Did you know almost half the lung cancer patients see their life quality drop in the first three months after a pneumonectomy? This fact sheds light on the huge challenges they face emotionally, physically, and mentally. It’s not just about overcoming a major surgery. It’s also about dealing with loss and adapting to new limits that can last for months or years. Knowing about the long-term effects and how to recover helps build a base for better healing. This article will share important tips on moving from surgery towards recovery. It aims to help people get back on track to health and wellness.
Key Takeaways
- Pneumonectomy requires a deep understanding of how it affects you and ways to recover.
- Post-surgery pain and discomfort are common and can last for several months.
- Walking every 2 hours after surgery is key to lower the chance of complications.
- It’s vital to keep an eye on and manage pain for a smoother recovery.
- A team approach, including getting help from respiratory therapists, supports long-term healing.
- Life quality might drop significantly in the time post-pneumonectomy.
- Making changes to your lifestyle can majorly improve your lung health after the surgery.
Understanding Pneumonectomy and Its Necessity
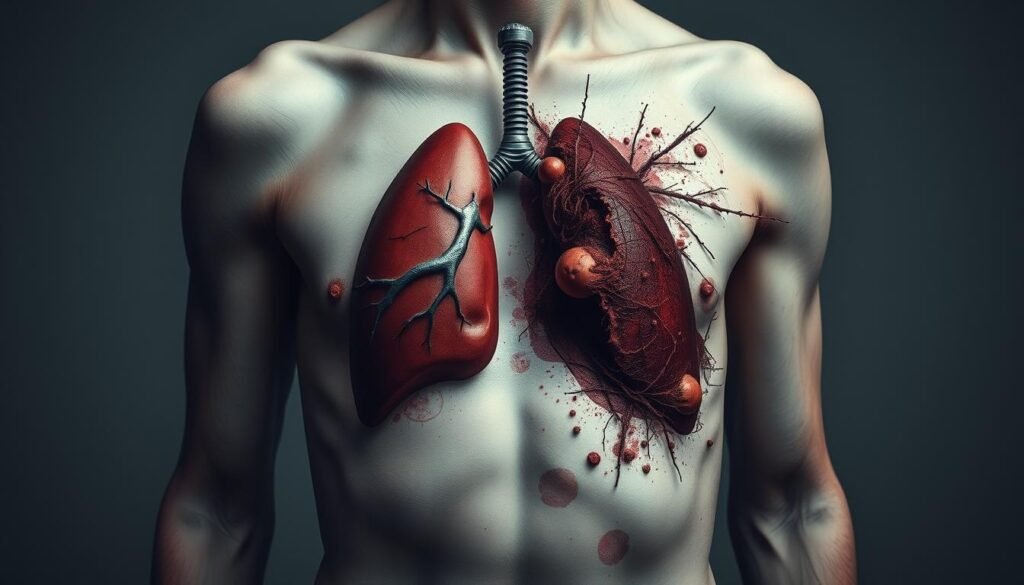
Pneumonectomy is the surgical removal of an entire lung. It’s often needed for those with lung cancer or severe lung diseases. The main goal of this surgery is to cure lung cancer. It offers the highest chance of success. When other treatments won’t work and the cancer is near vital chest structures, pneumonectomy might be the best option.
There are different types of surgery for lung diseases. Pneumonectomy removes the whole lung. But lobectomy, segmentectomy, and wedge resection could be better for early-stage diseases. These methods try to save as much lung function as possible. Sometimes, sleeve resection is used. It keeps lung capacity while removing tumors in large airways.
Recovering from lung removal takes time. It can last weeks to months, depending on the surgery and the patient’s health. Hospital stays after surgery vary. They can be from one to seven days, depending on the operation and any complications that occur.
