Did you know a recent study found a strong inverse relationship between allergies and lung cancer? The odds ratio (OR) was only 0.55. This suggests people with allergies might have a lower chance of getting lung cancer. As more people suffer from allergies, it’s important to understand how it affects lung cancer diagnosis. We will look into how allergies might hide or confuse lung cancer symptoms, which can cause wrong diagnoses.
It’s been found that 60-95% of those with asthma also have allergic rhinitis. Recognizing these symptoms is crucial due to their impact on health. The link between allergies and lung cancer diagnosis is getting more attention. Accurate diagnosis is key, especially as allergies become more common. This highlights the need for both doctors and patients to be more aware.
Key Takeaways
- The strong inverse relationship between allergic rhinitis and lung cancer may lead to decreased risk perceptions.
- Asthma, prevalent in allergy sufferers, can complicate lung cancer diagnoses.
- Allergies might obscure critical signs of lung cancer, leading to misdiagnosis.
- Recent studies indicate that individuals with a history of allergies could experience reduced lung cancer risk.
- Increased awareness of allergy impacts is crucial for healthcare professionals in diagnostics.
Understanding Allergies: A Growing Health Concern
Allergies are a big problem for many people, especially in developed places. About 20% of people face them. Allergic rhinitis is very common. It causes sneezing, itchy eyes, and can lead to more serious issues. Knowing about allergies is important. It’s especially true because they can be related to other problems like asthma.
Asthma affects a huge number of people globally – around 300 million. For those with asthma, there’s a 25% higher chance of getting lung cancer. This fact shows how critical it is to understand allergies and asthma. They can have a big impact on health. There’s growing interest in how allergies might increase cancer risks, lung cancer included.
Studies have found a complicated link between allergies and cancer. Out of nearly 6,000 articles reviewed, 312 found connections between allergies and cancer. This information means we need to look more into how allergies, rhinitis, and asthma relate to serious health issues.
To wrap up, allergies and asthma bring many health problems. It’s very important to understand their role in diseases like lung cancer. This understanding could lead to better care and ways to prevent health issues.
The Prevalence of Lung Cancer in the United States
Lung cancer is the top cause of cancer-related deaths in the U.S. About 80% of these deaths come from smoking. This highlights the urgent need for programs to help people stop smoking and other health efforts.
Lung cancer is the second most common cancer, making up 11.4% of all cases. Secondhand smoke is a big cause, right after radon exposure. These environmental risks are major concerns.
Working with dangerous substances like asbestos or diesel exhaust increases lung cancer risk. Smoking and taking beta-carotene supplements can make this even worse. It shows how lifestyle choices affect lung cancer rates.
Worldwide, lung cancer is behind 18% of all cancer deaths. In the U.S., almost half of the people diagnosed have cancer that has spread far. But catching lung cancer early gives a much better chance of survival, with a 5-year survival rate over 60%.
It’s key to know these facts to create good screening and prevention plans. This can lead to better chances for people at risk.
| Risk Factors | Contribution to Lung Cancer |
|---|---|
| Smoking | About 80% of lung cancer deaths |
| Secondhand Smoke | Third most common cause |
| Radon Exposure | Second-leading cause |
| Workplace Asbestos | Significantly increases risk |
| Diesel Exhaust | Increases risk |
| Previous Radiation Therapy | Higher risk of lung cancer |
| Family History | Higher risk of developing lung cancer |
Common Symptoms of Lung Cancer and Allergies
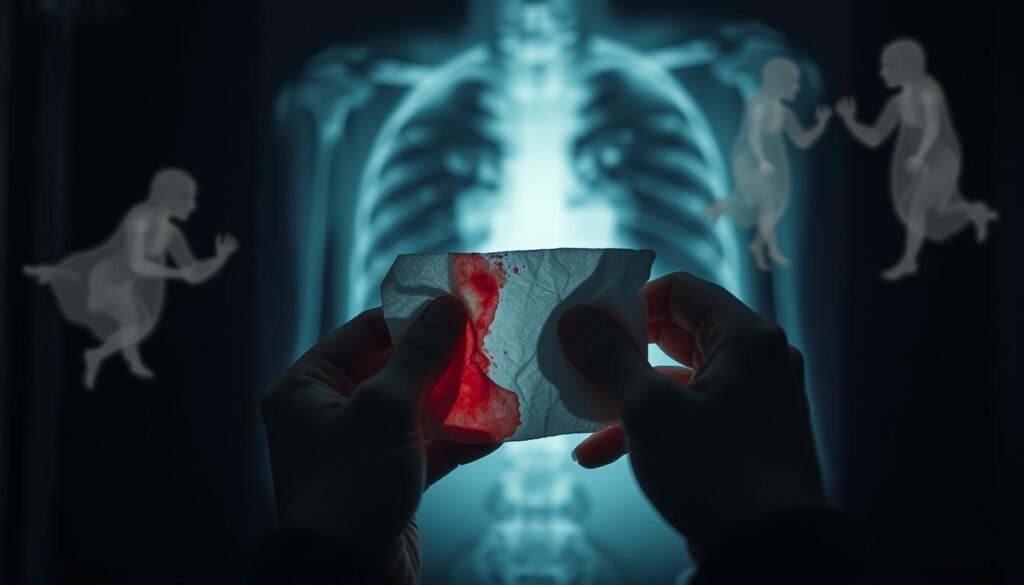
Lung cancer symptoms often look like allergy symptoms. This similarity makes it hard to figure out the real problem. People might think their allergy signs are actually lung cancer signs. These signs include coughing, chest pain, finding it hard to breathe, and feeling very tired. Knowing these shared symptoms helps doctors and patients make better decisions.
