Did you know that only about 25.4 percent of lung cancer patients live beyond five years? This low number shows how serious lung cancer is. It gets more complicated with a pneumothorax, or collapsed lung. The link between lung cancer and a collapsed lung can greatly change a patient’s prognosis. We aim to shed light on lung cancer with a collapsed lung. You’ll learn about how it affects survival, signs to watch for, treatment choices, and the cancer stages.
Understanding the link between lung cancer and a collapsed lung is helpful for patients. It’s important to know how the stage of cancer, weight loss, and overall health affect living with this disease. We’ll explore these key points to help those living with lung cancer make informed choices about their care.
Key Takeaways
- The average five-year survival rate for lung cancer is approximately 25.4%.
- Stage of cancer significantly affects prognosis, with earlier stages offering better survival rates.
- The occurrence of spontaneous pneumothorax in lung cancer patients is rare.
- Factors such as general health and genetic changes can influence survival outcomes.
- Pneumothorax can complicate the prognosis for patients with lung cancer.
- Understanding symptoms and treatment options is vital for improving quality of life.
Understanding Lung Cancer
Lung cancer is the third most common cancer in the US. It falls behind breast and prostate cancer. About 235,000 new cases are found each year. Currently, roughly 611,000 people are living with lung cancer in the US. The main types are non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC makes up about 85% to 90% of all cases. Subtypes include squamous cell carcinoma, large cell carcinoma, and adenocarcinoma. SCLC, mostly seen in heavy smokers, accounts for 10% to 15% of cases.
Smoking is the leading cause of lung cancer, linked to nearly 90% of cases. What’s surprising is nearly 60% of people diagnosed have quit smoking. Secondhand smoke also causes thousands of cases each year. Moreover, most people diagnosed are older than 65.
Lung cancer cells grow fast and spread easily. This can include spreading to lymph nodes or distant organs. Knowing the stage of cancer is key because it helps predict the outcome. Sometimes, conditions like pneumothorax can point to lung cancer. This shows how tricky diagnosing and treating lung cancer can be.
Symptoms of Lung Cancer
Lung cancer symptoms can be easy to ignore at first. Many people don’t notice the early signs. A continuous cough is one of these signs. It may get worse and even bring up blood.
Chest pain often goes along with the cough. This is a clear sign that you should see a doctor right away.
Sudden weight loss without trying is another key symptom. It can happen even if you don’t change your eating or exercise. It’s a warning that shouldn’t be ignored.
Feeling very tired, not hungry, and having a different sounding voice are common too. These signs can make figuring out the problem harder.
Finding these symptoms early is super important. It can help doctors catch the cancer sooner and treat it better. If you feel anything unusual, like getting sick a lot or wheezing, get it checked out.
When lung cancer grows, symptoms can change. You might feel pain in your bones or see swelling in your lymph nodes. Knowing about these signs helps you take action early.
For more details on why it’s crucial to know these signs, check out this source.
Lung cancer can cause other problems like a collapsed lung. This shows why you must watch closely and talk to doctors quickly. If you notice any worrying signs, talking to your doctor can make a big difference in your health.
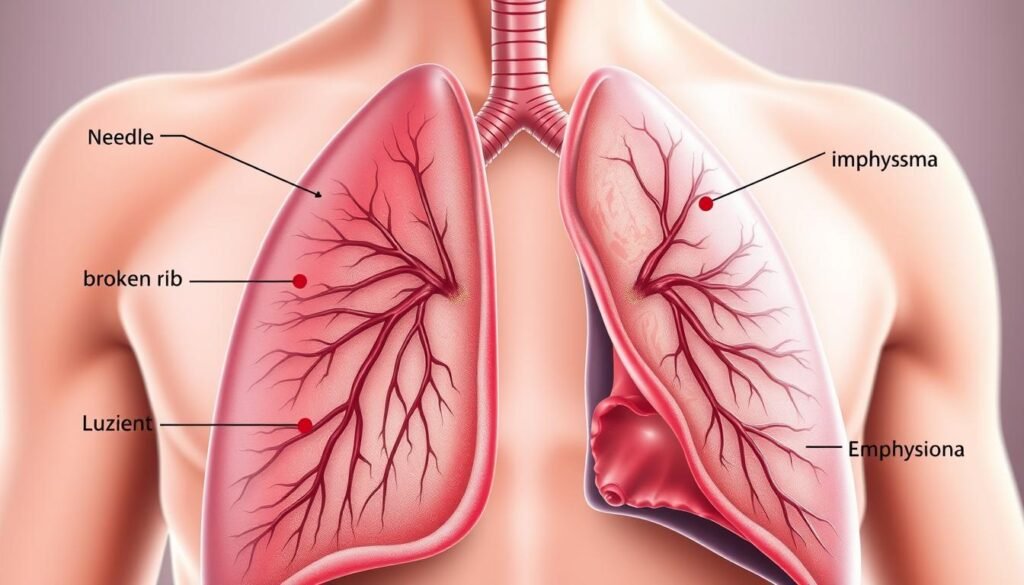
What is a Collapsed Lung?
