Asthma impacts 300 million people all over the world. It can cause severe problems if not managed right, including emergency hospital visits. This condition makes the airways of the lungs inflamed and very sensitive, affecting how well the lungs work. With more people getting asthma, it’s important to look at how asthma and chronic inflammation affect lung health. This piece explores how these issues are connected. It looks at what it means for breathing health and what can be done to help.
Key Takeaways
- Asthma affects an estimated 300 million individuals globally.
- Uncontrolled asthma can lead to serious complications, including hospitalizations.
- It increases susceptibility to respiratory disorders like pneumonia.
- Airway remodeling can occur with unmanaged asthma over time.
- There is a notable link between obesity and asthma risk.
- Environmental factors, including urbanization, contribute to asthma prevalence.
Understanding Asthma: A Complex Condition
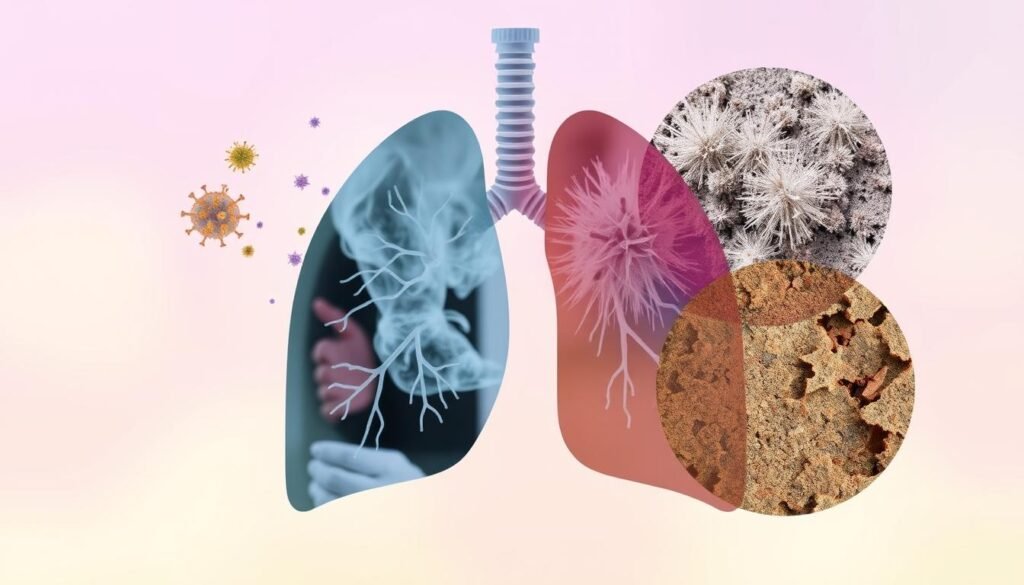
Asthma is not just a single disease, but a complex condition. It involves ongoing airway inflammation and increased sensitivity in the airways. Because it can lead to serious, even life-threatening attacks, managing asthma every day is essential. Both genetic and environmental factors play a big role in forming asthma. They cause different symptoms and how well treatments work.
About 50-70% of asthma cases are allergic asthma, linked to specific allergens. Knowing these asthma triggers is key to handling the condition. For example, things like dust, pet fur, mold, smoke, and pollen can set off asthma.
Keeping airway inflammation under control is very important. If not, flare-ups can make symptoms much worse. This leads to more swelling, mucus, and tight airways, making it hard to breathe. These episodes can increase discomfort and even lead to more attacks if ignored. And, without proper treatment, asthma can change the airways over time, causing scarring. This makes asthma medicine less effective.
Asthma can start at any age, affecting both children and adults in different ways. Being born prematurely raises the risk of having asthma. Plus, things like working around certain substances, smoking, and being overweight can make asthma worse. Treatments usually include inhaled steroids to lessen inflammation, which helps improve life quality.
Asthma’s complexity means everyone needs a plan tailored to their situation. Such plans help people not just deal with symptoms but also lead normal, healthy lives. For more on how inflammation affects the lungs, check out this informative resource.
Chronic Inflammation and Its Role in Respiratory Disorders
Chronic inflammation is key in respiratory disorders such as asthma and COPD. It happens when the immune system wrongly acts against harmless environmental things. This leads to ongoing inflammation. Cells like macrophages and T lymphocytes play a role in this by producing cytokines. These cytokines help immune cells survive and find where to go.
When it comes to COPD, smoking is a major cause. Almost 90% of COPD cases are due to smoking. Yet, some cases come from genetic issues like alpha-1-antitrypsin deficiency. This constant inflammation can harm not just the lungs. It also risks heart disease and lung cancer.
People with chronic inflammation react differently. For COPD patients, more immune cells in airway secretions signal a stronger immune response. This makes symptoms worse and speeds up lung function loss. Healthcare workers need to understand inflammation to manage these disorders better. To learn more about how chronic inflammation and COPD interact, more research is necessary. Particular focus is needed on how inflammation links to other health issues associated with respiratory disorders.
