after diagnosis. Catching it in stage I boosts survival rates to 56%. This fact shows how vital regular doctor visits and symptom checks are.
Role of Screening in Early Detection
Screening is key for finding lung cancer early. The American Cancer Society suggests yearly scans for those 50 to 80 who smoked a lot. These scans spot unusual lung spots early, helping to start treatment sooner.
With early screening, doctors can treat patients quickly. This quick action improves results. The National Lung Screening Trial found screenings reduced lung cancer deaths by 20% versus older methods. Plus, 67% of stage I lung cancers were found through screening. This shows how well screenings work.
Lung Cancer Screening Methods
Lung cancer screenings have gotten better over time. Now, low-dose computed tomography (LDCT) is the top way to find lung cancer early. This technique is very sensitive. It can spot lung cancer much earlier than older methods could. Chest X-rays and sputum cytology aren’t as effective. They haven’t helped lower the number of people dying from lung cancer. So, experts suggest not using them.
Low-Dose Computed Tomography (LDCT)
LDCT is key for spotting lung cancer early, especially in those at high risk. Studies show that LDCT screens cut down deaths from lung cancer. This is true particularly for those who’ve smoked a lot. The advantages of LDCT are that it’s quick and non-invasive. It usually takes less than a minute. People between 55 and 74, with a heavy smoking history, should get a yearly LDCT scan. This follows the National Comprehensive Cancer Network’s advice.
Comparison with Other Screening Techniques
LDCT is much better at finding lung cancer early compared to other methods. Studies using controlled groups show that chest X-rays don’t really affect lung cancer death rates. But LDCT finds over half of lung cancers early on. Without screening, about 25% of cases get identified early. Other screening methods, like sputum cytology, haven’t shown good results. However, LDCT lowers lung cancer deaths. And it does so while keeping false positives at an okay level.
Lung Cancer Screening Guidelines
Lung cancer screening is crucial in finding the disease early and preventing it. The latest guidelines show that we know more about lung cancer’s effects. By understanding these guidelines, people can see if they are eligible for screening. This helps them take steps to protect their health.
Overview of Recommendations
The U.S. Preventive Services Task Force recommends yearly lung cancer screening. This is for adults aged 50 to 80 who smoked a lot or quit in the past 15 years. The recommendations now include younger adults and those with a lighter smoking history. This change means more people can get screened. The goal is to lower the death rate from lung cancer.
Eligibility Criteria for Screening
To get screened for lung cancer, you need to meet specific criteria:
- Age: You need to be between 50 and 80 years old.
- Smoking History: You should have smoked a lot over the years or have quit in the last 15 years.
- Health Considerations: You might stop screening if you haven’t smoked in 15 years. Or, if you have health issues that affect your life span or treatment choices.
The guidelines suggest a personalized approach. They consider your health history and risk factors for lung cancer screening.
| Criteria | Description |
|---|---|
| Age | 50 to 80 years |
| Smoking History | 20 pack-years or quit within the last 15 years |
| Discontinuation | 15 years without smoking or limiting health issues |
Frequency of Lung Cancer Screening
Lung cancer screening is vital for catching the disease early, especially in high-risk groups. It’s important to know how often to get screened. Recommendations say to screen every year for those at risk, taking into account when it might be time to stop.
Annual Screening Recommendations
The USPSTF advises yearly screenings for those at high risk for lung cancer. These screenings are done with low-dose computed tomography (LDCT). People should keep getting screened until they haven’t smoked for 15 years. This approach aims to find lung cancer early, making it easier to treat.
A study showed that after three negative screenings with LDCT, the chances of getting lung cancer drop. This proves regular screenings can save lives in people who are at higher risk.
When to Stop Screening
Knowing when to stop screening for lung cancer is a delicate decision. If someone’s health worsens significantly, stopping might be the right choice. This decision should also reflect what the patient wants and their overall health condition.
Generally, if a person hasn’t smoked for 15 years, they might stop screening. This advice helps make sure treatments do more good than harm.
| Aspect | Annual Screening | Stopping Screening |
|---|---|---|
| Eligibility | High-risk individuals (ages 55-74 with 30 pack-year smoking history) | Health conditions affecting treatment options |
| Screening Method | Low-dose computed tomography (LDCT) | N/A |
| Screening Frequency | Annually | N/A |
| Criteria to Stop | N/A | 15 years smoke-free or major health issues |
Assessing Personal Risk Factors
Understanding your risk factors is key when looking into lung cancer screening. The main thing to look at is your pack-year history. This measures your smoking exposure and how likely you are to get lung cancer. It’s found by multiplying the daily packs smoked by years spent smoking. This number helps figure out your smoking history and lung cancer risk.
Understanding Pack-Year History
Pack-year history helps identify who might be at high risk and should get screened. The USPSTF once said people 55 to 80 with 30 pack-years of smoking should be screened. Now, they suggest starting at 20 pack-years and age 50. Updates like these show how risk factors guide screening plans.
Age and Smoking History Considerations
Age really impacts lung cancer risk. Nearly half of all lung cancer cases are in people over 75. So, age and smoking need to be looked at together to decide on screening. Since smoking is behind 75%-90% of lung cancers worldwide, checking both factors helps pinpoint who needs early screening. Modern risk-prediction models are getting better at finding those at high risk. You can learn more from recent research.
