About 41.4% of patients face problems after having a pneumonectomy. This surgery removes a lung completely. It’s done for serious issues like lung cancer and bad lung infections. Knowing when you need this operation could save your life.
We’ll look at why some patients need their lung taken out. We will explore what the surgery involves, the risks, and how people recover. This operation is a big deal. It’s especially tough when your lungs aren’t working well. But, with careful planning, a pneumonectomy might be just what’s needed for critical lung problems.
Key Takeaways
- Pneumonectomy is a major surgery typically performed for conditions like lung cancer.
- Postoperative complications occur in over 41% of patients who undergo this procedure.
- A significant number of patients are elderly or have pre-existing cardiovascular issues.
- Preoperative evaluations are essential to minimize risks and improve surgical outcomes.
- Understanding the indications is vital for determining when pneumonectomy is the best option.
- Recovery from pneumonectomy may involve lifestyle changes and ongoing medical supervision.
Understanding Pneumonectomy
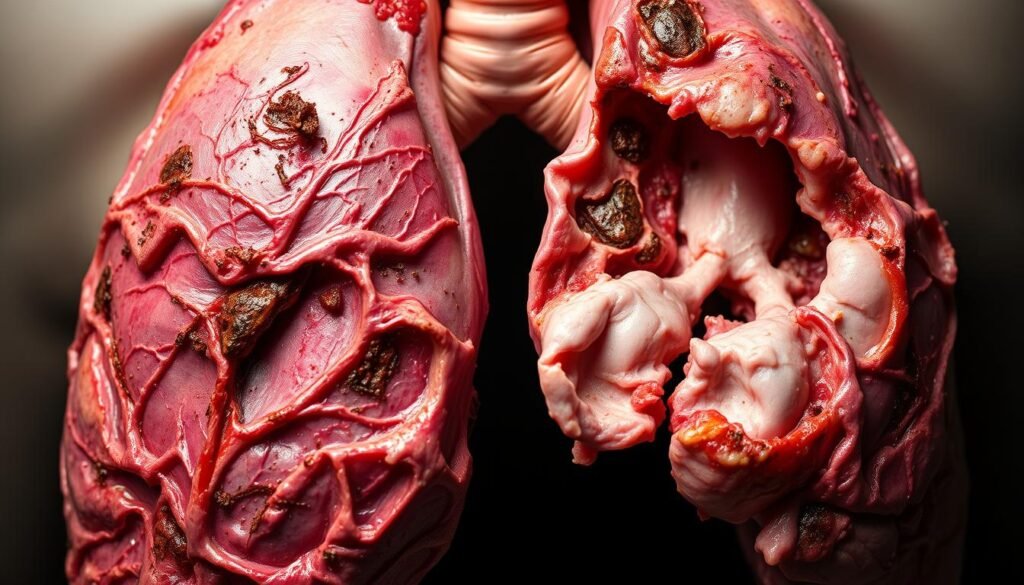
Pneumonectomy is the surgical removal of a lung. It’s mainly done to treat severe lung issues, like lung cancer. The purpose of pneumonectomy is to improve life quality. It removes sick lung parts that hurt lung function. This surgery takes a lot of planning because losing a lung changes the body a lot.
Definition and Purpose
The pneumonectomy definition is simple: it’s a big surgery to take out a lung. This could be because of cancer or other serious conditions. The goal is to stop the patient’s health from getting worse and to make breathing easier. Before the surgery, doctors check the patient carefully. They make sure the patient knows what will happen and what risks are involved.
Procedure Overview
The surgery starts with a thoracotomy. This means the surgeon cuts into the chest to reach the lung. This cut lets the surgeon remove the left or right lung. Sometimes, they might use video-assisted thoracoscopic surgery (VATS). VATS is less invasive and is used mainly for tumors that are not very advanced. Before surgery, the patient goes through many tests. These tests check if the surgery is a good option.
After the surgery, there’s a lot of focus on managing pain and recovery. Surgeons look out for risks like breathing problems, bleeding, and infections. Good care after surgery is key. It helps the patient get used to living with one lung.
For more details on pneumonectomy, click here.
Common Indications for Pneumonectomy
Pneumonectomy is a surgery that takes out an entire lung. This operation is needed for several health problems. Each case brings different challenges and thoughts on how to best care for the patient.
