About 85% of lung cancers are known as non-small cell lung cancer (NSCLC). Large cell carcinoma, a part of NSCLC, makes up 10% of these cases. It often comes with a bad outlook and many treatment challenges. Knowing about this subtype is key. It affects how doctors diagnose and treat it, and also how well patients might do.
This guide takes a close look at the prognosis and treatment options for large cell carcinoma. It discusses symptoms, how the cancer is staged, and treatment strategies for lung cancer. It’s important to understand LCC deeply because catching it early can really help to increase survival. For more details on large cell carcinoma, click here.
Key Takeaways
- Large Cell Carcinoma constitutes around 10% of non-small cell lung cancer cases.
- Early detection significantly enhances survival rates in lung cancer patients.
- Understanding lung cancer staging is crucial for effective treatment planning.
- Biomarker testing can identify genetic drivers essential for personalized treatment.
- The five-year survival rates for LCC vary widely based on the cancer’s stage.
Understanding Large Cell Carcinoma
Large cell carcinoma is a main type of lung cancer, called non-small cell lung cancer (NSCLC). It makes up about 80% to 85% of all lung cancer cases. As one of the three main subtypes, it shows unique features that affect diagnosis and treatment.
This cancer starts from big cells and can grow anywhere in the lung. It grows fast and is likely to spread quickly. This makes treating it quite hard. Unlike adenocarcinoma, seen more in younger people and women, large cell carcinoma is found mostly in older men.
Who gets this cancer is often tied to certain risk factors, like smoking. This is different from squamous cell carcinoma, which is directly linked to smoking. Large cell carcinoma involves various factors in its development.
Treating this cancer is hard because it progresses quickly. Doctors need to use strong methods for diagnosing and treating it, based on the patient’s specific situation. Understanding this complex cancer is key to improving how patients are cared for and helping research.
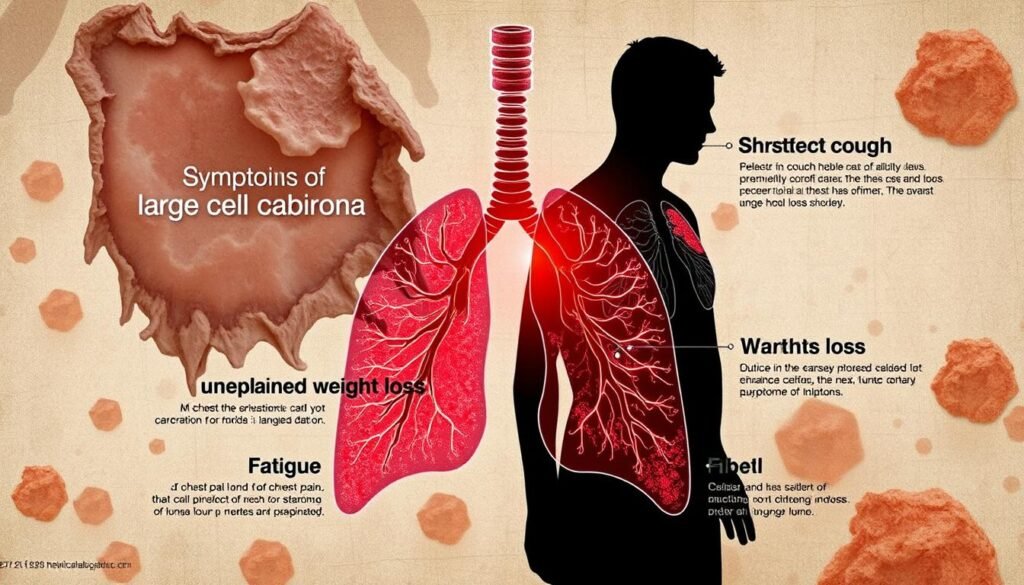
Symptoms of Large Cell Carcinoma
The symptoms of large cell carcinoma might show in many ways, based on the stage of cancer. People may feel various lung cancer symptoms such as:
- Persistent cough – This is a long-lasting cough that doesn’t go away and is a clear sign to watch for.