A collapsed lung happens when air gets into the chest cavity. This can cause the lung to collapse partly or fully. If this occurs, it becomes hard for the person to breathe. They need quick help from doctors to handle this serious issue.
Many things can cause a collapsed lung. These include injuries, medical treatments, or lung diseases. Even going deep-sea diving can raise the risk. Sometimes, the body can fix a tiny lung hole by itself in about two weeks. The main aim is to get the lungs working right again.
Some people might be more likely to get a collapsed lung. This includes those who smoke, have asthma, COPD, or it’s in their family. It’s key to know how this condition impacts someone. After getting treated the first time, up to half of people might go through it again. Quick spotting of the problem with things like chest X-rays is crucial. This helps doctors step in fast.
For extra info on checking for lung issues, click here. It stresses the need to find problems early. This helps avoid major issues from a collapsed lung on your health.
Causes of a Collapsed Lung
A collapsed lung, or pneumothorax, happens for many reasons. It’s key to know the collapsed lung causes for prevention and care. Medical procedures and injuries are big factors in this condition.
Medical Procedures Leading to Pneumothorax
Some medical procedures might lead to a pneumothorax by accident. Examples include:
- Biopsies: Lung biopsies might let air into the pleural space.
- Mechanical ventilation: Ventilators can damage the lungs, leading to air leaks.
- Central line placement: Placing medication lines might puncture the lung.
Knowing these risks helps patients and doctors handle pneumothorax causes better during treatment.
Injuries Resulting in Collapsed Lung
Injuries and accidents are big collapsed lung causes. Chest injuries from trauma are common. Main reasons include:
- Blunt force trauma: This can come from falls or car accidents.
- Fractured ribs: Broken ribs can pierce the lung and let air out.
- Sports injuries: Injuries during sports can harm the lungs.
Knowing about these lung injuries helps in planning how to avoid them. This is especially true for smokers and those with lung issues. For tips on spotting lung problems early, check out early symptoms of lung cancer.
Lung Cancer Collapsed Lung Prognosis
It’s critical to understand the outlook for lung cancer patients with a collapsed lung. This will help with planning treatment and supporting the patient. A collapsed lung can change the prognosis for lung cancer, making it important to know which factors influence outcomes.
Factors Affecting Prognosis
Several factors affect the survival rates of lung cancer patients. These include:
- Overall health status of the patient
- Stage of lung cancer at diagnosis
- Any changes in weight during treatment
- Genetic factors that may impact recovery
Studies show that patients with a collapsed lung have a worse outlook. For example, those with conditions like CTD-ILD are at a much higher risk of facing severe issues with their prognosis.
