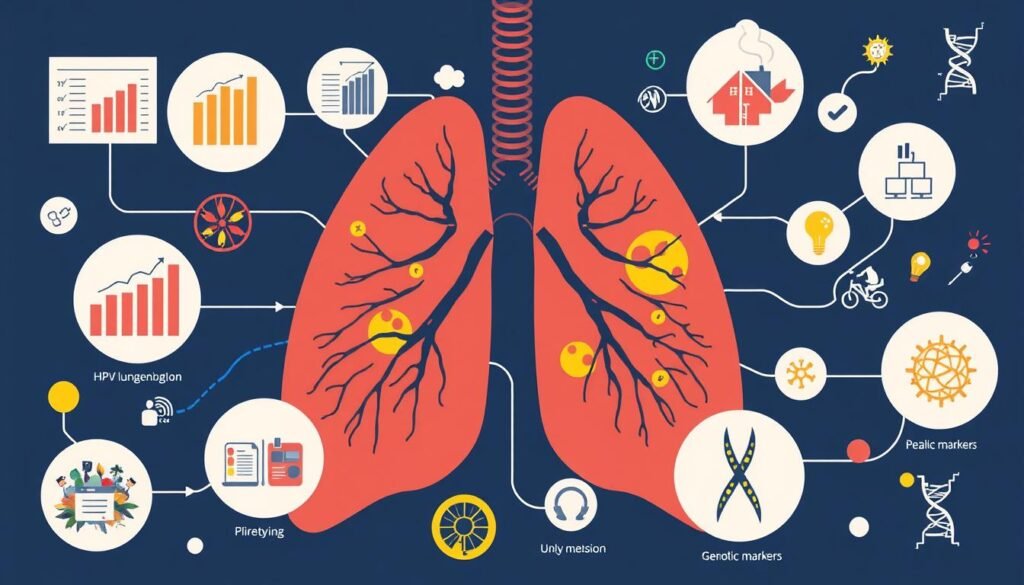
Lung adenocarcinoma patients with HPV infection have a better chance of survival, with a hazard ratio of 0.69. This data shows how HPV can affect lung cancer outcomes, an area that researchers are looking into more. Knowing how HPV links to lung cancer is key for patients and their families.
This piece shares important info on lung cancer related to HPV. It covers survival stats, treatment choices, and what might come next in research. With HPV playing a big role in lung cancers, those in healthcare need to stay informed. This can change how they care for people who are sick.
Key Takeaways
- HPV infection in lung adenocarcinoma patients shows a marked survival benefit.
- Understanding HPV-related lung cancer can lead to better patient outcomes.
- Median overall survival for HPV-positive patients treated with immunotherapy is notably prolonged.
- Variabilities in survival rates are influenced by numerous factors, including HPV status.
- Ongoing research aims to clarify the role of HPV in lung cancer and improve treatment strategies.
- Comparative studies indicate better response rates in HPV-positive patients.
Understanding HPV and Lung Cancer
Human papillomavirus (HPV) is mainly seen with cervical and head and neck cancers. Yet, it might also impact lung cancer. This virus could play a big role in causing lung cancer. Lung cancer is a top reason for cancer deaths globally. Each year, it leads to a lot of illness and death. Besides smoking and pollutants, HPV’s role in lung cancer is gaining attention.
Studies show that HPV is common in people with lung cancer. About 22% of lung cancer patients have HPV. This shows the virus’s effect on the cancer’s growth. People with high-risk HPV types, like HPV 16 and 18, might get lung cancer more often. They are three times and twice as likely, respectively, to develop lung cancer. Also, non-smokers with HPV have a higher lung cancer risk than smokers.
| HPV Type | Increased Risk of Lung Cancer |
|---|---|
| HPV 16 | 3 times more likely |
| HPV 18 | 2 times more likely |
HPV’s link to lung cancer varies by location. In China, 37.7% of lung cancer cases are due to HPV. But in North America, it’s much lower at 12.5%. This shows how HPV and cancer risks differ around the world. It’s more common in Asian populations than in American and European ones.
The CDC recommends the Gardasil 9 vaccine to prevent HPV-related cancers. It targets people from ages 9 to 26. While cervical cancer can be detected early, lung cancer is harder to find. It’s vital to understand how HPV affects lung cancer. This can help improve how we look after patients. More details on the link between HPV and lung cancer can be found in this study.