- Coughing up blood or rust-colored phlegm, which could mean there are complications.
- Chest pain – This is discomfort in the chest, often linked with lung problems.
- Shortness of breath, becoming more noticeable over time.
- Hoarseness, which could mean the cancer is affecting areas around it.
Other symptoms to be aware of include:
- Sudden weight loss, signaling a problem with overall health.
- Persistent fatigue, even with plenty of rest.
- Repeated infections, like bronchitis or pneumonia, can show a weakened lung system.
It’s key to know these symptoms for quick action. Spotting signs of lung cancer early, like ongoing cough and chest discomfort, is crucial. Quick diagnosis greatly helps in treating it effectively and improving results.
| Symptom | Description |
|---|---|
| Persistent Cough | A chronic cough lasting weeks or longer, often worsening over time. |
| Coughing Up Blood | Presence of blood or rust-colored phlegm, suggesting serious lung issues. |
| Chest Pain | Discomfort or tightness in the chest possibly linked to lung involvement. |
| Shortness of Breath | Difficulty breathing or breathlessness that can indicate advanced disease. |
| Hoarseness | Changes in voice quality, which may signify impacts on nearby vocal cords. |
| Weight Loss | Unintentional and significant loss of weight affecting health. |
| Fatigue | Persistent tiredness not alleviated by rest, impacting daily life. |
| Recurring Infections | Frequent respiratory infections that may point to lung function decline. |
Staging and Diagnosis
Diagnosing large cell carcinoma starts with specific imaging tests. Tests like X-rays, CT scans, and MRIs spot tumors. They show us if cancer is there and how much. Next, doctors use needle biopsy and sputum cytology. These tests confirm if it’s lung cancer.
The TNM staging system is key for large cell carcinoma. It looks at three things:
- Tumor size and extent
- Lymph node involvement
- Presence of metastasis
Each cancer stage tells doctors what treatments might work and the outlook. Stages go from 0, cancer only in the lung lining, to IV, cancer in other organs. Knowing the stage helps doctors plan the best treatment, improving chances.
Using the TNM system, doctors can make treatment plans that fit each case. This could be surgery, radiation, or chemo. After finding the cancer stage, doctors and patients discuss which treatments could help. This plan gives care that fits the cancer’s severity.
Prognosis and Treatment Options for Large Cell Carcinoma
It’s vital for patients and doctors to understand the outlook for large cell carcinoma (LCC). This helps when talking about ways to treat lung cancer. Survival rates change a lot because of several reasons like the cancer’s stage when found and the patient’s age and sex. A study of 3,197 people with LCC gives details about survival times and what affects them.
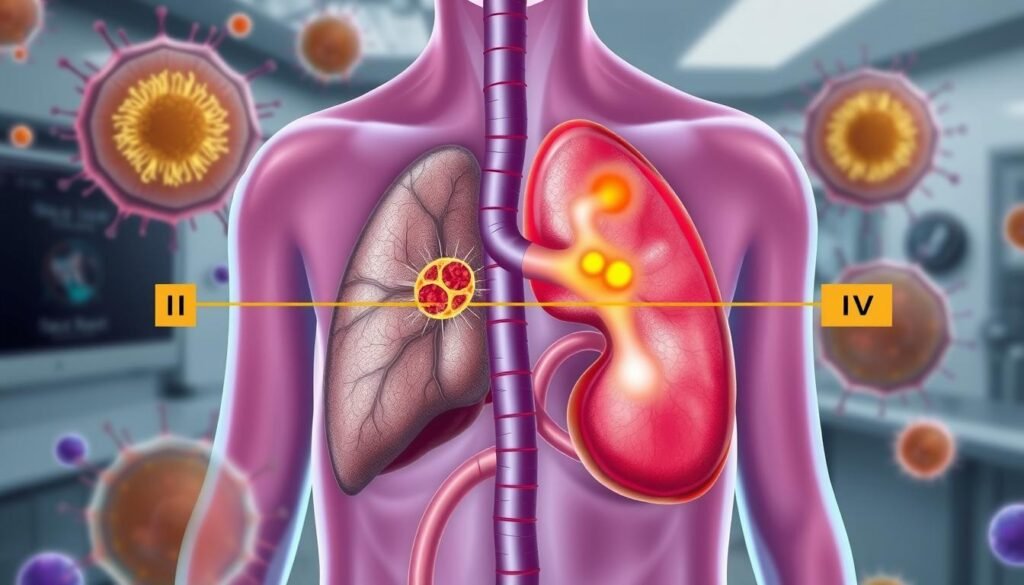
Survival Rates for Different Stages
Survival rates for LCC differ greatly depending on how far the cancer has spread. For LCC patients, here are the median survival times:
| Stage | Median Overall Survival (Months) |
|---|---|
| Stage I | 42 |
| Stage II | 22 |
| Stage III | 11 |
| Stage IV | 3 |
