Did you know that lung cancer causes nearly a quarter of all cancer deaths in the U.S.? This alarming fact shows why we must spread awareness and catch the disease early. It’s vital for patients, their families, and doctors to know how dangerous lung cancer can be. Out of all lung cancer cases, about 85% are called non-small cell lung cancer (NSCLC). The rest are different types, each with its own traits and ways to treat it.
The *lung cancer aggressiveness* can change a lot depending on its type. Small cell lung cancer (SCLC) is seen as the most fierce. This piece looks into how lung cancer is classified, its stages, spread, and how to treat it. Knowing the stats, and symptoms like a constant cough or sudden weight loss, is key. Spotting these signs early can greatly help in fighting the cancer, as shown by lung cancer symptom awareness sources.
Key Takeaways
- Non-small cell lung cancer (NSCLC) accounts for nearly 90% of lung cancer cases.
- Small cell lung cancer (SCLC) is the most aggressive type and comprises about 20% of all cases.
- Smoking is linked to approximately 85% of lung cancer cases.
- Early detection dramatically improves treatment options and chances of recovery.
- Recognizing symptoms like persistent cough and unexplained weight loss is crucial.
- There are several types and stages of lung cancer, each requiring different treatment approaches.
- Understanding lung cancer aggressiveness is essential for better health outcomes.
Understanding Lung Cancer
Lung cancer tops the charts for cancer deaths across the globe. It starts in the lungs and can spread. The term lung cancer definition covers two types: non-small cell (NSCLC) and small cell (SCLC). Smoking is the leading cause of lung cancer, responsible for about 85% of cases.
Others include secondhand smoke, various carcinogens, and genetic risks. Recognizing early lung cancer signs is tough. Early on, patients might not notice symptoms. Signs like a lasting cough, chest pain, tiredness, difficult breathing, and losing weight without trying show up.
These get worse, leading to scary problems like coughing up blood. Smokers are at the biggest risk, but quitting can cut down cancer chances. Being around harmful substances or having a family history also ups the risk. Knowing what causes lung cancer and working to lower risks is crucial.
Checking out resources like this guide helps in grasping lung cancer details. Being informed and catching it early boosts the chance to tackle lung cancer effectively.
| Risk Factors | Impact on Lung Cancer |
|---|---|
| Smoking | Major contributor (85% of cases) |
| Secondhand Smoke | Increases risk significantly |
| Family History | Increased susceptibility |
| Exposure to Carcinogens | Elevates risk, especially with smoking |
| Previous Radiation Therapy | Can heighten risk of lung cancer |
The Types of Lung Cancer
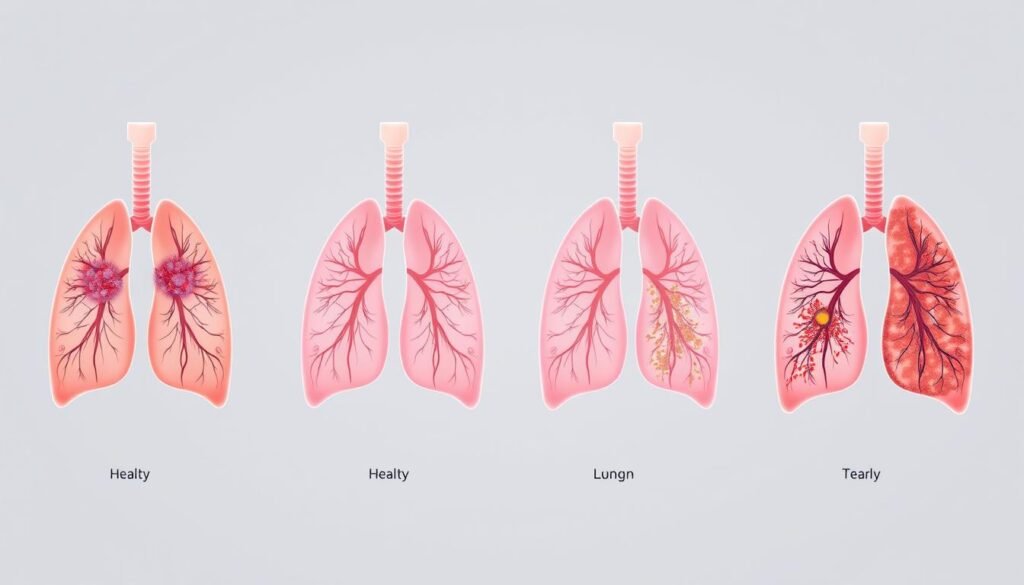
Lung cancer can be complex, with several types that differ importantly. There are two main kinds: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Most people with lung cancer have NSCLC, which is about 80% to 85% of cases. This type is further broken down into subtypes like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Adenocarcinoma is seen most often in the U.S. It starts in the mucus-making cells. Squamous cell carcinoma and large cell carcinoma each have unique traits and ways they grow. SCLC, though, is found in 10% to 15% of cases and is known for being very aggressive and spreading quickly.