Survival Rates Associated with Lung Cancer
Lung cancer survival rates depend on many factors. This includes the stage of cancer and if there’s a pneumothorax. For example, patients with a pneumothorax have a 10-year survival rate of only 29.6%. This is much lower than the 81.3% for those without it. Spotting lung cancer early by recognizing persistent symptoms is very important. It can improve survival rates. If you’re worried about lung cancer, you can learn about early warning signs. This can help you get treatment sooner.
| Condition | 10-Year Survival Rate | Mortality Rate |
|---|---|---|
| With Pneumothorax | 29.6% | 66.7% |
| Without Pneumothorax | 81.3% | 17.2% |
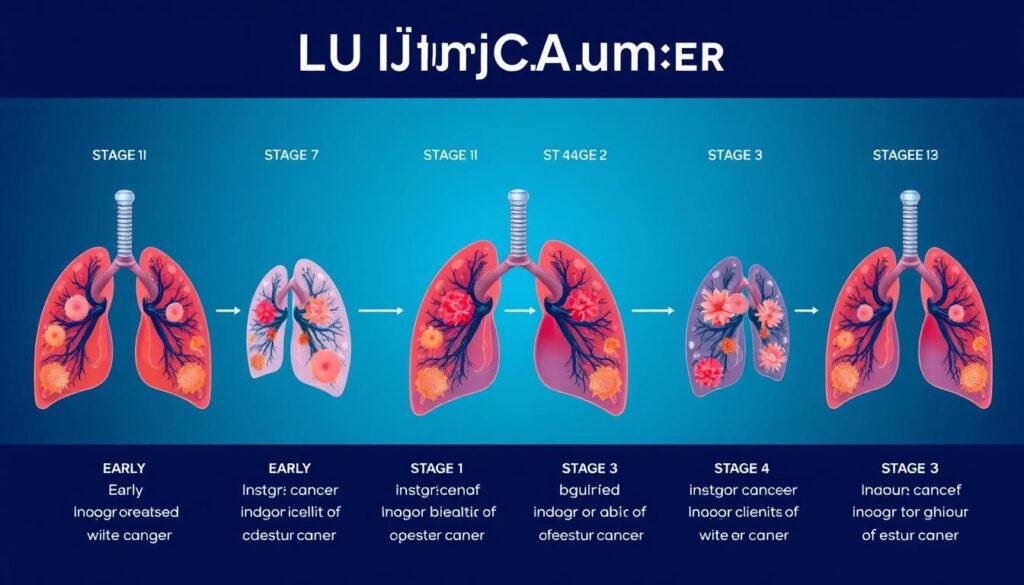
Stages of Lung Cancer
It’s key to know the different lung cancer stages. This knowledge shapes the treatment choices and hope for recovery. Cancer at stages 0 to 1 means it has not spread much. This offers a better chance for a good outcome. When the cancer reaches stages 2, 3, and 4, its impact on health gets worse, and survival rates drop.
Early Stages vs Advanced Stages
Early stage lung cancer is at stage 0 or 1, meaning it’s local. At stage 0, the cancer cells stay within the airways’ lining. Stage 1’s classification depends on the tumor’s size. Tumors up to 3 cm are stage 1A, but larger tumors at 1B could cause more serious issues, like a lung collapse.
When cancer moves to stages 2 through 4, it becomes advanced, and the outlook dims. Stage 2 cancer has bigger tumors that may reach the chest wall. Stage 3 sees the spread to lymph nodes close by. By stage 4, the cancer has spread far, reaching other organs.
Importance of Staging on Prognosis
Figuring out the cancer stage is crucial for predicting the outcome. Earlier stages mean better chances of beating the disease, thanks to limited spreading. Advanced stages, however, bring bigger hurdles, lower chances of survival, and often, tougher treatments. Knowing the exact stage helps in planning the care, influencing decisions about treatment options.
| Stage | Characteristics | Prognosis |
|---|---|---|
| 0 | Carcinoma in situ | High survival rate |
| 1A | Tumor ≤ 3 cm | Good outcomes |
| 1B | Tumor > 3 cm | Moderate outcomes |
| 2A | Tumor > 4 cm, localized | Moderate treatment options |
| 2B | Tumor > 5 cm or multiple | Lower survival rates |
| 3A | Small tumor, nearby lymph involvement | Varied prognosis |
| 3B | Larger tumor, opposite side lymph nodes | Poorer outcomes |
| 3C | Larger tumors, distant lymph nodes | Significantly affected |
| 4 | Metastatic spread | Very poor prognosis |
Lung Cancer Treatment Options
Lung cancer offers different treatment paths based on the patient’s condition and cancer stage. Treatments may include surgery, chemotherapy, or radiation therapy. Each method helps patients and families make knowledgeable choices about their care.