These numbers show why catching cancer early matters. People with cancer that hasn’t spread too far have a 63% chance of living five more years. If the cancer has spread nearby, that chance drops to 35%. For those with cancer in distant parts, the chance is just about 7%.
Factors Influencing Prognosis
Many things matter in figuring out the outlook for lung cancer. Some important things that affect it include:
- Tumor Stage: Finding cancer early helps survival chances a lot.
- Patient Age: Around 40% of LCC patients are over 70, which makes treatment trickier.
- Gender: Out of all patients, 59.1% are males and 40.9% are females.
- Treatment Modalities: Using surgery and chemo together tends to work better than just surgery.
- Metastatic Patterns: Cancer spreading to bones, brain, lungs, and liver in stage IV affects survival badly.
- Performance Status: Being in poor health or losing a lot of weight makes treatment less effective.
Knowing these factors helps patients and doctors choose the best treatment plan. The goal is always to improve how long patients can live.

Treatment Options for Large Cell Carcinoma
There are many treatments for large cell carcinoma. The choice depends on the patient’s health, cancer stage, and tumor traits. Knowing the options helps patients decide on their treatment.
Surgical Interventions
Surgery is key for treating large cell carcinoma in early stages. Common surgeries include:
- Wedge resection: Removing a small part of the lung with the tumor.
- Lobectomy: Taking out a whole lung lobe.
- Pneumonectomy: Removing a lung completely.
- Sleeve resection: Cutting out part of the airway with the tumor.
These surgeries aim to remove the tumor fully. They greatly improve the patient’s survival chances.
Chemotherapy Approaches
Chemotherapy uses drug combos to kill cancer cells. The treatment adjusts based on how the patient and tumor react. Many patients get both surgery and chemo as it helps fight advanced cancer.
Radiation Therapy for Large Cell Carcinoma
Radiation therapy can be a main or extra treatment. It helps especially with big tumors or advanced cancer. Sometimes, it eases symptoms and improves life quality. Patients often get it alongside surgery.
Targeted Therapy Options
Targeted therapy is an advancing treatment for large cell carcinoma. It attacks cancer cells with less harm to normal cells. New therapies often bring hope to those not helped by standard treatments.
Treatment choices are personalized. The tumor’s location and size, and patient health matter a lot. They help pick the best way to fight large cell carcinoma.
For more details on non-small cell lung cancer treatments, please visit treatment guidelines and insights.
Emerging Treatments and Clinical Trials
New treatments for lung cancer, especially large cell carcinoma, are showing great promise. Thanks to immunotherapy, there is new hope for patients. This method helps the immune system find and destroy cancer cells.
Current research focuses on checkpoint inhibitors, a key factor in lung cancer treatment. These treatments have significantly improved how we care for patients. It’s also important to stay informed about ongoing clinical trials for new treatments.