There are also rare kinds of lung cancer. These include lung carcinoid tumors, mesothelioma, and tumors in the mediastinum. Lung carcinoid tumors are slow-growing and uncommon, making up less than 5% of lung tumors. Mesothelioma, which is about 5% of cases, comes from the lung’s lining and is often due to asbestos exposure.
The table below summarizes the primary types of lung cancer, their prevalence, and key characteristics:
| Type of Lung Cancer | Percentage of Cases | Key Characteristics |
|---|---|---|
| Non-Small Cell Lung Cancer (NSCLC) | 80% – 85% | Common subtypes include adenocarcinoma, squamous cell, and large cell carcinoma. Grows slower compared to SCLC. |
| Adenocarcinoma | Most common NSCLC subtype | Originates in mucus-producing cells; prevalent in non-smokers. |
| Squamous Cell Carcinoma | Second most common NSCLC subtype | Often linked to smoking; arises in the central part of the lungs. |
| Large Cell Carcinoma | Rare NSCLC subtype | Characterized by large, abnormal cells; aggressive growth. |
| Small Cell Lung Cancer (SCLC) | 10% – 15% | Highly aggressive; spreads rapidly; often diagnosed at an advanced stage. |
| Lung Carcinoid Tumors | Less than 5% | Slow-growing, neuroendocrine tumors. |
| Mesothelioma | About 5% | Linked to asbestos exposure; arises from the lung lining. |
https://www.youtube.com/watch?v=ihCnDjyJv5c
How Aggressive Is Lung Cancer
Lung cancer varies in aggressiveness based on type. We’ll explore Non-Small Cell Lung Cancer (NSCLC) and Small Cell Lung Cancer (SCLC). Understanding them highlights how lung cancer aggressiveness needs different treatments.
Characteristics of Non-Small Cell Lung Cancer (NSCLC)
Non-Small Cell Lung Cancer makes up 80% to 85% of cases. It grows slower than aggressive types, like SCLC. Adenocarcinoma is the most common NSCLC, usually found in the lungs’ outer parts.
It’s known for being less aggressive. On the other hand, large cell carcinoma is rarer. It grows quickly and spreads fast. The different NSCLC types need specific treatment strategies.
Characteristics of Small Cell Lung Cancer (SCLC)
Small Cell Lung Cancer is about 15% of cases and very aggressive. It starts in the central chest. Then, it rapidly grows, spreading to the brain, liver, and bones. SCLC is mainly caused by smoking.
It’s very rare in non-smokers. Surviving SCLC is hard, with few living over five years. Treatments like chemotherapy and radiation can help, but often don’t cure. Catching it early may improve life expectancy slightly.
Lung Cancer Stages and Their Significance
It’s crucial to know the lung cancer stages to find the right treatment. The system for staging looks at tumor size, if lymph nodes are involved, and if it has spread. This helps doctors figure out the best treatment for each stage.
Overview of Lung Cancer Staging
Lung cancer is split into two kinds: Non-small Cell Lung Cancer (NSCLC) and Small Cell Lung Cancer (SCLC). Each type has stages from 0 to IV for NSCLC. Here’s a quick look:
- Stage 0: Cancer is only in the lung’s lining or the bronchus.
- Stage I: Cancer is split into 1A and 1B, based on size and lymph nodes.
- Stage II: Divided into IIA and IIB, due to tumor size and lymph nodes.
- Stage III: This stage includes IIIA, IIIB, and IIIC, meaning it’s spread often to lymph nodes.
- Stage IV: Shows cancer has spread far, even to different organs or the lung’s lining.
