Did you know about 1 in 16 men and 1 in 17 women will face lung cancer? This fact shows how big of an issue lung cancer is in the US. In 2024, experts expect around 234,580 new lung cancer cases and about 125,070 deaths. Lung cancer is the top reason for cancer deaths globally, presenting a significant health challenge.
Lung cancer’s fight is tough, with only about 19% of patients living five years after finding out they have it. This low survival rate shows we need better early detection and prevention.
Interestingly, 10% to 20% of lung cancer cases happen in people who never smoked much, if at all. This means 20,000 to 40,000 cases each year aren’t due to smoking. Radon and secondhand smoke also play a big part, causing many cases yearly. These facts stress the need for awareness and taking steps to protect our health.
Key Takeaways
- 1 in 16 men and 1 in 17 women will be diagnosed with lung cancer in their lifetime.
- 234,580 new cases of lung cancer are expected in the U.S. in 2024.
- 10% to 20% of cases are diagnosed in non-smokers.
- Lung cancer has a five-year survival rate of only 19% for all types.
- Secondhand smoke causes approximately 7,300 lung cancer cases annually.
- Radon exposure contributes to about 2,900 new lung cancer cases each year.
Introduction to Lung Cancer Statistics
Lung cancer is a major health issue in the United States. It’s the second most common cancer for both men and women. With a scary 20.4% of all cancer deaths, its impact is huge. This year, about 234,580 new cases are expected. That’s 11.7% of all new cancer diagnoses.
Most people are around 70 years old when they get diagnosed. Thanks to anti-smoking efforts, we’re seeing fewer cases and deaths each year. About 5.7% of people will face lung and bronchus cancer in their lifetime. Understanding lung cancer risk factors is key.
The five-year survival rate for lung cancer patients has gotten better, now at 26.7%. Localized cases have even better odds, with a 63.7% survival rate. Many things affect a patient’s outlook, like age, whether they smoked, and the cancer type.
For more details on lung cancer, including risks and how it affects different groups, check out detailed lung cancer statistics.
Lung Cancer Types and Their Statistics
Lung cancer is divided into two main kinds: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Each type is unique and affects how patients are treated and their survival chances. NSCLC is the more common type, making up about 80%-85% of all lung cancer cases. On the other hand, SCLC accounts for 10%-15% of cases and is usually more aggressive.
NSCLC includes different subtypes like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. These subtypes behave differently, so it’s crucial to understand them. Knowing the specific subtype of non-small cell lung cancer helps predict how well treatments might work and what the outcomes could be.
In the U.S., lung cancer is the top cancer killer. It’s expected that around 234,580 new cases will be found in 2024. Furthermore, around 125,070 people die from it every year. It’s vital to catch it early because early detection can greatly improve survival chances by up to 20% in those at high risk.
Talking about treatment choices and understanding lung cancer statistics is critical. Lung cancer takes as many lives yearly as breast, prostate, and pancreatic cancers combined. So, there’s a great need for more research funds, education on risks, and symptoms awareness.
| Lung Cancer Type | Percentage of Cases | Characteristics |
|---|---|---|
| Non-Small Cell Lung Cancer (NSCLC) | 80%-85% | Includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma |
| Small Cell Lung Cancer (SCLC) | 10%-15% | More aggressive; often spreads quickly |
Understanding lung cancer’s different types can help patients and families make better decisions about their care.
Lifetime Risk of Lung Cancer
The lifetime risk of lung cancer is a critical stat. It shows the chance of getting this disease during one’s life. About 5.7% of people are likely to hear a lung cancer diagnosis. This number shows a clear gender gap. Men have a risk of 1 in 16. For women, it drops to about 1 in 17.
Risk for Men and Women
Men are more at risk of lung cancer than women. This fact highlights the need for health efforts tailored to each gender. Men not only have a higher risk but also face different outcomes based on race. Black men, for example, are 12% more likely to develop lung cancer than White men. This raises the need for greater awareness and preventive steps.
Demographic Variations in Risk
Different racial and age groups face varied lung cancer risks. For older adults, the disease is more common. This calls for focused awareness and screening for them. Meanwhile, Black women have a 16% lower lung cancer rate than White women. This difference points to the complex role demographics play in cancer risk.