Immunotherapy Approaches
Immunotherapy tries to make the body’s immune system fight tumors better. Some strategies include:
- Checkpoint inhibitors like pembrolizumab (Keytruda) and nivolumab (Opdivo), which make the immune system attack cancer cells more effectively.
- Combining immunotherapy with chemotherapy, which may help patients live longer.
- Testing new immunotherapeutic drugs in clinical trials to see how well they work.
These methods are part of a move towards custom cancer treatment. It’s all about finding the right therapy for each patient’s situation.
Participation in Clinical Trials
Taking part in clinical trials is crucial for patients with large cell carcinoma. It gives them access to the latest treatments that aren’t widely available yet. Here are some key points:
- Clinical trials test new cancer treatments and compare them with current options.
- They let patients try drug combinations and treatments suited to their needs, possibly improving how well they do.
- By joining a trial, patients help improve our understanding of lung cancer. This can help future patients.
To find out about the latest in lung cancer treatment, patients should talk to their doctors about clinical trials.
Palliative Care and Supportive Treatments
Palliative care aids in improving life quality for lung cancer patients. It focuses on easing symptoms and boosting well-being. A team of doctors, nurses, and social workers offer this care. They work together to provide full support for physical and emotional challenges.
Patients might deal with pain, nausea, fatigue, and trouble sleeping during treatment. They might also feel anxious or depressed. Supportive care helps with these issues by managing pain, improving nutrition, and offering emotional support. This care brings peace and comfort.
Palliative care goes hand-in-hand with other cancer treatments. It doesn’t mean giving up. Studies have found that it can improve mood and might help patients live longer. The American Society of Clinical Oncology suggests all advanced cancer patients should get this care. It’s crucial at any illness stage.
Supportive treatments help open airways, manage pain, and support emotional healing. Patients can get these treatments in hospitals, clinics, or at home. This flexibility helps cater to personal needs and preferences.
Learning about early lung cancer signs is critical. Seeking palliative care early can lead to better symptom management. It’s about improving life quality, not giving up.
The Role of a Multidisciplinary Team
Managing large cell carcinoma needs a team effort. A multidisciplinary team in cancer care comes together for this. Medical oncologists, thoracic surgeons, radiation oncologists, and specialized nurses are part of it. Each one has unique skills. Together, they create detailed treatment plans.
Such teamwork really helps patients, especially with advanced lung cancer. These teams follow top guidelines, speeding up treatment start times. Patients see better survival rates and life quality.
Advanced lung cancer can be tough to tackle. It sometimes leads to issues like sarcopenia, which affects many patients. A team approach helps manage this, improving how well treatments work.
The need for a multidisciplinary team is growing as cancer care advances. Patients get personalized and thorough treatment plans. This teamwork leads to better health results. It also supports patients and their families.
| Team Member | Role in Cancer Care |
|---|---|
| Medical Oncologist | Directs chemotherapy and targeted therapies |
| Thoracic Surgeon | Performs surgical interventions as needed |
| Radiation Oncologist | Administers radiation therapy |
| Nurse Navigator | Guides patients through the healthcare journey |
| Palliative Care Specialist | Manages symptoms and improves quality of life |
Conclusion
Large cell carcinoma, especially the neuroendocrine type, is hard to treat. It needs a deep understanding of its signs and how to manage it. This cancer is rare and aggressive, making up about 3% of all lung cancer cases. People often find out they have it when it’s already advanced, leading to lower chances of survival.
Studies show that chemotherapy is the best way to treat it. A special tool called a nomogram model helps predict how patients might do. It shows why having a detailed plan for care is vital.
Research into immunotherapy is giving us hope. It’s part of a bigger effort to get better at treating lung cancer. Making progress in personal treatment plans is key. These plans need to take into account the unique aspects of LCNEC, which affect how well treatment works.
The overall picture shows that teamwork and continuous support are crucial. They help patients get the best possible care. This strategy helps those facing this tough diagnosis. It aims to increase their chance of survival and improve their life quality.