In the United States, about 10% to 20% of lung cancer cases occur in non-smokers. That’s around 20,000 to 40,000 people who’ve never smoked or smoked less than 100 cigarettes. This fact shows that lung cancer isn’t only a smoker’s disease.
Lung cancer in non-smokers is a major public health issue. It gets less attention than the risks of smoking. We need to understand the risk factors and how environment and genetics play a role. Knowing these can help us prevent it and push for better health policies.
Key Takeaways
- Approximately 10% to 20% of lung cancer cases occur in non-smokers.
- Secondhand smoke and radon exposure are significant contributors to lung cancer risks.
- Adenocarcinomas make up 50% to 60% of lung cancers in non-smokers.
- Environmental and genetic factors play crucial roles in lung cancer development.
- Preventive measures can significantly reduce lung cancer risks in non-smokers.
- A targeted therapy may be effective for non-smokers with specific genetic mutations.
- Lung cancer in non-smokers often develops at a younger age compared to smokers.
Introduction to Lung Cancer in Non-Smokers
Lung cancer is not just a concern for smokers. It also affects non-smokers. The introduction to lung cancer in non-smokers shows how different factors increase their risk. While smoking is a known cause, non-smokers can get lung cancer too. They’re exposed to environmental hazards.
Risk factors for non-smokers include secondhand smoke, radon, and pollution. Learning about these can help. Lung cancer awareness means knowing the dangers. This knowledge empowers people to protect themselves.
Statistics are worrying. Predictions for 2023 say over 20,000 non-smokers in the USA will die from lung cancer. This makes it one of the top cancer killers for non-smokers. Most of these cases, around two-thirds, happen in women. It’s important for non-smokers to know their risk.
Understanding these risks is the first step. Next, we explore lung cancer factors, numbers, and how to prevent it. It’s about raising awareness and promoting healthy choices.
Understanding Lung Cancer Statistics
Statistics about lung cancer show a surprising fact: 10% to 20% of people who get lung cancer never smoked. This highlights how crucial it is to be aware of lung cancer risks among non-smokers. Lung cancer among those who have never smoked tends to show up more in women and at a younger age compared to smokers.
Lung Cancer Incidence Among Non-Smokers
About 12% of lung cancer patients in the U.S. have never smoked. From the early ’90s to now, the percentage of never-smokers with lung cancer increased from 8% to about 15%. This points to a growing problem. Studies find that 20% of women and 9% of men with lung cancer never smoked, underlining the need for more research and awareness.
Percentage of Lung Cancers Attributed to Non-Smoking Factors
Secondhand smoke and radon are big reasons non-smokers may get lung cancer. Around 7,000 lung cancer cases in non-smokers might come from secondhand smoke. Another 3,000 cases could be from radon. Despite these numbers, lung cancer in non-smokers remains prevalent, showing other factors also play a role.
The data tells us a lot of lung cancer cases happen in non-smokers. This makes it clear we need to keep researching what causes lung cancer in non-smokers and how it’s different.
| Statistic | Percentage |
|---|---|
| Never-smokers among lung cancer patients (1990-1995) | 8% |
| Never-smokers among lung cancer patients (2011-2013) | 14.9% |
| Lung cancer cases in U.S. women who never smoked | 20% |
| Lung cancer cases in U.S. men who never smoked | 9% |
| Estimated lung cancer cases from secondhand smoke in never-smokers | 7,000 |
| Estimated lung cancer cases from radon exposure in never-smokers | 3,000 |
Can a Non Smoker Get Lung Cancer: Risk Factors Explored
It’s vital to understand how non-smokers can get lung cancer. Many factors, like secondhand smoke and radon, up the risk. Knowing about these can help us fight lung cancer in those who’ve never smoked.
Secondhand Smoke Exposure
Secondhand smoke is a big risk for non-smokers. With over 70 cancer-causing agents, it’s harmful. Non-smokers around it can have a 25% higher risk of lung cancer. This often happens in places where people smoke, like some homes or workplaces.
Radon Exposure and Its Risks
Radon is also a major risk factor. This gas is invisible and has no smell. But it can get into homes through small cracks. Being around a lot of radon for a long time can make lung cancer more likely.
So, it’s key to check your home for radon every two years. This is extra important in areas where radon is common. By doing this, non-smokers can lower their lung cancer risk and live in safer environments.
Environmental Factors Contributing to Lung Cancer
It’s vital to know how our environment can raise lung cancer risk, especially for those who don’t smoke. Air pollution is a huge risk factor that affects many across the U.S. Tiny particles like dust and chemicals in the air cause 1%-2% of lung cancer cases. These pollutants can hurt our lungs and even change our DNA, making us vulnerable to cancer.