Removing a lung is often needed to stop lung disease from getting worse or to ease symptoms of advanced conditions. The recovery can be tough. Understanding what pneumonectomy involves is crucial. It helps patients and their families get ready for what lies ahead.
| Surgical Type | Description | Typical Use |
|---|---|---|
| Pneumonectomy | Removal of an entire lung | Advanced lung cancer, severe disease |
| Lobectomy | Removal of an entire lobe of a lung | Non-small cell lung cancer |
| Segmentectomy | Removal of a segment of a lobe | In cases where less extensive removal is necessary |
| Wedge Resection | Removal of a small, wedge-shaped portion of a lobe | Targeting localized tumors |
| Sleeve Resection | Removal of a section and reconnection of the remaining lung | Preserving lung function for cancers near large airways |
The Immediate Effects of Pneumonectomy
After a pneumonectomy, patients face several challenges. Removing one lung has a big impact on the body. Knowing what symptoms to expect is key to taking care of them afterwards.
Post-Surgery Symptoms and Monitoring
About 85% of people feel tired and weak after the surgery. They may also have trouble breathing and feel pain. How fit they were before the surgery and how it was done affects this. Watching their vital signs and breathing closely is important.
In rare cases, they might have serious problems like air leaks or a collapsed lung. This needs quick treatment. There’s also a risk of getting infections in wounds, the chest, or the urinary tract. Some might need more surgery to deal with these infections.
Initial Recovery in the Hospital
Recovery at the hospital usually takes several days. Patients may get help with breathing, pain relief, and chest tube care. Using tools like incentive spirometry helps with deep breaths and healing.
Moving around early is crucial to prevent blood clots, such as DVT. DVT’s signs include leg swelling and redness. This happens from not moving much.

Some people may have long-term pain from nerve damage in surgery. This pain often lessens as they heal. Learning about recovery helps patients deal with these issues. The National Institute for Health and Care Excellence offers detailed care guidelines for lung cancer patients.
Coping with the Loss of a Lung
Losing a lung brings about deep emotional changes. People feel grief, anxiety, and depression. It’s a huge change in life. Getting emotional support for lung patients is crucial. This can be through mental health help or support groups. They help deal with these tough feelings after lung surgery.
Emotional and Psychological Adjustments
The grief journey is different for everyone. It often lasts months or even years. Accepting your feelings is key, not hiding them. Joining bereavement support groups offers comfort. They help by sharing experiences. Using resources like coping strategies gives power to face hardship.
Adapting to Physical Limitations
Adapting to new physical limits is key after lung removal. Daily life, exercise, and lifestyle may change. Focus on what you can control. This includes light exercise and a balanced diet. Acknowledging these changes is part of adapting. Support from others can build strength during this time.

Long-Term Effects of Lung Removal
Going through lung removal surgery, or pneumonectomy, leads to many long-term effects. One key change is how you breathe. After the surgery, many see a change in how much air their lungs can hold. This causes different levels of long-lasting breathlessness. While some people adjust well, others struggle with these changes in breathing.
Changes in Breathing Functionality
The effect on how you breathe can be different for everyone. Studies show many face side effects like less effective breathing. This makes physical activities harder and changes daily life for many. People need to adapt to these new breathing patterns. It’s good to take part in therapies that improve breathing over time.
Potential for Chronic Pain and Discomfort
Long-term pain after lung surgery is common. It often comes from nerve damage during surgery. Many report a condition called postpneumonectomy syndrome, which causes chest pain and discomfort. Knowing about the risk of chronic pain helps people find good pain control methods early. Addressing these symptoms is crucial for a smooth recovery after lung removal.
Managing Breathlessness and Respiratory Health
People who have lost a lung often feel short of breath. It’s important to know effective ways to handle this. Learning how to manage this can really help improve their lives. By using certain breathing methods, people can control their symptoms better. This also helps lessen their anxiety.
Breath Management Techniques
There are good techniques to manage breathlessness. They include:
- Pursed-lips breathing: This helps slow your breathing and keeps airways open.
- Diaphragmatic breathing: Using your diaphragm for breathing brings deeper breaths. It can make you feel better.
- Paced breathing: Useful during exercise, it keeps your breathing steady and stops you from holding your breath.
- Relaxed tummy breathing: Breathing with your belly relaxed helps reduce stress and increases oxygen intake.
- Sitting leaning forward can also help you recover from feeling out of breath.
Starting these techniques slowly is key. They help people handle breathlessness better, giving them more control over their daily lives.
Importance of Respiratory Therapy
Respiratory therapy is very helpful for those managing lung health. Its benefits are:
- It makes the remaining lung stronger with special exercises.