Benefits of Regular Screening
Screening regularly for lung cancer offers many advantages, especially when it comes to catching it early. Finding lung cancer in its early stages can drastically improve both the treatment options available and the likely outcomes. This highlights the benefits of lung cancer screening. A lot of studies back up the importance of regular screening in saving lives.
Detecting Lung Cancer Early
Early detection has benefits that go beyond health alone. For example, the National Lung Screening Trial showed a significant drop in death rates from lung cancer among those who went through screening with low-dose computed tomography (LDCT). In the LDCT group, 356 people died from lung cancer, compared to 443 in the control group. This shows a 20% drop in death rates from lung cancer, pointing out how important it is to find the disease early.
Reducing Lung Cancer Mortality Rates
The data shows that LDCT screening helped lower the death rate from lung cancer to 247 per 100,000 person-years. This is compared to 309 for those who weren’t screened. So, studies highlight how screening helps in lowering death rates. With LDCT screening, the risk of dying from lung cancer drops by 20%. This makes it clear that early screening is vital for those at high risk.
| Study | Reduction in Mortality | Lung Cancer Deaths | Lung Cancer-specific Mortality Rate |
|---|---|---|---|
| National Lung Screening Trial | 20% | 356 (LDCT) vs 443 (Control) | 247 (LDCT) vs 309 (Control) per 100,000 person-years |
| Overall Risk Reduction | Relative Risk 0.80 | – | – |
| Absolute Risk Reduction | 0.33% | – | – |
Potential Risks and Limitations of Screening
Lung cancer screening is important for early detection. It has risks and limitations, though. Knowing about these is crucial for those thinking about their screening options.
False Positives and Underlying Conditions
One big issue is false positives during screenings. About a quarter of people in a big study got false positive results from low-dose CT scans. This can cause stress, extra tests, and sometimes risky procedures.
Less than 5% might need follow-up procedures after a screening. For these folks, complications can happen 9.8% to 23.8% of the time, based on their age.
Radiation Exposure Concerns
Radiation from screening is a concern, too. Low-dose CT scans use less radiation than regular scans but still have risks. The long-term effects of this radiation need thinking about. This is especially true for those who get screened often. Weighing these risks against the benefits is key. It helps patients make informed health choices.

Shared Decision-Making in Screening
Shared decision-making is key in talks about lung cancer screening. It involves patients more closely, helping them understand what screening involves. This team effort helps people make informed choices about their health. Through this, patients learn the impact of screening and consider its risks.
Discussing Risks and Benefits with a Doctor
Talking about lung cancer screening’s pros and cons with a doctor is vital. The Centers for Medicare and Medicaid Services stress this through a required shared decision-making visit. This step is seen as crucial not only for payment reasons but also for the well-being of patients.
Studies have shown that using low-dose CT scans can cut lung cancer deaths by 20%. But it’s also important for patients to know about the possible downfalls. These include issues like finding cancer that might not cause problems (overdiagnosis) and the risks from exposure to radiation. These discussions can ease worries and help set health goals.
Importance of Patient Education
Educating patients is a big part of shared decision-making. It helps patients weigh the pros and cons of lung cancer screening. Although many patients lack knowledge about this, education can greatly improve their understanding.
Using visual aids and brochures can make complex information easier to grasp. Dialogue that invites questions and clarifies doubts is also crucial. This supportive approach leads to better decisions and health outcomes.
Implementing Lung Cancer Screening Programs
Lung cancer screening programs are vital for early detection and treatment. However, not enough people take part in these programs. There are many reasons why, and we need specific plans to make things better.
Barriers to Screening Uptake
There are several reasons why people might not get screened for lung cancer. These include:
- Lack of Awareness: A lot of people don’t know about lung cancer screening or how to get a low-dose CT scan.
- Access to Healthcare Services: It’s hard for some folks to get to the healthcare they need because of where they live or how much money they have.
- Misconceptions about Screening: Some people wrongly believe that screening is more harmful than helpful, which stops them from getting checked.
We must tackle these obstacles to get more people to participate in lung cancer screening programs. This will help us find cancer early when it’s easier to treat.
Promoting Awareness and Access to Screening
Getting the word out about lung cancer screening can really help increase participation. Some good ways to do this include:
- Community Outreach: Talking to people in their own neighborhoods can spread the word about how important screening is.
- Partnerships with Healthcare Providers: Working together with doctors and hospitals can make it easier for people to get screened by improving how we refer them.
- Incorporating Screening into Routine Care: Making sure doctors talk about screening during regular check-ups can make it a normal part of healthcare.
Overcoming the challenges in setting up these programs requires effort from both doctors and patients. By making more people aware of lung cancer screening and making it easier to access, we can make these programs work better for everyone.
Conclusion
Lung cancer screening is super important. It helps find the disease early, which can save lives. Since lung cancer is a leading cause of death, we need to screen often, especially those at high risk.
Screening every year can lower the chance of dying from lung cancer. Studies show it could cut deaths by 11% to 21%. Catching the disease early means treatment can start sooner, which makes a big difference.
We also need to make everyone aware and get rid of obstacles to screening. If more high-risk folks get screened, we could see fewer people die from lung cancer. Teaching people about how often to get screened can save lives and lead to better health for everyone.