Lung cancer is the top cause of cancer death worldwide. Treatments have gotten better, helping people live longer. Knowing the difference between pneumonectomy and lobectomy is key. This knowledge helps patients and doctors make the best surgery choices. It’s all about finding the right treatment for each person’s situation.
Key Takeaways
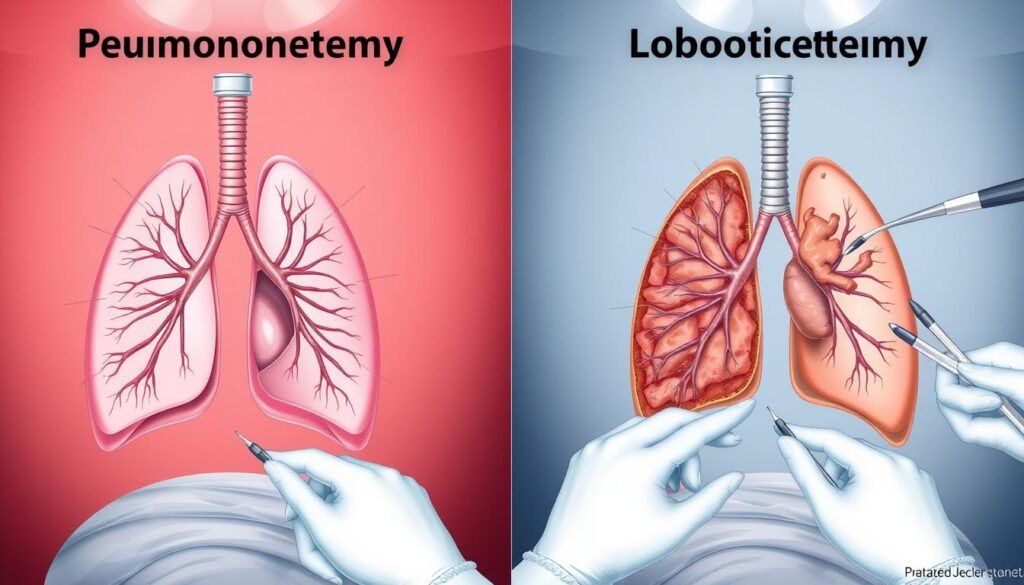
- Pneumonectomy involves the complete removal of one lung, while lobectomy removes only one lobe.
- Lobectomy is the most common surgery for early-stage lung cancer confined to one lobe.
- Understanding the type of lung tissue removed impacts recovery and treatment plans.
- Both surgical options come with unique risks and recovery expectations.
- Minimally invasive techniques are increasingly being used in lung cancer surgeries.
Overview of Lung Cancer Surgeries
Lung cancer surgery is key in treating different types of lung cancer, especially non-small cell lung cancer (NSCLC). There are several surgery options, like lobectomy, pneumonectomy, segmentectomy, and wedge resection. Each one aims at removing the sick parts of the lung to help improve a patient’s outlook.
Lobectomy surgery removes a section of the lung that has a tumor. It’s the go-to method if the cancer hasn’t spread much. Pneumonectomy involves taking out a whole lung and is used for tumors in the middle of the lung. Segmentectomy or wedge resection are for taking out small parts of the lung and are less extreme options.
Using less invasive surgeries like video-assisted thoracoscopic surgery (VATS) and robotic-assisted thoracoscopic surgery (RATS) is becoming more common. These techniques have big benefits like quicker healing, smaller cuts, and fewer complications after surgery than the standard thoracotomy, which has larger cuts. What surgery a patient gets depends on many things, like how big and where the tumor is and the patient’s lung health.
Tests to check lung function before surgery are very important. They help doctors decide which surgery method is best. After surgery, treatments like physical therapy and pulmonary rehab are often suggested. They help patients recover faster and make their lungs stronger.
Pneumonectomy: Definition and Indications
Pneumonectomy is a major surgery that removes a whole lung. It is mainly for severe lung damage patients, like those with lung cancer. This surgery is considered when other treatments fail, especially for tumors in the lung’s center.
What is a Pneumonectomy?
A pneumonectomy is a key option for treating serious respiratory conditions. It involves taking out an entire lung. This may be crucial for people with advanced lung cancer, severe lung injuries, progressive pulmonary tuberculosis, or intense bronchiectasis. The operation requires general anesthesia. It can be done through open chest surgery or using VATS (video-assisted thoracoscopic surgery) for early-stage tumors near the lung’s surface.
