About 10% to 20% of lung cancers are in people who’ve never smoked or who’ve had less than 100 cigarettes in their life. This means 20,000 to 40,000 lung cancer cases every year in the U.S. alone. It’s important to know that lung cancer can also affect non-smokers. This highlights the need to be aware of the signs and risk factors not linked to tobacco use.
Many things can lead to lung cancer in non-smokers. These include being around secondhand smoke, radon, and other harmful pollutants. Since adenocarcinomas are 50% to 60% of lung cancers in non-smokers, catching these signs early is crucial. Knowing about these risks and the symptoms can help at-risk individuals.
Key Takeaways
- Approximately 20,000 to 40,000 non-smokers are diagnosed with lung cancer each year in the U.S.
- Secondhand smoke and radon exposure are significant risk factors for non-smoking lung cancer.
- Adenocarcinomas make up the majority of lung cancer cases in non-smokers.
- Common symptoms often mimic other illnesses, potentially delaying diagnosis.
- Family history and genetic mutations increase risk for non-smokers.
- Awareness of environmental factors can help in prevention efforts.
Understanding Lung Cancer
Lung cancer starts in the lungs’ cells, mostly in smokers. Yet, it also strikes many non-smokers. The lung cancer definition covers various aspects and shows how complex this disease is. There are two main kinds of lung cancer: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).
Most non-smokers get non-small cell lung cancer, especially adenocarcinoma. This type makes up about 93% of cases in non-smokers. It’s found in smokers and those who’ve never smoked. Meanwhile, heavy smokers are more likely to get small cell lung cancer.
Knowing the types of lung cancer is crucial for the right diagnosis and treatment. Non-smokers with lung cancer are usually older, about 67, compared to smokers, who are around 66. Sadly, more non-smokers are diagnosed late, with 62% found at Stage IV versus 49% of smokers.
Genes play a big part in lung cancer in non-smokers. For example, non-smokers have more EGFR mutations (36%) and ALK mutations (26%). These gene changes might lead to lung cancer. Also, secondhand smoke and radon add to the risk for non-smokers.
| Attribute | Smokers | Non-Smokers |
|---|---|---|
| Common Type | Squamous Cell Carcinoma / Small Cell Lung Cancer | Adenocarcinoma |
| Average Diagnosis Age | 66 | 67 |
| Stage IV Diagnosis Rate | 49% | 62% |
| EGFR Mutations | 8% | 36% |
| ALK Mutations | 4% | 26% |
Who is Affected by Lung Cancer?
Lung cancer affects more than just smokers. In 2023, it’s estimated that over 20,000 non-smokers in the USA will die from lung cancer. This makes lung cancer one of the top reasons for cancer deaths, even among those who never smoked.
Studies show that lung cancer in non-smokers often has unique genetic markers. These differ from those found in smokers. Lung cancer rates are climbing among women, with two-thirds of non-smoker cases occurring in females. Additionally, the link between smoking and lung cancer varies across countries, pointing out global risk differences.
More non-smokers are getting lung cancer now than before. From the early 1990s to the early 2010s, the rate grew from 8.0% to 14.9%. By 2045, more women might get lung cancer than men, depending on smoking trends.

It’s crucial to spread knowledge about lung cancer risks beyond smoking. Everyone needs to know that non-smokers can also face significant risks. We must keep researching and taking steps to protect those who have never smoked.
Lung Cancer Non Smoker: Prevalence and Statistics
Lung cancer statistics show a high number of cases in people who’ve never smoked. About 10% to 20% of lung cancer cases in the U.S. involve non-smokers. The rising prevalence highlights the need for increased awareness.
Secondhand smoke is a significant risk, causing about 7,300 deaths yearly. Radon exposure also leads to around 2,900 cases annually. These facts are vital for understanding lung cancer in non-smokers.
Statistics reveal that more women, compared to men, get lung cancer without ever smoking. Rates for women aged 40-79 range from 14.4 to 20.8 per 100,000 person-years. Men’s rates are lower, from 4.8 to 13.7 per 100,000 person-years. Women especially face high rates of adenocarcinoma, more so than current or former smokers.
About 12% of U.S. lung cancer patients never smoked. This number has increased from 8% in the early 1990s to nearly 15% recently. The UK also reports rising rates among never-smokers, showing a significant demographic shift.
Lung cancer statistics for non-smokers highlight a critical health issue. Education and awareness are key in tackling this problem. Understanding the risks and symptoms is crucial for better outcomes through early detection and prevention.
Common Signs of Lung Cancer in Non-Smokers
Lung cancer isn’t just a smoker’s disease; it can happen to anyone. Spotting the signs early is key for effective treatment. Knowing symptoms that non-smokers face helps catch the disease sooner, improving chances of successful treatment.