Impact of Air Pollution on Lung Health
Air pollution is a big threat to our lungs and increases lung cancer risk. It has a buildup effect over years, especially in polluted places. People living in such areas are at a higher risk. We need to work on cleaner air to protect our lungs and lessen cancer risks.
Occupational Hazards and Lung Cancer Link
Workplace dangers play a big role in lung cancer risk. Being around asbestos, diesel smoke, and harsh chemicals puts workers in danger. These substances can greatly increase lung cancer risk. Therefore, having a safe workplace is crucial. Non-smokers should also be aware of these risks at work to protect their health.

Want more details on environmental risks and lung cancer? Check out this in-depth guide here.
The Role of Genetic Factors in Lung Cancer
Understanding the role of genes in lung cancer is not simple. It’s about inherited and somatic mutations. Even people who don’t smoke can get lung cancer due to their genes. Your genetics can influence how you react to things like pollution or smoke. For example, some people’s genes make them more likely to get lung cancer.
Inherited Genetic Mutations
Research shows that certain gene mutations increase the risk of lung cancer. Genetic testing helps find those at risk. Changes in the 15q24 area can make smokers more likely to get lung cancer by 30% to 80%. These findings tell us that not all lung cancer patients have smoked. Each year, lung cancer affects about 222,500 people in the U.S. It’s a big portion of all cancer cases.
Somatic Mutations in Non-Smokers
Somatic mutations happen due to DNA changes after birth and are key in non-smokers. These include changes in the TP53, EGFR, and KRAS genes. Such mutations are common in lung cancer patients. They show a clear link between these genetic changes and lung cancer. For instance, EGFR gene changes offer new ways to treat the disease. This knowledge helps doctors treat lung cancer more effectively, focusing on each patient’s unique situation.
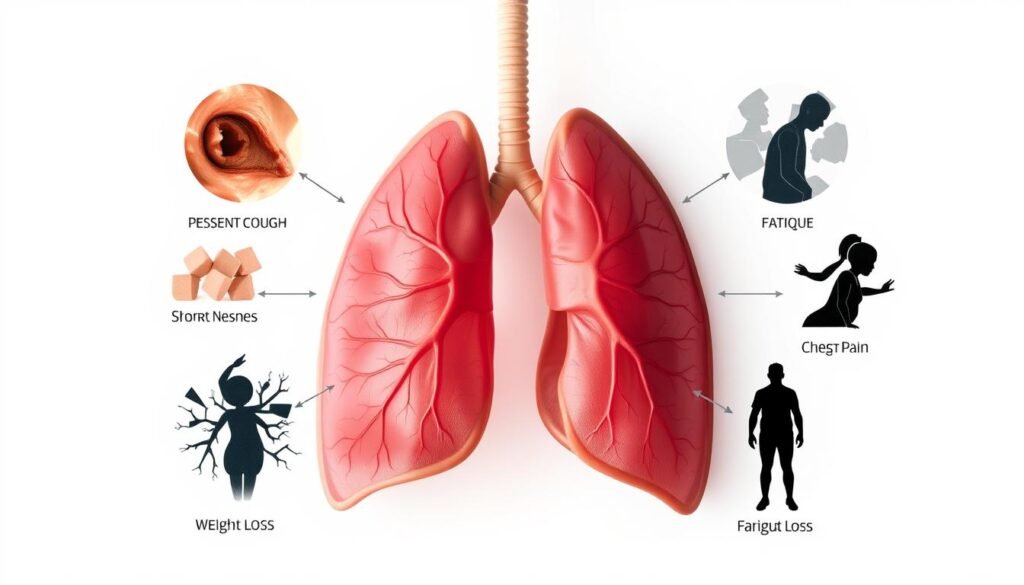
Common Symptoms of Lung Cancer
It can be hard to spot lung cancer symptoms, especially for non-smokers. They might think these symptoms are from other illnesses or not notice them. Knowing about both general and specific symptoms is key for catching the disease early.
Recognizing General Symptoms
Common symptoms of lung cancer include:
- Fatigue
- Persistent cough
- Chest pain
These symptoms might not seem serious at first. This could lead to delays in getting help. It’s vital to pay attention to your health and see a doctor if anything changes.
Specific Symptoms Related to Lung Cancer
Certain symptoms are strongly linked to lung cancer:
- Coughing up blood
- Shortness of breath
- Wheezing
Don’t ignore these signs, they could mean lung cancer is present. Non-smokers should also talk to their doctors about any unusual health changes. Finding lung cancer early can make treatment more effective.