The Connection Between HPV and Lung Malignancies
Doctors are studying how HPV might lead to lung cancer. They’ve found strong evidence that HPV can cause lung malignancies. This has sparked talks about how it affects lung cancer outlooks. A key study showed HPV infection makes lung cancer more likely by 3.64 times.
Different studies show varied results. Studies with unrelated people found a very high link, showing a 6.71 times increase. But in studies where people are compared to themselves, the risk was lower, at 2.59 times. Studies within the same group of people showed almost no link, with a 0.92 times increase.
It turns out certain HPV types, like 16 and 18, are mostly to blame. They increase lung cancer risk by 3.14 and 2.25 times, respectively. Specific types of lung cancer, such as squamous cell and adenocarcinoma, are also closely linked to HPV.
Looking at where cases happen adds to the puzzle. Out of almost 7,000 cases, most were in Europe, and a big portion was in Asia. A study in China found that HPV increases lung cancer risk in women, but not in men. This shows how complex the relationship between HPV and lung cancer is.
More research is crucial to fully understand HPV’s role in lung cancer. Future studies might explain why it happens, how it changes patient results, and ways to treat HPV-related lung cancer.
| HPV Type | Pooled Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Overall HPV | 3.64 | 2.60–5.08 |
| HPV 16 | 3.14 | 2.07–4.76 |
| HPV 18 | 2.25 | 1.49–3.40 |
| Allogeneic Case-Control Studies | 6.71 | 4.07–11.07 |
| Self-Matched Case-Control Studies | 2.59 | 1.43–4.69 |
| Nested Case-Control Studies | 0.92 | 0.63–1.36 |
HPV Lung Cancer Survival Rate: What the Data Shows
Research shows lung cancer outcomes vary by HPV status. This knowledge can guide treatment choices. It helps patients make smart decisions about their health.
Overview of Survival Statistics
Lung cancer survival stats offer insights into HPV’s impact. A thorough review of studies looked at survival rates linked to HPV. It found no big difference in survival between HPV-positive and negative patients.
However, people with lung adenocarcinoma and HPV had better survival rates. Their survival hazard ratio was more favorable. This means they were more likely to survive than those without HPV.
Comparative Analysis of HPV-Positive and HPV-Negative Patients
When we compare HPV lung cancer outcomes, results vary among different groups. HPV affects certain lung cancer types more. Studies showed adenocarcinoma patients with HPV had improved outcomes.
This highlights how HPV status affects survival in certain cancers. It shows the importance of detailed analysis in treatment planning.
Factors Affecting HPV Lung Cancer Prognosis
It’s vital to grasp how certain factors impact HPV-related lung cancer outcomes. Pathological types and treatment strategies are key. They help predict the survival rate of patients with HPV lung cancer. Let’s delve into how these elements affect patient survival chances.
Pathological Types and Survival Outcomes
When it comes to survival, the type of lung cancer matters a lot. Studies show that patients with HPV-positive adenocarcinoma tend to live longer than those with squamous cell carcinoma. Knowing this difference is crucial. It helps doctors decide on the best treatment options and discuss prognosis with patients.
Impact of Treatment Methods on Survival Rates
The way HPV-positive lung cancer is treated significantly affects patient outcomes. Patients undergoing non-surgical treatments often have better survival rates. It’s important to carefully consider all prognostic factors. This ensures the chosen treatment plan boosts survival chances for HPV lung cancer patients.
| Pathological Type | Survival Outcome | Typical Treatment |
|---|---|---|
| HPV-Positive Adenocarcinoma | Improved survival | Targeted therapy, chemotherapy |
| Squamous Cell Carcinoma | No significant survival benefit | Surgery, radiation therapy |
Understanding these factors in HPV lung cancer prognosis aids in treatment planning. It also helps set patient expectations and guides future studies.
HPV-Related Lung Cancer: Epidemiology Insights
Studies have revealed important facts about HPV and lung cancer. They show how common HPV is in lung cancer cases. This helps us know who might be more at risk and look for cancer early on.
Prevalence of HPV in Lung Cancer Cases
About 20% of lung cancer tests find HPV DNA. The rate is different depending on where you live. Asia has high rates of HPV in lung cancer cases.