Initial Symptoms that May Go Ignored
The first signs of lung cancer can be easy to miss. People might notice:
- A persistent cough that doesn’t get better.
- Unexplained fatigue, making daily tasks hard.
- Recurrent respiratory infections, like bronchitis or pneumonia.
- Shortness of breath when doing everyday activities.
- General malaise or feeling sick without a clear reason.
It’s easy to mistake these lung cancer signs for less serious issues, which can delay getting medical help.
Advanced Symptoms Indicating Lung Cancer
As lung cancer grows, its symptoms get more severe and need quick medical care. These include:
- Chest pain that gets worse with breathing, coughing, or laughing.
- Coughing up blood or rust-colored spit, which could signal big problems.
- Severe wheezing or starting to wheeze as an adult.
- Swelling in the face or neck, which may mean blood vessels are blocked.
- Weight loss without trying or not feeling hungry.
Noticing these serious symptoms is vital. It can lead to tests like scans which may show if tumors are present.
In conclusion, it’s critical to be aware of lung cancer signs, especially in non-smokers. Early signs can be easy to ignore, while advanced signs need fast medical checkups. Being alert to these symptoms can help start treatment sooner, which might save lives.
Key Risk Factors for Non-Smokers
Understanding lung cancer’s key risk factors is vital, especially for non-smokers. Genetic factors play a big role. If lung cancer runs in your family, your risk may be higher. This is because changes in certain genes, like the EGFR gene, can make lung cells grow abnormally.
Genetic Predisposition and Family History
Having a family history of lung cancer is a significant risk factor. If your close relatives have had it, your own risk might double or even increase more. Combining genetic factors with environmental ones could make the risk higher. But leading a healthy life, getting regular check-ups, and choosing the right foods can help lower some inherited risks.
Impact of Occupational Hazards
Jobs can put people at risk for lung cancer, especially in certain fields. Being around substances like asbestos, diesel exhaust, and arsenic can raise lung cancer risk in non-smokers. Workplaces can expose people to many toxins, increasing this danger. Following safety practices at work is crucial to lower these risks and keep workers safe.
Talking about safety at work and having regular safety checks should be normal in risky industries. Being aware and taking steps to avoid exposure can really help lower lung cancer rates in workers. For more details on non-smokers and lung cancer, check out this informative study.
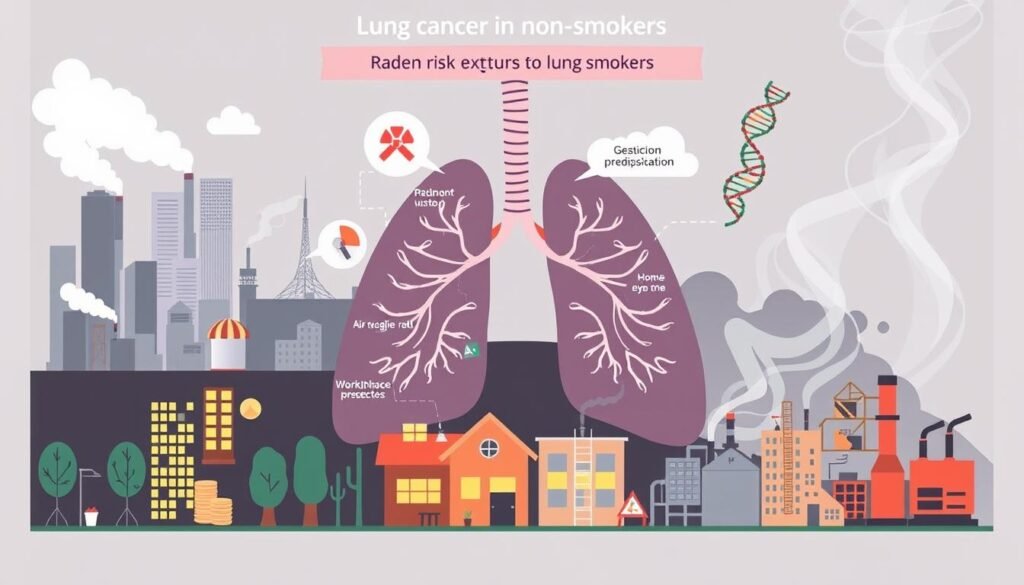
Environmental Factors Contributing to Lung Cancer
Understanding environmental factors that lead to lung cancer is key. It helps us know about risks. Some factors like secondhand smoke and radon are big concerns, especially for people who don’t smoke.