Surgery
Surgery is often the main treatment for early-stage non-small cell lung cancer (NSCLC). The surgery types are lobectomy, pneumonectomy, and wedge resection/segmentectomy. Each has benefits and risks like pneumonia or heavy bleeding.
Chemotherapy
Doctors may suggest chemotherapy when surgery isn’t an option or cancer has spread. It involves taking medicine in cycles, followed by rest. Chemotherapy can also boost surgery results or ease symptoms.
Radiation Therapy
Radiation therapy is key for lung cancer treatment. It works alone or with surgery and chemotherapy. Types include radical, stereotactic, and palliative radiation. Although effective, it may cause fatigue and skin issues, needing careful monitoring.
Recovery from Collapsed Lung
It’s vital to know how to recover from a collapsed lung for the best healing. The recovery journey includes healing time, follow-up care, and lifestyle changes. What you can expect depends on the cause and if you have other lung issues, like lung cancer.
Long-term Recovery Expectations
If you’re getting better from a collapsed lung, you should know about possible complications. Recovery often takes days for the lung to expand again. Some people may need more rest. It’s crucial to keep having check-ups to watch your lung function and see if it happens again.
- Shortness of breath
- Chest pain
- Anxiety and emotional stress
These symptoms are serious and mean you need to see a doctor right away. Staying in touch with medical experts is key. Talking medicine like painkillers and antibiotics helps you recover well. You should also stay away from risky activities, like flying or diving, for a while.
Rehabilitation for Lung Cancer Survivors
Rehab is important for lung health and life quality, especially after lung cancer. Joining a rehab program helps with exercises and learning, supporting your recovery. Quitting smoking is also a good idea to get better faster.
| Rehabilitation Component | Description | Benefits |
|---|---|---|
| Exercise Programs | Guided physical activities designed to strengthen respiratory muscles. | Improved lung capacity and overall physical fitness. |
| Education | Information on managing symptoms and understanding lung health. | Increased awareness and self-management of lung conditions. |
| Support Groups | Peer support for emotional and psychological well-being. | Reduced feelings of isolation and increased coping strategies. |
Being committed to recovery and talking openly with your doctors helps improve lung health after a collapse.
Pleural Effusion and Pneumothorax
Pleural effusion and pneumothorax are two conditions that affect respiratory health. It’s important to understand how they relate to each other. This knowledge is key for managing and treating these issues. This is especially true for people with lung cancer or other malignancies.
Understanding the Relationship
Pleural effusion is when fluid builds up in the pleural cavity. This can make pneumothorax, or collapsed lung, more complicated. Symptoms of pleural effusion include breathlessness, coughing, and chest pain.
About 15% of lung cancer patients have pleural effusion when diagnosed. This number goes up to 50% over time. This shows why keeping an eye on lung health is crucial. Malignant pleural effusion, linked with lung cancer, complicates diagnosis and treatment due to its similarity with pneumothorax.
Possible Treatment Options
Treatments for pleural effusion and pneumothorax often overlap. Here are some common treatments:
- Pleural Aspiration: This procedure can relieve symptoms but might not be the best for cancer-related fluid. The fluid may build up again quickly.
- Pleural Drainage: This involves putting in a catheter for ongoing fluid drainage. It’s used when lots of fluid keeps building up.
- Pleurodesis: This treatment uses materials like talcum powder to close the pleural space. It usually means staying in the hospital for a bit to drain fluid and for monitoring.
- Indwelling Pleural Catheter: For those with frequent effusions, this catheter stays in for long-term drainage.
Choosing a treatment depends on many things. These include the patient’s health, the type of cancer, and how much fluid is in the pleural cavity. Careful management is needed when both pleural effusion and pneumothorax are present. This way, patients get care that’s right for their specific needs.
| Treatment Option | Description | Hospitalization Requirement |
|---|---|---|
| Pleural Aspiration | Removal of fluid for symptom relief, not typically ideal for malignancies. | Possible overnight stay. |
| Pleural Drainage | Inserting a catheter for persistent fluid drainage. | Varies based on method; may require more than a day. |
| Pleurodesis | Sealing the pleural cavity to prevent fluid accumulation. | A few nights for monitoring and drainage. |
| Indwelling Pleural Catheter | Long-term drainage option for recurrent effusions. | Generally outpatient, but regular follow-up required. |
Thoracic Surgery for Lung Cancer
Thoracic surgery is key in lung cancer care, focusing on removing tumors. Lobectomy, wedge resection, and pneumonectomy are top methods. Which method to use depends on the tumor’s size, place, and patient health.