For example, 31.3% of Koreans with lung cancer had HPV subtype 33. Women who have never smoked and get HPV are more likely to get lung cancer. Their risk goes up by more than five times.
Regional Variations in HPV Incidence and Lung Cancer
Where you live can affect your HPV risk and lung cancer rate. Research often looks at women and people who don’t smoke. Lung cancer is becoming more common in these groups.
HPV’s impact is stronger in certain places, like Asia and Latin America. These findings show we need better screening and prevention in areas with more HPV.
| Region | HPV Detection Rate in Lung Cancer | Notable Observations |
|---|---|---|
| Korea | 31.3% | High prevalence of HPV subtype 33 |
| General Asian Population | Higher than global average | Significant odds ratio in studies |
| Latin America | Varies by country | Increased focus on HPV-related cancers |
HPV-Positive Lung Tumors: Characteristics and Challenges
HPV-positive lung tumors have unique lung cancer characteristics. In a study of over 7,000 cases, 22.4% were HPV-positive. This number has grown to 24.5% from earlier studies. HPV-16 is the most common type found in these cases.
These tumors react differently to treatments. The effectiveness of a treatment can depend a lot on a person’s immune response to HPV. This makes diagnosing and treating these cancers challenging. Problems arise because their symptoms can look like those of other cancers. To learn more about treating these cancers, check out this guide on radiation therapy for lung cancer.
It’s important for doctors to understand HPV-positive lung tumors well. This knowledge can help create better treatments for patients. By knowing what makes these tumors unique, doctors can offer more specific and effective care.
| Characteristic | Details |
|---|---|
| HPV Prevalence in Lung Cancer | 22.4% from analyzed samples |
| Types of HPV | HPV-16 is the most common strain |
| Impact on Treatment | Varies with host immune response |
| Diagnostic Challenges | Overlap in symptoms with other lung cancers |
| Research Considerations | A need for tailored treatment approaches |
Current Treatment Approaches for HPV Lung Cancer
HPV lung cancer treatment is complex and involves multiple standard protocols. The usual care path includes surgery, chemo, and radiation. Each treatment plays a part in fighting this disease, considering the special issues HPV tumors cause.
Standard Treatment Protocols
The first steps in treating HPV lung cancer generally include:
- Surgical Resection: This surgery removes tumors and parts of the lung.
- Chemotherapy: This treatment uses drugs to kill cancer cells in the body.
- Radiotherapy: This method shrinks tumors and kills cancer cells after surgery.
These treatments are key to better outcomes for patients. At the same time, new treatments are being studied.
Novel Therapies and Clinical Trials
New therapies for HPV lung cancer are changing how it’s treated. Immunotherapy, for example, uses our immune system to fight cancer. It’s showing potential for HPV-positive patients. Clinical trials are testing different immunotherapy methods to see their effects.
| Clinical Trial Focus | Phase | Status |
|---|---|---|
| Pembrolizumab with Chemotherapy | Phase 2 | Completed |
| HPV-specific Immunotherapies | Phase 1 | Recruiting |
| Combination Treatments | Phase 3 | Ongoing |
Clinical trials aim to improve treatments and boost survival rates for HPV lung cancer patients.
The Role of Immunotherapy in HPV Lung Cancer Treatment
Immunotherapy plays a key role in fighting lung cancer linked to HPV. Studies show that HPV-positive lung cancer patients respond better to immunotherapy. This can lead to higher survival rates compared to HPV-negative patients. Scientists are studying why this happens, focusing on the immune system’s role in the body.

Immunotherapy alone hasn’t cured metastatic HPV-related cancer. But, it’s helping to slow down the cancer’s growth. When used with other treatments like chemotherapy, outcomes improve. For instance, treatments that use monoclonal antibodies have fully helped 20% of patients with different cancers.
There are ongoing studies for cancers caused by HPV. One study involved 43 people with advanced cancers. Impressively, 39% of those with HPV-positive tumors responded well to treatment. This suggests that specific treatments could greatly improve survival. These people lived an average of 16.2 months longer, a big improvement from past studies.
New treatments like bintrafusp alfa are showing promise against HPV cancers. This drug has been tested in almost 700 patients. It aims to treat a wide range of cancers. This highlights how important immunotherapy is in cancer care today.