How Asthma and Chronic Inflammation Affect Lung Health
Asthma and chronic inflammation play a big part in lung health. Asthma leads to chronic inflammation, which can hurt pulmonary function. This means that the airways can’t let air flow freely. This causes problems like wheezing and breathlessness.
Chronic inflammation may also change the lung’s structure, known as airway remodeling. This can permanently decrease how well the lungs work. People with asthma might be more sensitive to different things, making symptoms worse. This happens because of inflammation and certain immune cells.
Around 300 million people worldwide have asthma. The numbers are going up, which shows we need to understand this issue better. The cost of taking care of people with asthma is high. Since asthma can be triggered by many things, it’s important to have a plan that fits each person. This includes looking at their specific situation and the type of asthma they have.
The Mechanisms of Airway Inflammation
It’s vital to know how asthma impacts lung health through airway inflammation. Asthma involves many cells and molecules working together. Scientists have found over 100 substances like cytokines that play a part in this.
Cellular and Molecular Mediators of Inflammation
Eosinophils and mast cells are key in airway inflammation. Eosinophils’ presence leads to more inflammation. This often causes the airways to thicken and muscles to grow, making breathing harder.
Activated epithelial cells release factors that make muscle cells grow and extra proteins appear. This makes asthma worse.
The Role of Eosinophils and Mast Cells
Eosinophils help in both inflammation and repairing tissues. They keep the cycle of irritation going. Mast cells cause tightening of the airways through histamine, making the airways more sensitive.
These cells work together to worsen asthma inflammation. Seasonal changes and infections also play a role in this process.

| Mediator | Source Cells | Effects |
|---|---|---|
| Cytokines (e.g., IL-4, IL-5) | Eosinophils, mast cells, Th-2 cells | Promote inflammation and eosinophil recruitment |
| Histamine | Mast cells | Causes bronchoconstriction and increased vascular permeability |
| Growth Factors (e.g., EGF, PDGF) | Activated epithelial cells | Enhance smooth muscle proliferation and fibrosis |
| Pro-inflammatory Cytokines | Eosinophils | Sustain airway inflammation and remodeling |
| Toll-like receptors (TLRs) | Airway smooth muscle cells | Promote hyperresponsiveness and inflammation |
Impact of Environmental Factors on Asthma
Environmental factors are key in both causing and worsening asthma. They affect the breathing health of many people. In the U.S., about 25 million people have asthma. This includes over 4.7 million children. Asthma rates are greatly tied to air quality and allergens around us. Asthma triggers include air pollutants, allergens, and certain home settings.
Studies show that areas with a lot of air pollution see more severe asthma in adults. Also, children moving to less poor areas get better from their asthma symptoms. Being exposed to things like PM2.5 and nitrogen dioxide early on can lead to more asthma in the future.
Indoors, things like dust mites are big asthma triggers. They affect around 85% of kids with asthma who are allergic. In cities, mouse and cockroach allergens also make asthma worse for many. Knowing about these risks is important for those impacted.
Making eco-friendly choices, like using zero-emissions vehicles, can help ease asthma. Changing where we live and pushing for clean air can help fight asthma triggers. These efforts improve public health and our planet’s well-being.
| Environmental Factor | Impact on Asthma |
|---|---|
| Outdoor Air Pollution (PM2.5, NO2) | Increases asthma cases and exacerbates symptoms |
| Indoor Allergens (Dust Mites, Molds) | Common triggers for asthma, particularly in children |
| Traffic-Related Air Pollution | Linked to wheezing and development of asthma in infants |
| High Levels of Poverty | Associated with higher rates of asthma and respiratory issues |
| Zero-Emissions Vehicles | Reduction in emergency asthma visits and symptoms |
Taking steps to lessen these environmental factors is key for better breathing health and managing asthma. Being aware and taking action can greatly improve life for those with asthma.
Airway Hyperresponsiveness: A Key Feature of Asthma
Airway hyperresponsiveness (AHR) is a main sign of asthma. It means the airways narrow too much when exposed to things like dust. This leads to symptoms like coughing, wheezing, and breathing hard. Factors like inflammatory mediators, which increase during asthma attacks, play a role in AHR. They make timely bronchodilation important to ease the narrowing of airways.
Years ago, Cockcroft and others introduced non-specific AHR testing. This testing is still key in diagnosing asthma, figuring out how severe it is, and planning treatment. If a methacholine challenge test is positive, it’s helpful in diagnosing asthma. However, a negative result can’t rule out asthma if symptoms are still there. After a long-term treatment with a high dose of inhaled corticosteroids, 40% of people showed normal responses to the test.
A higher risk of developing asthma and more wheezing is linked to increased AHR. In people with severe airway diseases, AHR is often worse. AHR can vary, especially in those over 50 or with non-atopic disease. This can affect diagnosis and how well treatments work.
Doctors use bronchoprovocation tests (BPTs) to check for AHR in asthma patients. Direct BPTs involve agents like methacholine. A positive test is when there’s a 20% drop in the amount of air a person can exhale in one second (FEV1). AHR can have fixed and variable parts. It’s influenced by inflammation and changes in the airways. Regular steroid inhalation can lessen AHR but might not get rid of it completely.