SCLC is simpler, labeled as limited or extensive, depending on its spread. Knowing this helps in choosing the right treatment path.
Impact of Stage on Treatment Options
Knowing the lung cancer stage is key to picking treatment methods. Options may include:
- Surgery for early stages (I and II).
- Chemotherapy and radiation are common for later stages (III and IV).
- Targeted therapies and immunotherapies are chosen based on cancer traits.
Determining the cancer stage lets oncologists craft treatments that work well while keeping life quality in mind. Finding cancer early often means better treatment results, showing why knowing about this is vital.
| Stage | Description | Treatment Options |
|---|---|---|
| Stage 0 | Confined to the lining of the lung. | Surgery |
| Stage I | Localized with no lymph node involvement. | Surgery, Radiation |
| Stage II | Extended to nearby lymph nodes. | Surgery, Chemotherapy |
| Stage III | Cancer involved in mediastinal lymph nodes. | Chemotherapy, Radiation, Surgery |
| Stage IV | Metastatic cancer affecting distant organs. | Palliative care, Chemotherapy, Targeted therapies |
Lung Cancer Spread Rate: How Fast It Can Grow
Lung cancer grows and spreads at different speeds. This depends on the cancer type and the patient. Small Cell Lung Cancer (SCLC) spreads quickly because its cells divide fast. This kind of cancer can spread to other parts of the body in just a few weeks or months after finding out about it.
About 10% to 15% of lung cancers are SCLC. Shockingly, almost half of these are already spread at diagnosis time. For SCLC, two-thirds are found spread beyond the lungs when detected. This shows why knowing how fast lung cancer spreads is crucial.
Non-Small Cell Lung Cancer (NSCLC) grows slower but is still dangerous. For example, adenocarcinoma, a kind of NSCLC, grows slowly. However, finding it late is still risky. Without treatment, NSCLC patients might live just over seven months. SCLC patients have a shorter survival time, between two to four months.
The growth speed of cancer affects treatment choices. NSCLC tumors found on CT scans usually double in size every 134 days. This means lung cancers can get twice as big every four to five months. Tumors in smokers grow faster than in non-smokers.
| Cancer Type | 5-Year Survival Rate | Average Doubling Time |
|---|---|---|
| Localized NSCLC | 65% | 134 days |
| Nearby Tissue NSCLC | 37% | 134 days |
| Distant Spread NSCLC | 9% | 134 days |
| Localized SCLC | 30% | 97.6 days |
| Nearby Tissue SCLC | 18% | 97.6 days |
| Distant Spread SCLC | 3% | 24 days |
Understanding how fast lung cancer spreads is key to improving chances of survival. Catching it early can make a big difference, especially with NSCLC. Knowing the specific growth rate of the cancer can help in making a personalized treatment plan.
Lung Cancer Metastasis: Understanding the Process
Lung cancer metastasis is a major issue in treating the disease. Cancer cells leave the lung tumor and move to other body parts via blood or lymph. They often spread to the brain, bones, liver, and other lungs. Knowing how lung cancer spreads helps in treating it effectively.
About 53% of lung cancer cases are found after they have spread. This means they are detected late, making treatment harder. The chance of surviving five years after such a diagnosis is only 8.9%. It’s vital to spot symptoms early. Yet, symptoms like coughing, breathlessness, and chest pain often appear late.

Metastasis greatly influences treatment choices. A study found different survival rates for lung metastases from colorectal and breast cancers. For instance, breast cancer’s five-year survival rate drops from 96% to 21% with lung metastasis. Accurate tests like imaging and biopsies are crucial for early detection.
| Type of Cancer | Metastasis to Lungs | 5-Year Survival Rate (with Metastasis) | 5-Year Survival Rate (without Metastasis) |
|---|---|---|---|
| Breast Cancer | Common | 21% | 96% |
| Colorectal Cancer | Common | Less than 10% | 91% |
| Other Cancers | Varies | Varies | Varies |
Treatments for spreading lung cancer include chemo, targeted therapy, and immune therapy. Each therapy has side effects that may affect life quality. With new drugs and tests being developed, hope rises for those with lung cancer and metastasis.
Lung Cancer Prognosis and Survival Rates
Lung cancer’s outlook can change based on the cancer type, stage, and patient health. Knowing these factors helps predict survival rates. This information is vital for patients and their families.