- Therapy plans are made to fit each person’s needs, which helps them recover in their own way.
- It also reduces stress and teaches how to relax. This is good for both mental and physical health.
This therapy doesn’t just offer quick fixes; it leads to lasting improvements in lung health. Meeting regularly with a trained therapist helps people learn effective breath control techniques. They become empowered to handle their new lifestyle and keep their lungs healthy.
Benefits of Pulmonary Rehabilitation
Pulmonary rehab is key for those recovering from lung surgery or chronic breathing problems. It offers more than just workouts. It provides customized programs to boost health and life quality. By joining, patients can get stronger, breathe better, and learn how to manage their illness.
What to Expect in a Rehabilitation Program
Starting rehab means entering a recovery-focused setting. Here, you’ll find:
- Personalized exercise plans to build strength.
- Tips on handling COPD and making lifestyle changes.
- Steps to live healthier.
- Advice on eating well for better health.
- Support for your emotional needs.
Through rehab, getting better and handling symptoms get easier, motivating participants. This approach not only eases symptoms like breathlessness but also empowers people to actively manage their health for the future.
How to Stay Motivated
Keeping up with rehab post-surgery may seem hard. Setting SMART goals helps keep the focus. This method shows clear progress, boosting morale. Celebrating small wins along the way is important too.
Being part of a community with the same struggles can be uplifting. Knowing the pulmonary rehabilitation benefits can improve not just physical health, but emotional strength as well. This makes life after surgery much better. For tips on COPD management, visit this resource.
Integrating Lifestyle Changes Post-Surgery
Making lifestyle changes after pneumonectomy is key for a better recovery and life. Eating right and exercising can make a big difference for your lungs and health. It’s important to eat a balanced diet filled with important nutrients and to follow safe exercise rules after surgery.
Nutrition and Diet for Lung Health
Eating well is important for lung patients to boost the immune system and heal. Foods high in vitamins, minerals, and antioxidants fight stress and help breathing. Here are some good food choices:
- Fruits and vegetables: Rich in vitamins A, C, and E
- Whole grains: Provide fiber and essential nutrients
- Lean proteins: Support muscle health and recovery
- Omega-3 fatty acids: Found in fish and walnuts to reduce inflammation
Following custom nutritional advice can make a big difference post-pneumonectomy. Personal meal plans ensure enough protein and prevent muscle loss, crucial for recovery.
Exercise Recommendations and Limitations
After surgery, it’s important to follow exercise rules to build endurance and strength safely. Start with gentle activities like:
- Walking: A great way to gradually improve cardiovascular fitness
- Stretching: Enhances flexibility and reduces stiffness
- Pulmonary rehabilitation exercises: Focus on breathing techniques and stamina building
Checking with doctors and monitoring exercise levels will keep you safe. As you heal, you can slowly do more, depending on your lung health. Making these changes is key for a strong recovery from pneumonectomy.
| Food Category | Benefits |
|---|---|
| Fruits and Vegetables | Rich in vitamins and antioxidants, support immune function |
| Whole Grains | High in fiber, aids digestion and provides sustained energy |
| Lean Proteins | Essential for muscle repair and recovery |
| Omega-3 Fatty Acids | Help reduce inflammation, beneficial for lung function |
Maximizing Emotional Support for Lung Patients
Emotional support is crucial for lung patients on their recovery path. A strong support network greatly improves emotional health. This includes family, friends, healthcare professionals, and online support groups. Such connections make patients feel supported and less alone, easing anxiety and isolation feelings.
Building a Support Network
Lung patients should build a support system. Family and friends offer emotional support and practical assistance. They can also join local support groups or palliative care services for more emotional help. Joining these groups allows them to share struggles, which eases anxiety and leads to a better recovery. This interaction is key to a rewarding recovery journey.
Grief Counseling for Lung Disease
The impact of lung disease isn’t just physical; it’s emotional too. Grief counseling is helpful for dealing with these emotional effects. It helps patients process feelings of loss related to their health and lifestyle changes. With professional help, patients can better manage anxiety and stress. This, along with strong emotional support, helps patients and caregivers face their emotional hurdles, promoting a well-rounded recovery process.