Treating asthma with inhaled corticosteroids helps a lot. It can improve how the lungs work and make asthma attacks less frequent. There’s evidence that adjusting steroid doses can cut down AHR by about 40%. This shows how effective treatment can control AHR.

| Factor | AHR Impact | Notes |
|---|---|---|
| Environmental Stimuli | Heightens AHR response | Contributes to symptoms like wheezing and coughing |
| Inhaled Corticosteroid Treatment | Reduces AHR severity | Improves overall lung function and decreases exacerbation frequency |
| Age and Disease Type | Increases AHR variability | More pronounced in non-atopic diseases |
| Response to Methacholine | Key diagnostic measure | Normal response may occur after treatment |
| Direct BPTs | High sensitivity for asthma detection | Influenced by exercise and inflammation |
Chronic Obstructive Pulmonary Disease (COPD) and Asthma Connection
COPD and asthma link shows how complex breathing problems can be, especially with similar symptoms. It’s vital to explore this link for better care of dual illnesses. People with both suffer more, from using healthcare more to facing serious exacerbations.
Understanding Co-Morbidities
Managing asthma and COPD gets tougher with other diseases. ACOS mixes the two, making symptoms worse and attacks more frequent. To diagnose ACOS, doctors review history, do exams, and use imaging. Recognizing symptom patterns and lung tests craft care plans.
Effects on Lung Function and Quality of Life
COPD and asthma harm lung function a lot. People with both do less physically and struggle with breathing more. This hurts their life quality. They end up in the hospital or emergency room more, pushing healthcare limits. Ongoing studies seek treatments to improve care for both. Inhaled meds could help improve life for those facing both conditions. For additional details on this connection, visit this resource.
Identifying Asthma Triggers: Patient Perspectives
Understanding asthma triggers is key in managing the condition well. Many people in Western countries are diagnosed with asthma. They often find between four to twelve things can trigger their asthma. These include weather changes, strong smells, and feeling stressed out. To help identify these triggers, patients might use the Asthma Trigger Inventory. This is a questionnaire with 32 items that is known for being very reliable.
When patients know and avoid their triggers, their health gets better. Those who know more about their triggers often have worse asthma. They also enjoy a lower quality of life. Interestingly, studies show women report more triggers than men. Also, those with more education tend to report fewer triggers.
Emotions play a big role in asthma control. Patients hit by emotional triggers tend to have more issues at night. Their overall quality of life goes down too. Different cultures see asthma triggers in unique ways. For instance, some South Asian cultures blame cold foods. Meanwhile, in Guatemala and Mexico, an imbalance of hot and cold is often the culprit.
It’s crucial to get how different perspectives link to asthma. For example, type 2 inflammation is tied to various triggers and how people react. Recent research shows that patients with hard-to-control asthma are at risk of severe attacks. Talking about personalized treatments with doctors can greatly help. It’s important to understand how triggers and personal reactions join up. This understanding leads to better health.
For more information about asthma, check out this insightful article.
Effective Anti-Inflammatory Treatments for Asthma
Managing asthma focuses on anti-inflammatory treatments to improve lung health. Different treatments work in various ways, helping doctors customize care. This approach targets the swelling in the airways.
Medications and Their Impact on Airway Health
Inhaled corticosteroids (ICS) are a key tool against asthma. They cut down inflammation, easing symptoms and flare-ups. Studies show these meds boost lung function and cut down on emergency inhaler use.
For those with hard-to-treat asthma, leukotriene modifiers and prednisone are options. These can greatly enhance a patient’s life when standard treatments don’t work.
Role of Biologics in Asthma Management
Biologics are a major leap forward, especially for severe asthma. They target specific parts of the immune system to reduce inflammation. For example, mepolizumab (Nucala) goes after IL-5 to lower the risk of bad asthma attacks.
Omalizumab (Xolair) works well for those with serious allergic asthma. Reslizumab (Cinqair) helps by decreasing eosinophils, which cause asthma symptoms. Biologics represent a new, precise way to handle the chronic inflammation seen in asthma.
Conclusion
Over 25 million people in the United States face the challenges of asthma and chronic inflammation. Understanding these conditions, especially how inflammation works and the impact of the environment, is key for effective management. Nearly 60% of asthma patients suffer from allergic asthma, pointing to the need to tackle indoor allergens like house dust mites.
Advancements in research and treatment, such as biologics and targeted therapies, bring hope to those fighting for better lung health. The widespread nature of asthma doesn’t just affect one’s physical health. It also impacts their quality of life, with many struggling to control their symptoms.
This struggle emphasizes the need for strategies that include both medical care and lifestyle changes. The link between chronic inflammation and asthma highlights how vital ongoing education and awareness are. They help reduce the triggers that worsen asthma.
By addressing physiological responses and environmental factors, people can greatly reduce asthma’s effect on their life. In 2016, asthma led to nearly 420,000 deaths globally. This fact underlines the crucial need for cooperation among patients, healthcare providers, and researchers. Together, they can strive for better asthma care and healthier lungs for everyone.