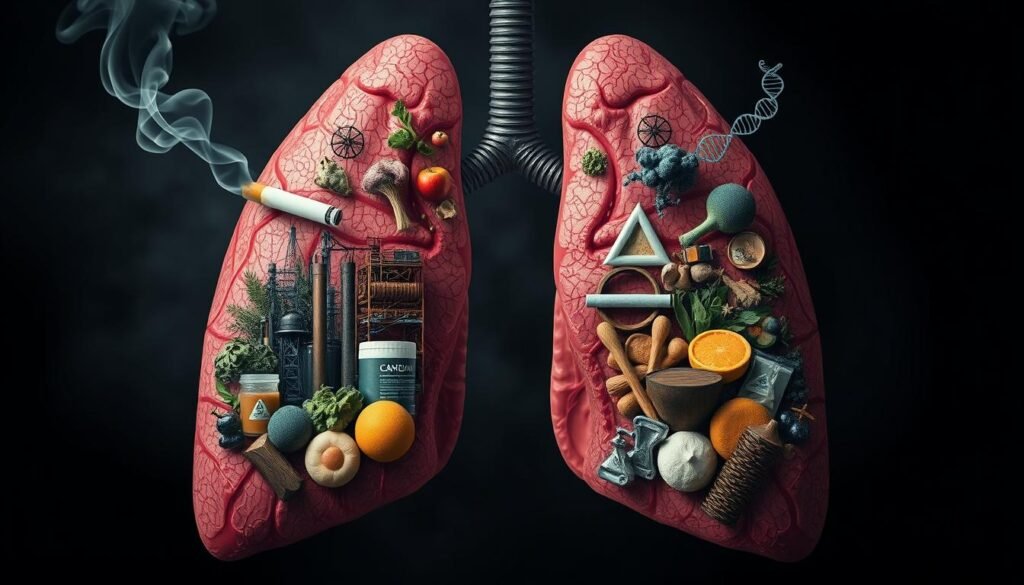
Understanding Lung Cancer Causes
Lung cancer is not easy to understand. It’s affected by many things. Smoking and radon gas exposure are key causes. Knowing these can help people make better health choices and reduce their risks.
Smoking and Lung Cancer
Smoking is the top reason for lung cancer, causing most deaths in the U.S. Smokers have a much higher chance of getting lung cancer. This is true for cigarettes, cigars, and pipes. If you stop smoking, you greatly reduce your lung cancer risk, no matter your age. Stopping is very important.
Being around smoke can also be harmful. Being near someone else’s smoke can increase your lung cancer risk. So, it’s key to have smoke-free places.
Radon Exposure
Radon exposure is a big concern too. This gas has no smell or color, and it builds up inside homes. It’s dangerous indoors and causes lung cancer in people who’ve never smoked. For smokers, the risk is even higher.
Many lung cancer cases in non-smokers come from radon. Other reasons include air pollution and workplace hazards. Knowing how these causes work together helps people make better health choices.
Occupational Hazards and Lung Cancer Risk
It’s important to understand the link between job dangers and lung cancer risk. This is key for keeping workplaces safe. Some jobs expose workers to bad stuff, which increases their chances of getting lung cancer. Working on ways to tackle these risks can help make jobs safer.
Common Occupational Hazards
Different jobs have different risks for lung cancer. Here are some risky substances:
- Asbestos: A harmful substance linked to lung cancer, found in building and ship making.
- Arsenic: People run into this in glass making and making bug killers.
- Beryllium: A risk in nuclear and space jobs, it’s bad for the lungs.
- Cadmium: Used in making batteries and covering metals, it can lead to lung cancer.
- Nickel: Exposure in making stuff can increase lung cancer chances.
- Chromium (VI): Found in making stainless steel and colors, it’s not good for lung health.
These substances are dangerous because they can cause cancer. Research shows that about 10% of lung cancers come from working with these things. This shows we need better rules and safety steps at work.
| Hazard | Primary Industries Affected | Significant Risk |
|---|---|---|
| Asbestos | Construction, Shipbuilding | High |
| Arsenic | Pesticide production, Glass Manufacturing | Moderate |
| Beryllium | Nuclear, Aerospace | High |
| Cadmium | Battery, Metal Plating | High |
| Nickel | Manufacturing | Moderate |
| Chromium (VI) | Steel Production, Pigment Manufacturing | High |
It’s crucial for workers and bosses to know about these job-related hazards. Taking steps to keep the workplace safe can really lower lung cancer risks. Making workplaces safer should be a top goal for dangerous jobs.
Environmental Factors Contributing to Lung Cancer
Understanding environmental factors is key in grasping lung cancer risks. Air pollution and secondhand smoke stand out as significant threats. Cities often face intense air pollution, which poses a risk for lung cancer in their residents. Identifying and tackling these factors is vital for prevention.
Air Pollution
In crowded areas, air pollution poses a great danger. It includes harmful particles and gases that can damage our lungs. Research shows it’s linked to many lung cancer cases, besides those from smoking. Thus, cutting down pollution and enhancing air quality is crucial for health and reducing cancer risks.
Secondhand Smoke Effects
Secondhand smoke poses a well-known danger to health, increasing lung cancer risks. Non-smokers exposed to it have a higher chance of getting lung cancer. Protecting people from tobacco smoke in public and private spaces is key. Efforts to reduce secondhand smoke exposure can lower lung cancer rates.
| Environmental Factor | Impact on Lung Cancer | Preventive Measures |
|---|---|---|
| Air Pollution | Increases lung cancer risk due to harmful particles and gases | Implementing stricter emissions regulations and promoting clean air initiatives |
| Secondhand Smoke | Significantly raises the likelihood of lung cancer in non-smokers | Enforcing smoking bans in public areas and encouraging smoking cessation programs |
Family History and Genetic Factors
Knowing if lung cancer runs in the family is key to gauging one’s risk. Having close relatives with lung cancer may increase your risk because of genetics. Studies show that having a first-degree relative with lung cancer, particularly if diagnosed before 60, greatly increases your chances.