Video-Assisted Thoracoscopic Surgery (VATS) reflects modern, less invasive techniques. From 2002 to 2007, VATS lobectomies jumped from 10% to 29%. In Denmark, over half of lobectomies are done using VATS. In some areas, 80% of these surgeries are VATS, showing wide acceptance.

Thoracic surgery, best for many lung cancer patients, comes with risks. Problems can include infections, bleeding, and severe conditions. Rates of complications can reach 58% with traditional surgery but are lower with VATS, between 6% and 34.2%. Yet, patients might still face breathlessness and pain from nerve damage.
Recovery after lung surgery is crucial. Using surgical options wisely helps improve breathing. A good support system is essential for recovery. Talking to your doctor about any issues after surgery is critical for health and getting back to normal life.
Lifestyle Changes for Better Prognosis
Making lifestyle changes when you have lung cancer can greatly help your health and how well you do. A key step is stopping smoking. Quitting smoking improves how your lungs work. It also makes treatments work better and helps you recover faster.
Eating well is crucial too. A diet for lung cancer should include lots of fruits, veggies, grains, and lean meats. These foods give you the nutrients you need to heal. Drinking plenty of water is important too. It helps with digestion and feeling well, especially when dealing with treatment side effects.
Being active is important as well. Light exercises like walking or stretching can reduce fatigue and anxiety from treatment. Even small activities make a difference. Experts like physical therapists can help with setting up safe and good exercise plans.
Some folks might find exercising hard, especially if they’re very tired or have a weak immune system. It’s key to be careful but try to keep moving as much as you can.
In summary, to fight lung cancer, stopping smoking, eating right, and exercising are all vital. These changes are good for you while in treatment and for staying well later on. They help you get better and live a healthier life.
Psychosocial Support for Patients
Getting diagnosed with lung cancer brings lots of emotional challenges. Psychosocial support helps patients and their families handle these feelings. It makes coping with the disease’s complexities easier.
There are many types of support available, like counseling, support groups, and learning materials. These resources improve the mental health of those facing lung cancer. Lung cancer support networks create a sense of community. This helps reduce the loneliness that can come with treatment.
- Counseling: Personalized sessions help patients understand and manage their feelings and fears.
- Support Groups: Connecting with others facing similar struggles can provide comfort and shared experiences.
- Educational Resources: Access to information empowers patients and families to make informed decisions regarding treatment and care.
| Type of Support | Description | Benefits |
|---|---|---|
| Counseling | Individual sessions focusing on emotional well-being | Improved coping strategies and resilience |
| Support Groups | Gatherings for sharing experiences and advice | A sense of belonging and understanding |
| Educational Resources | Information on lung cancer treatment and care options | Increased confidence in health decisions |
Psychosocial support significantly helps those on their lung cancer journey. It tackles the emotional challenges they face. And it boosts their overall well-being. For the best care, combining medical treatments and psychosocial support is critical. It improves the life quality and mental health of lung cancer patients.
Conclusion
Lung cancer and collapsed lung prognosis are closely linked, showing how complex lung health is. It’s essential for both patients and healthcare professionals to understand the prognosis of lung cancer. Although a collapsed lung with cancer is rare (0.03% to 0.05%), it’s critical to detect and manage lung issues on time.
Patient’s outcomes may not change if a collapsed lung is treated well. This is true even when compared to those without this problem.
How lung cancer is managed can greatly impact long-term health. Survival depends a lot on the type of lung cancer and its stage when found. For patients, early action and proper care are key to live better, even with such daunting diseases.
Handling lung cancer and its challenges needs a full approach. This includes medical care, emotional support, and changes to one’s lifestyle. It’s important for patients to work closely with their doctors and get help when needed. Doing so helps achieve better health outcomes and gives more insight into their condition.