To learn more about new treatments, check out the latest on HPV lung cancer treatment outcomes.
Lung Cancer Survival Statistics for HPV: A Closer Look
Lung cancer survival stats show how well treatments work based on HPV status. For non-small cell lung cancer (NSCLC), survival rates change with how early it’s found. Localized cases have a survival rate of 65%, while regional cases are at 37%.
Distant-stage cases have only a 9% survival rate, showing a big difference. Combining all stages, the survival rate is about 28%.
Comparing Non-Small Cell Lung Cancer Survival Rates
The SEER database shows differences in survival between HPV-positive and HPV-negative lung cancer patients. A review of nine studies found HPV status to be an important sign, especially in lung adenocarcinoma. HPV infections were connected to a hazard ratio of 0.69, hinting at better survival for these patients.
Identifying Risk Factors with Better Outcomes
Knowing which risk factors lead to better outcomes helps make treatment fit the patient better. Age, cancer stage, and HPV status are key. Recognizing these factors helps doctors make customized treatment plans, possibly improving survival rates.
The type of treatment can greatly affect survival rates too. Non-surgical options, for example, might show different results in the overall data.
| Cancer Type | Localized Survival Rate | Regional Survival Rate | Distant Survival Rate | All Stages Combined |
|---|---|---|---|---|
| NSCLC | 65% | 37% | 9% | 28% |
| SCLC | 30% | 18% | 3% | 7% |
Patient Stories: HPV Lung Cancer Survival Experiences
People share their patient stories to offer insights into dealing with HPV lung cancer. They talk about their challenges and the strength needed to face this disease.
A young woman shares her battle with cervical cancer and the radical surgery she endured. Her story highlights how crucial early detection and individualized treatments are. Such stories can inspire others going through similar battles.
People of various ages share their HPV lung cancer experiences, from teens to middle-aged adults. A 42-year-old marketing professional, Alastair McCausland, shares his journey.
He talks about the effect of cancer on family and personal well-being. His story shows how cancer can disrupt both work and home life.
- Significance of early detection, similar to Louise’s breast cancer discovery through screening.
- Innovative treatment approaches, evidenced by Dennise’s experience with targeted therapies.
- The emotional toll, as seen in Samantha’s story of loss and growth following a melanoma diagnosis.
The narratives often highlight how HPV links to different cancers, like throat cancer. This raises awareness about prevention and the need for vaccinations.
Community support through fundraising and volunteering shines through in these stories. Greer Worsley, for instance, emphasizes how community action can bring about change and raise awareness.
Sharing these patient stories brings people together, creating a community of support and hope. It encourages others to seek help and follow their recovery journey.
To learn more about lung cancer treatments, it’s good to stay updated. Check out this resource for the latest information.
Future Directions in HPV Lung Cancer Research
Research into HPV-related lung cancer is growing fast. It’s uncovering new details about the disease, like how it acts, treatment options, and how common it is. Knowing what to study next is key to see how HPV and lung cancer affect people.
Emerging Trends and Clinical Implications
Modern studies are diving into all parts of HPV lung cancer. They look at how the disease works and the impact of treatments. The study of new trends has shown how important prevention, like vaccines and checks, is. Also, there’s a push towards new treatments, including gene editing with CRISPR/Cas, to make therapies better.
The Need for Comprehensive Studies
Broad studies on the lasting effects of HPV cancers are vital. They work to see how long people live after treatment and how they respond to it. This forms a guide to better care for patients. Grasping HPV lung cancer patterns helps plan future treatments and health efforts. A deep look into how often and where HPV lung cancer happens helps us understand its big-picture impact. For more info, check out the article here.
Conclusion
Understanding the survival rate of HPV lung cancer is key for guiding patients and healthcare workers. Studies show that patients with HPV tend to live longer than those without. Factors like age, smoking, the stage of cancer, and treatments also play a big role.
Continued research is opening up new ways to treat this disease and improve care. This highlights the need for more awareness about HPV’s impact on lung cancer. It points to the importance of personalized treatment plans. As research grows, so does the chance for better outcomes for patients with HPV-related cancers.
Talking more about HPV and lung cancer helps support those affected. It helps guide them towards a future with better survival rates. This brings hope in dealing with a tough diagnosis.