Lung Cancer
Lung cancer is the most common reason for this surgery. If the tumor is in the middle of the lung, usual treatments might not work. Then, surgery is crucial to remove the cancer and help the patient live longer.
This surgery gets rid of harmful tumors. This step increases recovery chances and helps extend the lives of those affected.
Pulmonary Infections
Severe lung infections, like bad tuberculosis or ongoing fungal infections, can harm the lung beyond repair. When a lung stops working well, removing it through surgery can be necessary. This helps stop more health issues from happening.
Getting surgery for lung infections can really help make life better for those with chronic breathing problems.
Congenital Lung Abnormalities
Some people are born with lung issues that make breathing hard. Diseases like bronchiectasis destroy lung tissue and may need a pneumonectomy to fix. This surgery is critical for improving breathing and avoiding worse problems later.

| Indication | Description |
|---|---|
| Lung Cancer | Primary malignant tumors that require removal for effective treatment. |
| Pulmonary Infections | Severe infections causing irreversible lung damage. |
| Congenital Lung Abnormalities | Structural lung issues leading to impaired respiratory function. |
Indications for Pneumonectomy
Pneumonectomy may become crucial in certain medical conditions that severely compromise lung function. Such conditions include lung trauma, pulmonary fibrosis, and tuberculosis complications. These can lead to life-threatening health issues, requiring surgery. Pneumonectomy aims to restore lung capacity and improve the patient’s quality of life.
Severe Lung Damage from Trauma
Lung trauma can result from accidents or injuries. It causes significant damage, impairing breathing and lung function. When the lung is beyond repair, pneumonectomy can protect the healthy lung tissue. This surgery is vital for those with acute respiratory distress from trauma.
Pulmonary Fibrosis and Other Chronic Conditions
Pulmonary fibrosis scars lung tissue, leading to a major drop in function. Chronic lung diseases add to this trouble. Pneumonectomy is an option when other treatments don’t help. It removes the damaged lung, improving breathing and life quality.
Tuberculosis Sequelae
After treating tuberculosis, some patients have scarring and remaining infection. These can still harm lung function. Pneumonectomy may be needed to remove diseased tissue and stop further health problems. This surgery is key to regaining health and lung function.
| Condition | Indication for Pneumonectomy | Potential Outcome |
|---|---|---|
| Lung Trauma | Severe damage, impaired function | Restored lung capacity, reduced complications |
| Pulmonary Fibrosis | Chronic lung disease progression | Improved breathing, enhanced quality of life |
| Tuberculosis Sequelae | Residual disease and infection | Health restoration, reduced lung complications |
Evaluating the Need for Pneumonectomy
Doctors assess if pneumonectomy, or lung removal, is necessary by looking at each patient’s needs. They look for other, less risky surgical options to help the patient recover better. It’s best to keep as much lung as possible.
When Other Surgical Options Are Not Viable
Sometimes, less invasive treatments won’t work. This makes a detailed patient health assessment critical. Patients need good lung function to handle the surgery. According to guidelines from the British Thoracic Society in 2001, a patient needs an FEV1 of 2 liters to be a good candidate. If a patient’s %PPO is 60% or above, lung surgery is generally safe.
Assessing Patient Health and History
Doctors need to know about any lung problems a patient has had before. They have found that DLCO levels are a better way to predict surgery risks than FEV1 levels. If a patient’s %PPO FEV1 or DLCO is below 30%, doctors will suggest a special exercise test.

Patients struggling to walk 400 meters on a test are often seen as not fit for surgery. Making a well-informed choice early on, based on these health checks, can really affect the surgery’s success. Recognizing symptoms early and managing them well is crucial for the patient’s health. See more on improving patient health.
The Surgical Process of Pneumonectomy
A pneumonectomy requires careful steps to ensure the patient’s safety and the surgery’s success. The first step is planning for anesthesia and the surgery. This planning is key to achieving good results.
Anesthesia and Preparation
Before the surgery, patients get anesthesia for surgery. This makes sure they feel no pain during the operation. General anesthesia keeps patients asleep for the entire surgery. Tests like ECGs and CT scans check if patients are ready for surgery.
Procedure Details and Techniques
A cut is made between the ribs to reach the lung in surgery. The surgeon then carefully removes the lung without harming nearby tissues. Important steps are:
- Using a tool to cut the main airway to the right lung.