Conditions Treated with Pneumonectomy
- Lung cancer, particularly non-small cell lung cancer (NSCLC)
- Traumatic lung injury
- Advanced pulmonary tuberculosis
- Fungal infections affecting lung tissue
- Severe cases of bronchiectasis
- Congenital lung diseases
- Bronchial blockages leading to lung destruction
Lobectomy: Definition and Indications
Lobectomy is a key surgery in treating lung cancer, specifically removing one lung lobe. It is often chosen for early-stage lung cancer. The goal is to stop the cancer from growing while keeping as much healthy lung as possible.
Understanding Lobectomy
Dr. Davies first did this surgery in 1913. Since then, there have been many improvements. Better surgeries, anesthesia, and ways to control infections have helped patients recover better.
The introduction of video-assisted thoracoscopic surgery (VATS) has changed lobectomy. VATS is less invasive than older methods. It also has fewer risks, making it a top choice for treating early lung cancer and some benign lung issues.
When is Lobectomy Recommended?
Lobectomy is recommended for several lung problems, including:
- Early-stage lung cancer
- Tuberculosis
- Lung abscess
- Emphysema
- Benign tumors
- Fungal infections
The decision for lobectomy depends on the tumor’s size and location. Surgeons aim to remove the right lobe to get the best results while reducing risks. After the surgery, patients stay in the hospital for a bit. They must follow a careful plan to heal well.
Pneumonectomy vs. Lobectomy: Key Differences
Choosing between pneumonectomy and lobectomy involves knowing what lung tissue is removed. It also involves the recovery needed afterwards. Each surgery has unique features that decide if a patient can have it. They also affect how the patient recovers.
Type of Lung Tissue Removed
Pneumonectomy means taking out a whole lung on one side. This is more extensive than a lobectomy. Lobectomy removes part of a lung, usually one or more lobes. It’s less invasive. Surgeons look at lung function, like FEV1 and DLCO, to decide the best surgery. Lobectomy patients need a post-operative FEV1 over 1.5L. Pneumonectomy patients need an FEV1 over 2L.
Indications for Each Procedure
The reasons for these surgeries are different. Pneumonectomy is for certain lung cancer stages where removing the entire lung is best. Lobectomy is chosen for early-stage lung cancer or limited lung disease. The patient’s health, like exercise ability and oxygen levels, is key in deciding the surgery.
Recovery Outcomes
Recovery from pneumonectomy usually takes longer, about five to seven days in the hospital. This is because it’s a bigger surgery. Lobectomy has a quicker recovery and needs less monitoring after the surgery. Knowing these differences helps in making informed choices and planning care after surgery.
| Parameter | Pneumonectomy | Lobectomy |
|---|---|---|
| Type of Lung Tissue Removed | Entire lung on one side | One or more lobes |
| Indications | Stage 1 small cell lung cancer, Advanced stage non-small cell lung cancer | Stage 1 and stage 2 non-small cell lung cancer |
| Post-operative FEV1 Requirement | Greater than 2L | Greater than 1.5L |
| Average Hospital Stay | 5 to 7 days | Shorter duration |
| Recovery Monitoring | Extensive | Less intensive |
Pneumonectomy Differs from Lobectomy: Surgical Techniques
There are big differences in how surgeries for lung cancer, like pneumonectomy and lobectomy, are done. They include open surgery and less invasive methods. Knowing about these helps doctors choose the best care for patients.
Open Surgery vs. Minimally Invasive Techniques
Open surgery requires large cuts for doctors to access the lung. This traditional method leads to longer healing times and more pain after surgery. It also raises the risk of complications during recovery.
On the other hand, minimally invasive surgeries like VATS are becoming more popular. VATS involves small cuts and special tools. This method means less pain and quicker recovery for patients. For example, studies show VATS reduces bleeding during surgery. It’s important to pick the right surgery method for each patient to get the best results.
Role of Thoracotomy and Video-Assisted Thoracoscopic Surgery (VATS)
Thoracotomy is an open surgery often used for pneumonectomy. It can make recovery hard for patients. VATS, however, is a newer, less invasive approach. It allows surgeons to operate more precisely with less harm to the body. VATS is changing how doctors perform surgery, making the recovery easier for patients.
Different surgeries, like open and minimally invasive techniques, have their own benefits depending on the patient. It’s important to look at the patient’s age, health, and tumor details. Choosing the right surgery gives better results and highlights the need for personalized medical care.
| Surgical Technique | Invasive Level | Recovery Time | Postoperative Complications |
|---|---|---|---|
| Open Surgery | High | Longer | Higher |
| Minimally Invasive Techniques (VATS) | Low | Shorter | Lower |
By comparing these methods, medical experts can choose the best surgical process for lung cancer. This decision affects both the patient’s immediate and long-term health. It also focuses on improving life quality through careful surgery choice.