Allergy symptoms, like coughing, feeling tightness in the chest, and breathing issues, can be mistaken for lung cancer signs. Every year, over 50 million people in the U.S. deal with allergies. This makes figuring out if symptoms are from allergies or lung cancer even more difficult. Allergic reactions make airways swollen. This might lead some to wrongly think they have lung cancer. This mistake can delay getting the right tests for lung cancer.
It’s crucial for doctors to look at all symptoms closely. They need to tell apart lung cancer from allergy issues. Being aware of the symptoms that lung cancer and allergies share is key. This helps in giving the right treatment quickly. Good treatment can improve how well patients do.
| Common Symptoms | Lung Cancer | Allergies |
|---|---|---|
| Coughing | Persistent, often worsening over time | May include sneezing or runny nose |
| Chest pain | Often sharp, persistent | Rarely severe, more associated with pressure |
| Shortness of breath | Progressively increases with exertion | Acute episodes during exposure to allergens |
| Fatigue | Chronic tiredness, weight loss may occur | Occasional fatigue due to allergic reactions |
Understanding both common symptoms of lung cancer and symptoms of allergies helps everyone. It lowers the chance of making a wrong diagnosis. So, patients can get the right help they need sooner.
Allergic Reactions and Their Impact on Health
Allergic reactions greatly influence our health, notably affecting asthma and lung health. Those with asthma often face IgE-mediated immune responses. This can hurt lung function and raise the risk of further issues. Recent studies show allergies and cancer risk may be linked. Allergies to air substances from plants, grass, and trees might up the risk of blood cancers.
Research found that people allergic to certain things might get a type of lymphoma more often. Being allergic to cats and dogs can also lead to more cases of plasma-cell neoplasms. This shows how different allergens have a broad health impact.
It seems women are more prone to blood cancers from these allergens than men. Scientists looked at smoking, diet, and how people rated their health. They based their conclusions on data from over 66,000 people, which gave deep insights into cancer risks.
Healthcare workers need to know how allergic reactions can hide cancer symptoms. If symptoms keep up, seeing a doctor is crucial to avoid wrong diagnoses. Allergies can look like or hide signs of severe lung problems, even lung cancer. For more on how conditions can be confused with lung cancer, check out this helpful link.

| Type of Allergy | Associated Health Risk |
|---|---|
| Pollen (plants, grass, trees) | Increased risk of lymphoma |
| Pets (cats, dogs) | Higher risk of plasma-cell neoplasms |
| Seasonal allergies | Potential for complicating lung health |
| Food allergies | Can lead to severe reactions |
The Role of Allergies in Misdiagnosed Lung Cancer Cases
There’s a complex link between allergies and lung cancer that impacts diagnoses. Research shows that allergies, especially those with IgE reactions, can change the diagnosis of lung cancer. It’s key to look at the correlation between allergies and lung cancer risk. This means doctors should check for allergy history when diagnosing.
Correlation Between Allergies and Lung Cancer
Recent research finds that cancer patients have fewer IgE-related allergies than others. For example, the chances of having allergic rhinitis, atopic dermatitis, and asthma are lower in cancer patients. This suggests a strong correlation between allergies and lung cancer. Lung cancer patients report fewer allergy issues.
Epidemiological Evidence from Recent Studies
Many epidemiological studies looked at allergies in lung cancer patients. They noticed cancer patients had lower average IgE levels than healthy people, 45.98 versus 83.2 IU/l. Also, cancer patients were less likely to have allergic rhinitis, atopic dermatitis, and asthma. This info might help catch lung cancer early, avoiding misdiagnosis.