Secondhand Smoke Exposure
Being around secondhand smoke is dangerous. It can increase your chances of getting lung cancer. Even if you don’t smoke, being around others who do can harm you. In the U.S., secondhand smoke causes about 21,000 lung cancer deaths every year. It has many cancer-causing chemicals. That’s why places without smoke are important for our health.
Radon Exposure in Homes
Radon is a big problem when it comes to lung cancer. This gas comes from the ground and can build up in houses, especially if there’s not much air moving through. It’s the second main cause of lung cancer in the U.S., causing about 21,000 deaths each year. Checking your home for radon can help you stay safe. Knowing about it and taking steps can lower the dangers of this invisible gas.
The Role of Air Pollution in Lung Cancer
Air pollution is a significant environmental threat that affects lung cancer rates. It impacts both smokers and non-smokers. Now, about 25% of lung cancer cases are in people who never smoked. This fact makes it critical to understand how urban air affects lung health.
Fine particulate matter, or PM2.5, plays a big role in causing lung cancer. Just a 10 µg/m³ increase in PM2.5 can raise the lung cancer risk by 1.43 times in non-smokers. Carcinogenic air pollutants from cars and burning fossil fuels can damage lungs over time. This may lead to cancer-causing changes in the lungs.
A large study found long-term exposure to PM2.5 increases lung cancer cases. This is even in groups once considered low risk.
In 2017, PM2.5 was linked to 14.1% of lung cancer deaths worldwide. With 99% of people living in places with too much PM2.5, this issue could get worse. Stronger regulations on urban air quality can help lower lung cancer rates.
A review of 18 studies highlighted the link between particulate matter and lung cancer. In the UK, outdoor air pollution causes roughly 1 in 10 lung cancer cases. This shows the need for better air quality measures.
Nearly 6,000 never smokers in the UK die from lung cancer yearly. This shows the danger of air pollution. It also stresses the need to protect people, especially those with EGFR, from air pollution.
| Statistic | Impact |
|---|---|
| 10 µg/m³ increase in PM2.5 | 1.43 increased risk of lung cancer |
| 14.1% lung cancer deaths (2017) | Attributable to ambient PM2.5 |
| 99% population | Exceeds WHO PM2.5 limits |
| 6,000 never smokers | Die annually from lung cancer in the UK |
Importance of Early Detection Methods
Finding lung cancer early can greatly improve chances of survival and treatment. Low-dose CT scans are key in spotting the disease early. These scans have been linked to fewer deaths from lung cancer, especially for those at high risk.
In the USA, lung cancer is very common and a leading cause of death from cancer. Guidelines suggest yearly low-dose CT scans for 50 to 80-year-olds who smoked a lot. This method is only for heavy smokers because of the risks and little benefits for others.
These scans are good at finding lung cancer early which can help beat the disease. Although there is some risk from the radiation, it’s much less than regular CT scans. Studies show they can cut the chance of dying from lung cancer by up to 25% unlike chest x-rays.
It’s important to talk to a doctor before getting screened for lung cancer. These talks help understand the pros, cons, and risks of lung cancer checks. Smokers should also get help to quit smoking from these discussions.
| Screening Method | Effectiveness | Radiation Exposure |
|---|---|---|
| Low-Dose CT (LDCT) | Effective in early detection and reducing mortality | More than a standard chest x-ray, less than a standard CT scan |
| Chest X-Ray | Not recommended due to ineffective mortality reduction | Lower than LDCT |
Not many eligible people get screened for lung cancer, even with its benefits. Over 36% travel more than an hour for tests in high lung cancer areas. Screening is best for those healthy enough for treatments like surgery.
Choosing to get screened for lung cancer should involve careful talks with healthcare providers. For detailed info on lung cancer screening benefits, visit this link.
Conclusion
Raising awareness about lung cancer is more important now than ever. This is true even for people who have never smoked. Factors like radon exposure and air pollution play a big role in increasing cases. It’s vital to know the signs and risks so we can all be proactive.
If you have symptoms like a long-lasting cough or trouble breathing, it’s time to see a doctor. For extra help, websites like lung cancer prevention are great. They offer lots of information on how to lower your risk.
In the U.S., someone is diagnosed with lung cancer every two minutes. Catching it early can really improve chances of survival. Survival rates have gone up by 26% in five years, but screening is still essential.
Right now, only 16% of people who should get screened actually do. Yet, screening is proven to save lives by finding lung cancer early. We need more people to be aware and get tested to make a big difference.
We all need to work together to educate people about lung cancer. Regular doctor visits and knowing the signs can lead to earlier diagnosis and better treatment. Teaching everyone about early detection and healthy living is key to fighting lung cancer.
By taking action and spreading knowledge, we can lower the number of lung cancer cases and save lives. It’s something we can achieve as a community.