For more details on how these surgeries affect patients, check this study. It offers insights into why personalized surgery options can lead to faster recovery and higher survival rates.
Recovery Process after Pneumonectomy
The recovery after a pneumonectomy can be tough but it’s crucial for your health. Patients see different effects after this major surgery. Knowing what to expect is important for being ready for the recovery journey.
Short-term Recovery Expectations
The beginning of recovery usually means a stay in the hospital. This lets doctors keep an eye on you. They work to manage your pain and stop infections. It’s common to feel short of breath for up to six months after.
Some people can go back to light work within eight weeks, if they have no complications. Following a rehab program closely can help make recovery easier. For more info on pneumonectomy recovery, check out this link.
Long-term Health Implications
Long-term effects after a pneumonectomy are different for everyone. A common change is in lung function, which might impact everyday life. It’s key to have regular check-ups to keep an eye on lung health. Support from healthcare professionals can help tackle any emotional or mental challenges.
Working with various healthcare experts ensures a well-rounded recovery plan. They help with both the physical and emotional aspects of healing.

Recovery Process after Lobectomy
The recovery from a lobectomy tends to be easier than more invasive surgeries like pneumonectomy. Knowing what to expect right after the operation helps patients get through the first days. It also helps them get ready to go back to their usual routines.
Immediate Postoperative Care
Patients are closely watched after the surgery to keep an eye on vital signs and ease pain. The key parts of care after surgery include:
- Pain Management: Medications help reduce any pain.
- Chest Tube Management: A chest tube aids lung expansion and is usually taken out in two days.
- Monitoring for Complications: Doctors watch out for issues like air leaks, more common in patients with emphysema.
- Gradual Activity Increase: Patients are advised to start walking as soon as possible to help with blood flow and lung health.
Return to Normal Activities
The time it takes to get back to normal varies for each person. It depends on their health, the surgery’s complexity, and the surgical method used. Here are some basic recovery timelines:
| Activity | Typical Timeline |
|---|---|
| Light activities (walking, household chores) | 1-2 weeks |
| Returning to work (depending on job type) | 4-6 weeks |
| Strenuous activities (exercise, heavy lifting) | 6-12 weeks |
Many people feel better and have a better quality of life after the surgery. The usual stay in the hospital is six to seven days for a traditional lobectomy. For VATS, which is less invasive, it’s four to five days. Good care after surgery lowers the chance of problems and helps with the recovery.
Risks and Complications Associated with Pneumonectomy
Pneumonectomy is a major surgery with many risks and complications. It’s important for patients to know these challenges before deciding. Issues such as breathing problems, infections, and heart complications are common. This surgery’s complex nature increases the pneumonectomy complications over simpler procedures.
Common Complications
Here are some common complications from pneumonectomy:
| Complication | Incidence Rate |
|---|---|
| Respiratory Failure | 10-20% |
| Pneumonia | 8-15% |
| Bronchopleural Fistula | 1-3% |
| Cardiac Complications | 5-10% |
| Postoperative Stroke | 0.6% |
The 30-day mortality rate for pneumonectomy patients is around 5.86%. This is higher than for those getting a sleeve lobectomy. The mortality rate at 90 days shows the surgical risks of pneumonectomy.
Comparative Risk Factors
Risk factors for pneumonectomy often include being older and having heart problems before. A study shows many patients are diagnosed late (stages IIIA and IIIB). This raises their risk of complications. Here’s a comparison of risk factors for pneumonectomy and sleeve lobectomy patients:
| Risk Factor | Pneumonectomy | Sleeve Lobectomy |
|---|---|---|
| Mean Age | 57.89 years | 60.08 years |
| Proportion of T3 Tumors | 31% | 21.2% |
| Proportion of Advanced Stage Diagnosis (IIIA and IIIB) | 54.8% | 38.7% |
| Mortality Rate (30 Days) | 5.86% | 2.91% |
Understanding all pneumonectomy complications helps patients and doctors make better choices. It’s crucial to talk about these risks and complications with a healthcare team before the surgery.
Risks and Complications Associated with Lobectomy
Lobectomy is often needed for lung cancer treatment. It comes with certain lobectomy risks. Before the surgery, it’s vital for patients to know about the potential side effects. Compared to a pneumonectomy, a lobectomy usually leads to fewer problems. However, knowing these risks is key for making the best decision.