These findings stress the need to consider allergies when checking for lung cancer. This could avoid wrong diagnoses because of similar symptoms. Knowing about allergies might make diagnoses more accurate and help patients better.
Misdiagnosis in Lung Cancer Patients: A Critical Issue
Lung cancer misdiagnosis is a big problem in our health system. Many people don’t get the right treatment on time because lung cancer signs often look like other illnesses, like allergies. When symptoms like a long-lasting cough and chest pain are mistaken for less serious conditions, it leads to dangerous delays in treatment.
Research shows that early-stage lung cancer is incorrectly diagnosed 20% to 50% of the time in X-rays. This alarming fact highlights the struggles faced by both patients and doctors. Missing lung cancer in chest X-rays not only worsens the person’s outlook but can also mean the disease is much advanced when finally discovered.
Misdiagnoses happen due to several reasons, including observer error, how the tumor looks, and technical difficulties. Errors in seeing the issue, recognizing it, and making the right decision are main contributors. Knowing about common missed spots in X-rays, especially in the upper parts of the lungs, can help improve patient outcomes. Paying extra attention to areas like near the heart and lung routes is key to catching missed cases early.
It’s vital to tackle these issues to better patient care and results. People can take an active role in their healthcare by knowing the key symptoms and pushing for thorough checks. Getting a second opinion and talking about different tests can help one navigate through the healthcare system better. For details on how wrong diagnoses in lung cancer affect patients, visit this resource. Knowing the warning signs and the value of quick action can greatly impact lung cancer survival rates. For more tips on early detection and symptom recognition, see this guide.
Exploring the Connection Between Allergies and Lung Cancer Misdiagnosis
The connection between allergies and lung cancer misdiagnosis is a key concern for doctors. Allergies can cause symptoms that look like lung cancer. This can lead to the wrong diagnosis and affect treatment choices. Asthma is seen as a risk for lung cancer. The International Lung Cancer Consortium (ILCCO) found asthma patients have a 1.28 times higher risk of lung cancer. This information shows doctors need to carefully examine symptoms that could be lung cancer.
Statistics show asthma patients have a higher chance of getting squamous cell and small-cell carcinomas. Their risks are 1.69 and 1.71 times higher, respectively. This highlights the need for a detailed patient history and careful diagnosis. Wrongly thinking asthma symptoms are lung cancer can delay the right diagnosis. This delay can really impact patient care. Doctors must work hard to tell the difference between allergy symptoms and signs of lung cancer.
Also, the risk of lung cancer is much higher in the first two years after an asthma diagnosis. The risk goes up to 2.13 times. But, if asthma was diagnosed over ten years ago, the risk isn’t as high. This shows the importance of regular check-ups for asthma patients. Especially in the years right after they’re diagnosed.
Understanding how allergies and lung cancer misdiagnosis overlap is crucial for better diagnosis and quick treatment. Healthcare workers need to look at patient history and symptoms together. This way, they can navigate the complex issues this connection brings.
| Type of Cancer | Relative Risk (RR) | Confidence Interval (CI) | Time Frame Post-Asthma Diagnosis |
|---|---|---|---|
| Total Lung Cancer | 1.28 | 1.16–1.41 | General |
| Squamous Cell Carcinoma | 1.69 | 1.26–2.26 | General |
| Small-Cell Carcinoma | 1.71 | 0.99–2.95 | General |
| Adenocarcinoma | 1.09 | 0.88–1.36 | General |
| Risk After 2 Years | 2.13 | 1.09–4.17 | Within 2 years |
This deep dive into the data shows why accurate assessment is so important. It underlines the role of patient care when managing allergies and diagnosing lung cancer.
Common Diagnostic Tests: Challenges and Limitations
Diagnosing lung cancer can be difficult. The usual tests, like CT scans and X-rays, have big challenges and limits. They may show nodules that don’t actually mean cancer, because non-cancer issues like chronic lung conditions or allergies can look the same. This makes understanding test results tough and raises the risk of wrong diagnoses.
In the US, less than 20% of lung cancer cases are found early when they are still localized. This makes treatment harder. Even though screening with low-dose computed tomography (LDCT) can cut death rates by 20% to 39%, it’s not used enough. Only 12.5% of people who should get the screening actually do. This shows a big gap in catching the disease early.
It’s key to know these problems to make testing better and help patients more. If we can use tests more wisely, we can find cancer earlier and plan treatments better. Too many screenings end up being false alarms—81% aren’t accurate. We need to fix this. We must make sure high-risk people are watched closely. For deeper knowledge on diagnostics in lung cancer, check this source.