- Taking out the lung, lymph nodes, and tissues around them.
- Fixing the diaphragm and heart covering with special materials.
- Checking the surgery’s success with daily X-rays.
After the surgery, patients might need tubes to remove fluid. With good preparation and surgery, patients can start to recover. For more info on pneumonectomy, check this detailed guide.
Risks and Complications Associated with Pneumonectomy
Anyone thinking about getting a pneumonectomy should know the risks. Like all major surgeries, a pneumonectomy can lead to several complications. These problems can show up right after surgery or even later on.
Understanding the Potential Risks
The death rate for this surgery is about 4.17%, and the chance of having problems is 41.6%. You might have breathing troubles, such as acute respiratory failure (1.2%), pneumonia (10.1%), or bronchopleural fistula (4.17%). Also, almost half of the patients (46%) may get heart rhythm problems like atrial fibrillation.
Being older, or not in great shape before surgery, increases your risk. These factors make it harder for your heart and lungs.
Long-term Complications and Recovery
Recovery from a pneumonectomy can take a long time, from weeks to months. Patients might feel pain where they were cut and find it hard to breathe as well. If you have heart disease or your breathing test scores drop, you might have more trouble getting better.
After surgery, your chest X-rays will usually show fluid build-up. This usually fills up the space in about four months. Knowing about these potential problems helps in dealing with them during recovery.
The Role of Pneumonectomy in Lung Cancer Treatment
Pneumonectomy is crucial for treating lung cancer, mainly when tumors can’t be removed with simpler methods. It removes an entire lung and is key for improving survival for some patients. Knowing how pneumonectomy works in treatment plans is vital for both doctors and patients.
How Pneumonectomy Fits into Treatment Plans
Pneumonectomy is often essential for treating non-small cell lung cancer (NSCLC). The 5-year survival rates change based on the cancer stage:
| Stage | 5-Year Survival Rate |
|---|---|
| Stage I | 44% |
| Stage II | 37.5% |
| Stage III | 29% |
About 30% of NSCLC patients might get surgery to try and cure them. Despite its benefits, it’s crucial to know all treatment options. After surgery, survival rates are between 21% and 31%. Treatment must be customized to the patient’s specific health and tumor type.
Pros and Cons for Patients
Like all surgeries, pneumonectomy has its good and bad sides. The benefits include:
- Increased survival rates for localized lung cancer.
- Potentially curative outcomes with follow-up therapies.
- Complete removal of sick lung tissue, lowering recurrence risk.
However, there are downsides to consider.
- Long recovery time and hospital stays.
- Risks like breathing problems and less lung function.
- The emotional toll of a major surgery.
Patients should weigh these pros and cons when deciding on treatment. In-depth talks with healthcare teams are crucial for personalized lung cancer care.
Pneumonectomy Recovery: What to Expect
Recovery from pneumonectomy means closely managing your health. Patients usually stay in the hospital for 7 to 10 days. Doctors watch vital signs closely for a safe recovery. Managing pain is also important.
Patients may need breathing treatments and extra oxygen. This helps avoid complications like infections or blood clots. It’s a key part of getting better.
Post-Operative Care and Management
After surgery, care focuses on helping you recover. Walking daily and using a spirometer help lung function. It’s important to follow all medical advice.
Don’t lift heavy things or do hard activities for months. Let your healthcare providers know if you feel anything unusual. This will help you heal well.
Rehabilitation and Lifestyle Changes
Life after surgery requires some changes. Eating well helps you recover. Adding exercise, as you can, improves health and lung strength. Learning about your recovery helps you take part in your rehab.
These changes and keeping up with doctor visits help you return to daily life. They ensure a better health future.
Conclusion
Pneumonectomy is key for those with serious lung issues, especially lung cancer. This surgery can greatly improve health despite its risks. Studies show that while risks are higher, the right patients see a boost in survival time. For example, those with the same tumor type in different surgeries lived longer (48 months).
It’s vital for doctors and patients to talk about pneumonectomy carefully. They should consider personal health and how recovery will go. Understanding what it means to remove a lung helps patients decide based on their life goals.
Pneumonectomy will stay important as surgical methods and aftercare improve. Looking at all evidence helps patients get the best care for their situation. For more information on pneumonectomy results, check the studies here.