Preventive Measures for Non-Smokers
Taking steps early on can greatly lower your chances of getting lung cancer if you don’t smoke. Knowing how to prevent lung cancer can improve lung health. It also lessens the risks from bad environmental elements.
Avoiding Secondhand Smoke
Creating smoke-free spaces at home and work is key to avoid secondhand smoke. Non-smokers can face a 25% higher risk of lung cancer from secondhand smoke. Especially if exposed as children. Actions like supporting no-smoking areas help make healthier places and cut down on cancer dangers.
Testing for Radon in Homes
Checking your home for radon regularly is important. It’s especially true where radon is often high, like the Mountain West. Tests every two years can alert you to dangerous radon levels. If levels are above 4.0 pCi/L, it’s time to get a radon reduction system. This action is vital for keeping your home safe.
| Preventive Measure | Description | Frequency |
|---|---|---|
| Avoid Secondhand Smoke | Establish tobacco-free spaces to reduce exposure. | Incurable |
| Radon Testing | Test for radon levels in homes to manage risks. | Every 2 years |
| Air Quality Monitoring | Stay informed about local air pollution levels. | Regularly |
Using these strategies helps keep your lungs healthy and your living area safe. By focusing on these preventive actions, you can take charge of your health. This way, you lower your chances of getting lung cancer.
Understanding Lung Cancer Treatments for Non-Smokers
Lung cancer treatments for people who’ve never smoked are improving a lot. There’s more knowledge about the types of lung cancer affecting them. This has led to better, targeted treatments. These treatments focus on specific genetic changes found in testing. They offer more personalized care compared to standard treatments.
Targeted Therapy and Genetic Testing
Targeted therapy is a big step forward in treating lung cancer in non-smokers. It’s vital to find certain genetic changes that occur. These changes are often unique compared to those in smokers. Up to 92% of lung cancers in non-smokers can be treated with FDA-approved precision drugs. Genetic testing helps pick the best treatment and understand the tumor’s biology.
Different Types of Lung Cancer Found in Non-Smokers
Adenocarcinomas are most common among non-smokers, making up to 60% of cases. This cancer acts differently than the types seen in smokers. Knowing these differences helps in planning treatment. The presence of mucinous and non-mucinous subtypes adds complexity to treating non-smokers.

It’s becoming crucial to consider genetic risks. These risks can significantly increase non-smokers’ chances of getting lung cancer. Using targeted therapies and specific diagnostic tests, doctors can create effective lung cancer treatments for non-smokers. This improves survival rates and the quality of care.
| Type of Lung Cancer | Prevalence in Non-Smokers | Common Mutation |
|---|---|---|
| Adenocarcinoma | 50%-60% | EGFR mutations |
| Squamous Cell Carcinoma | Less common | TP53 mutations |
| Large Cell Carcinoma | Rare | ALK rearrangements |
With growing awareness, non-smokers should talk to doctors about lung cancer treatments right for them. Environmental factors and genetics are important to consider.
Family History and Lung Cancer Risk
Knowing how family history affects lung cancer risk is vital for health concerns. If you have family members with lung cancer, your chance of getting it can be higher. This is because of genetics, which may increase your risk.
Studies show that if a close family member had lung cancer, your risk goes up. Specifically, there’s a 1.51 times higher chance, even if you don’t smoke. That’s why talking to doctors about your family’s health history is key.
Some genes are linked to more lung cancer cases, especially among non-smokers. Researchers look at genes like EGFR to learn more about this connection. Understanding these gene changes helps us know more about lung cancer risks.
Getting genetic tests if you have a family history can be smart. These tests help you understand your risk better. Then, you and your doctor can work out how to watch for or prevent cancer. For more on how family history and lung cancer are connected, check out this research on lung cancer.
Conclusion
Lung cancer is a big health problem, not just for smokers but also for those who’ve never smoked. About 10–15% of lung cancers are found in never smokers. This results in thousands of deaths in the U.S. every year not linked to smoking. It shows how important it is to work harder on prevention and raising awareness.
Nearly half of lung cancers in never smokers are due to factors other than smoking. It’s vital that health experts and the public pay attention to early detection and acting quickly. Knowing the risks related to the environment and genes can really help these patients. Screenings and pushing for healthier lung habits can tackle this issue. People need to know their risks and take steps like radon tests and avoiding polluted air.
The rise in lung cancer among non-smokers is something we can’t ignore any longer. It’s a call to action for more research and attention. As we come together to help this group, finding what causes their lung cancer is key. For more information, including new studies, check out important research aimed at increasing awareness and finding better treatments.