If both relatives were diagnosed early, your risk jumps even higher. This shows the strong link between inherited risks and lung cancer.
Genetics play a complex role in lung cancer. Studies have found that lung cancer often runs in families. This hints at a strong genetic factor. Scientists have pinpointed a crucial gene area on chromosome 6q23-35 linked to lung cancer.
Those with early-onset lung cancer in the family are at most risk. This highlights the importance of knowing your family health history.
Getting to know your family’s lung cancer history is useful. Consider genetic counseling and testing if you think you’re at risk. This information can help create personal plans for lung cancer prevention. Informed decisions can then be made, empowering individuals with a family history of lung cancer.
| Family History | Increased Risk | Genetic Factors | Significant Findings |
|---|---|---|---|
| First-degree relatives with lung cancer | Odds Ratio: 4.89 (if diagnosed before 60) | Chromosome 6q23-35 susceptibility locus identified | Higher incidence in early-onset cases |
| Familial patterns | Elevated risk observed in multiple studies | Familial aggregation evident | Significant indirect evidence of genetic influence |
Lung Cancer Prevention Strategies
Preventing lung cancer is key to reducing new cases and saving lives. There are two main strategies: quit smoking and cut down on radon exposure. By tackling these, people can greatly lower their chances of getting this serious disease.
Quitting Smoking
Quitting smoking is a major way to prevent lung cancer. It’s linked to about 90% of all lung cancer cases. Smokers are 20 times more likely to get lung cancer than those who don’t smoke. Quitting smoking lowers the chance of getting lung cancer and reduces death from the disease. Support programs are crucial in helping lower lung cancer rates.
Reducing Radon Exposure
Lowering radon exposure is also crucial. Radon is a natural, radioactive gas that can build up in homes. High radon levels are especially a concern in certain areas. Testing for radon is crucial, especially in places known for it. Using mitigation actions like better ventilation can lower radon levels. Since radon exposure ups the risk of lung cancer, especially for smokers, taking action is very important.

The Importance of Lung Cancer Screening
Lung cancer screening is key to improving survival rates. It helps find the disease early, increasing treatment success chances. People aged 50 to 80 with 20 pack-years of smoking are advised to get yearly low-dose CT scans. This is crucial for raising awareness and talking to doctors about lung cancer.
Screening Guidelines and Recommendations
The National Lung Screening Trial shows low-dose CT scans lower lung cancer deaths by 20% among high-risk folks. These are people aged 55 to 74 with a long history of smoking. Other studies show a 24% drop in deaths with these scans. This highlights important screening guidelines.
Benefits of Early Detection
Spotting lung cancer early through screening is hugely beneficial. Low-dose CT scans find way more early-stage cancers than x-rays. This means more people get diagnosed at stage I, making treatments more likely to work. Early detection greatly boosts survival rates. Low-dose CT scans are especially good at finding tiny tumors, increasing early diagnosis.
Current Lung Cancer Survival Rates
The fight against lung cancer has seen progress, thanks to better treatments and catching it early. From 2012 to 2018, the overall 5-year survival rate for all types of non-small cell lung cancer (NSCLC) was about 28%. If the cancer is found early and is still local, the survival rate jumps to 65%. But, if it’s at a regional stage, the rate falls to 37%.
For those with cancer that has spread far, the situation is tougher. Their survival rate is just 9%. Small cell lung cancer (SCLC) has its own numbers. If SCLC is caught while it’s still local, the 5-year survival rate is 30%. This drops to 18% for cases found at a regional stage and to a grim 3% for distant cases. For SCLC overall, the average 5-year survival rate is around 7%.
This shows how crucial early detection and specific treatment plans are for improving chances of survival.

There’s a difference in survival rates between men and women. From 1999 to 2006, women had a 5-year survival rate of 19%, while men had 14%. Also, men have a 1 in 13 chance of getting lung cancer, while women have a 1 in 16 chance in the U.S.
These statistics highlight important trends. They help doctors and patients choose the best approach to fight cancer.
Ongoing research and developments in cancer treatment are making a positive impact. They’re giving hope to many dealing with lung cancer. With continued focus on education, prevention, and early detection, we aim for even better results ahead.
Conclusion
Lung cancer is a major public health issue, especially in groups where smoking is common. This overview shows that both genes and the environment play roles in increasing lung cancer risk. It’s vital to keep pushing for awareness about lung cancer. This will help in preventing the disease and catching it early, which can save lives.
Studies reveal that having family members with lung cancer raises your risk, especially if they were diagnosed before 60. It’s key to know if lung cancer runs in your family. Early detection and regular screenings can make treatments more effective. This can lead to a hopeful future in battling lung cancer.
As science moves forward, merging research on smokers and non-smokers helps us better understand risk factors. For more info on how radiation affects lung cancer risk, visit this resource. Knowing the early signs of lung cancer and raising awareness of these symptoms can lower the disease’s rates. This promises a better future in treating and managing lung cancer.