Comparative Survival Rates for NSCLC and SCLC
Non-small cell lung cancer (NSCLC) often has higher survival rates than small cell lung cancer (SCLC). This is clear when looking at survival data by stage. Here’s a detailed comparison:
| Cancer Type | Stage | 5-Year Survival Rate |
|---|---|---|
| NSCLC | Localized | 65% |
| NSCLC | Regional | 37% |
| NSCLC | Distant | 9% |
| NSCLC | All SEER stages combined | 28% |
| SCLC | Localized | 30% |
| SCLC | Regional | 18% |
| SCLC | Distant | 3% |
| SCLC | All SEER stages combined | 7% |
The stats show a big difference in survival rates between NSCLC and SCLC. NSCLC patients, especially with early-stage cancer, have better chances. This emphasizes the importance of catching cancer early and the impact of new treatments.
Treatment Options for Lung Cancer
Choosing the right lung cancer treatment depends on its type and stage. Non-Small Cell Lung Cancer (NSCLC) and Small Cell Lung Cancer (SCLC) require different approaches. The disease’s progression and the patient’s health are key in this choice.
Standard Treatments Available for NSCLC
Treatment options for NSCLC change with the cancer’s stage:
- Stage 1 or 2: Surgery is usually the first step, sometimes along with targeted radiation therapy called stereotactic body radiation therapy (SBRT).
- Stage 3: Surgery and chemotherapy, or radiation and chemotherapy are options.
- Stage 4: The focus shifts to palliative care. This combines chemotherapy, immunotherapy, and specific drugs to ease symptoms and improve life quality.
New treatments for NSCLC include targeted therapies. These focus on the cancer’s specific genetic features, offering more options. To learn more, visit NSCLC treatment options.
Innovative Approaches in SCLC Treatment
SCLC’s fast spread means treatment must start quickly. Standard strategies include:
- Limited Disease: Usually, this involves chemotherapy with radiation therapy. If caught early, surgery might be an option.
- Extensive Disease: The focus is on palliative chemotherapy and immunotherapy. This helps relieve symptoms and improve comfort.
After treatment, recovery includes thorough assessments and support therapies. These help improve lung function and speed up recovery. Ongoing research into immunotherapy offers new hope for better results in treating both SCLC and NSCLC.

Living with Lung Cancer: Patient Perspectives
Living with lung cancer is tough for patients and their families. They often face fear and feel alone. It’s vital to stay connected with lung cancer support networks like family, friends, and groups. This support helps them deal with their diagnosis. Sharing experiences with others provides helpful tips on battling the disease.
Oswald Peterson, battling stage 4 non-small cell lung cancer, shows how new treatments can help. After starting immunotherapy with Keytruda, his cancer shrank quickly. His story highlights the need to fight for the best care and explore new treatments.
New treatments help many feel stronger and get back to their daily lives. Oswald says fighting lung cancer takes resilience and a willingness to try new therapies. His experience encourages others to seek good lung cancer support and community help.
The emotional toll on patients can lower their life quality. Sharing their stories helps us all understand lung cancer better. It lets healthcare workers offer better support tailored to each person’s needs. As treatments improve, so does the outlook for lung cancer management.
Social media is a key place for sharing stories about lung cancer treatment. It lets patients and caregivers talk about their experiences. This sharing fosters community and deepens discussions on treatment and health.
It’s important to know how lung cancer affects people and their families. Learning from patients’ experiences helps improve care and support for those facing this tough illness.
Conclusion
Knowing about lung cancer is key to dealing with it and helping patients live longer. Lung cancer is very aggressive, and sadly, only 20% of those diagnosed live more than five years. This fact shows why finding it early and treating it effectively is so important. Today, new treatments like immunotherapy and targeted drugs, such as osimertinib, are making a big difference.
To fight lung cancer, raising awareness is crucial. Quitting smoking, which is linked to 80% of lung cancer deaths, is a big step. We also need to tell people about the other risks, like radon and asbestos exposure. And we need to talk about how harmful it is to live with smokers.
Finally, we must keep researching and educating on lung cancer. By working together, patients and doctors can use what we know to catch cancer early. This teamwork leads to better chances of beating lung cancer. It requires everyone to pay attention and take action.