Potential Side Effects
After a lobectomy, between 10% to 50% of patients may face complications. The most common issues include:
- Pneumonia, with a 2.5% chance
- Prolonged air leaks, seen in 15-18% of patients
- Atrial fibrillation, happening in 14.4% of cases
- Reoperation for bleeding, in 1.5% of cases
- Empyema, with a 1.1% rate
Dealing with pain after surgery is common. About 50% to 70% of patients feel pain for over two months. Furthermore, more than 40% report discomfort after a year.
Comparative Analysis of Complications
When comparing lobectomy to pneumonectomy, lobectomy stands out as safer. Its operative mortality rate is about 2.6%. Meanwhile, postoperative deaths, mainly from pneumonia or ARDS, occur in 1.4% of cases. Pneumonectomy, on the other hand, has a 10.1% death rate. This shows lobectomy’s relative safety.
About 21.9% of lobectomy patients see major complications, slightly less than pneumonectomy’s 22.5%. Lobectomy is a good choice for early-stage lung cancer. It often leads to long-term survival without the cancer coming back.
For those considering immunotherapy as an added approach, knowing these risks can be very helpful. It can help in shaping a better treatment plan.
Understanding Oncological Treatments in Relation to Surgery
Lung cancer treatment often involves teamwork, using both surgery and chemotherapy. It’s key to know when to combine these methods to improve patient results.
When is Surgery Combined with Chemotherapy or Radiation?
Surgery is a common choice for treating non-small cell lung cancer with resectable tumors. If the cancer is too spread or the tumors too big, it might not be operable right away. Then, treatments like chemotherapy or radiation are used to shrink the tumors before surgery.
Chemotherapy before surgery can make tumors smaller, which helps the surgery go better. Chemotherapy after surgery might be needed to get rid of any remaining cancer cells.
Benefits of Interdisciplinary Treatment Approaches
Different healthcare experts work together to make tailored treatment plans. This team approach helps lung cancer patients recover better and live longer. For example, mixing surgery with radiation therapy can lower the chance of cancer coming back. This is especially true for patients with positive lymph nodes.
Studies show that managing lung cancer with these team strategies leads to better results. You can learn more from detailed studies about the benefits of well-rounded treatment plans.

Minimally Invasive Techniques in Lung Surgery
Lung surgery has seen major changes thanks to new techniques. These minimally invasive methods, like video-assisted thoracoscopic surgery (VATS), change how doctors treat lung cancer. They use smaller cuts, usually 2-3 inches long, which is less harsh than old methods.
Advancements in Surgical Methods
These new ways of doing surgery have really cut down on recovery time. A study looked at 108 patients. It showed those who had VATS didn’t face more risks than those who had traditional surgery.
Survival rates differ by the type of surgery. Pneumonectomy patients had a median survival of 23.6 months. While those who had sleeve lobectomy lived longer, around 60.7 months. This shows it’s important to choose the right surgery type.
Benefits and Challenges of Minimally Invasive Techniques
Minimally invasive surgeries have a lot of upsides. Patients feel less pain and don’t stay as long in the hospital. They also get back on their feet quicker. There’s no big difference in complications when compared to open surgeries.
But, these methods are not without their challenges. Surgeons need special training and tools. This is crucial for giving patients the best care.
It’s key to understand these advances in lung surgery. Minimally invasive methods have their benefits. Yet, ongoing research is vital. This helps us understand their effectiveness and the hurdles surgeons face.
| Aspect | Minimally Invasive Techniques (VATS) | Open Surgery |
|---|---|---|
| Incision Length | 2-3 inches | 8-10 inches |
| Typical Recovery Time | Shorter | Longer |
| Hospital Stay | 2-5 days | Varies |
| Patient Ambulation Start | 1st or 2nd day | Post Anesthesia Recovery |
| Common Procedures | Lobectomy, Pneumonectomy | Lobectomy, Pneumonectomy |
| Surgeon Training Required | Specialized | Standard Training |
Conclusion
When it comes to surgery for lung cancer, knowing the difference between pneumonectomy and lobectomy is key. Pneumonectomy removes a whole lung and is often used for large, serious tumors. Lobectomy, on the other hand, only takes out a lobe of the lung. This method is usually better for patients, leading to higher survival rates.
Choosing the right surgery is very important and depends on each patient’s unique situation. Things like how old the patient is, the tumor’s size, and its stage play a big role. Nowadays, sleeve lobectomy is becoming more popular. It helps patients recover faster and improves their health after surgery.
This knowledge helps patients and their families make better choices about treatment. They can talk with doctors about what options are best for them. Making informed decisions is crucial for successfully treating lung cancer. It relies on understanding, current research, and new surgical methods.