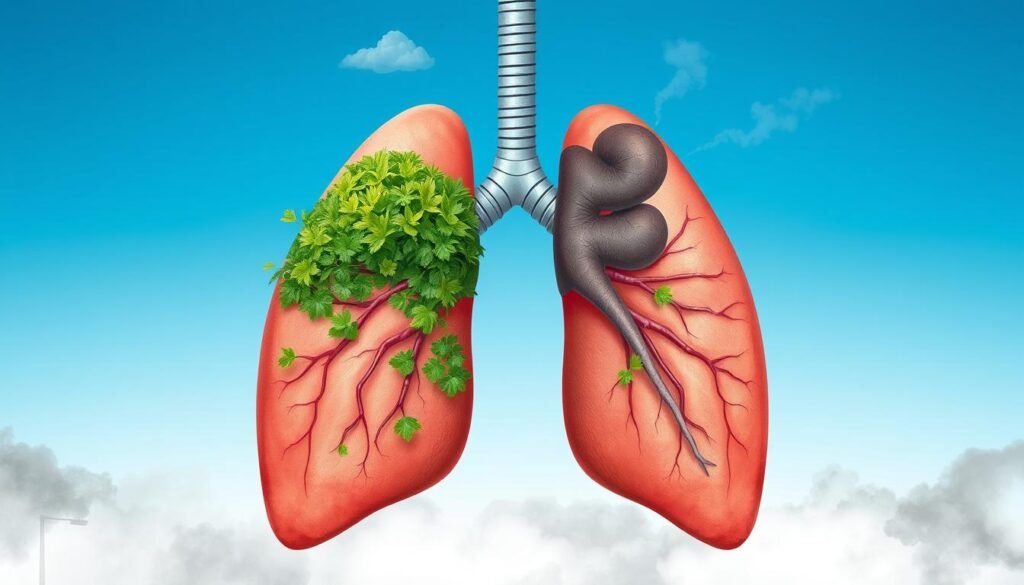
Cigarette smoking causes about 80% to 90% of lung cancer deaths in the U.S. This fact shows how crucial it is to know what raises the risk of lung cancer. Several main things increase this risk. These include using tobacco, being around secondhand smoke, and environmental factors.
People who smoke are 15 to 30 times more likely to get lung cancer than those who don’t. It’s not just people who smoke a lot who are at risk. Even smoking once in a while can harm your lungs.
But there’s more to the story than just smoking. The air quality inside homes and dangerous substances like radon and asbestos also matter. These are especially risky for people who are more likely to get the disease because of their genes or family history. We’re learning more about how these factors come together. So, it’s vital to prevent these risks and tell people about what contributes to lung cancer. Knowing all this helps individuals make better health decisions.
Key Takeaways
- 80% to 90% of lung cancer deaths are linked to cigarette smoking.
- Smoking increases lung cancer risk by 15 to 30 times for individuals compared to non-smokers.
- Secondhand smoke also contributes significantly to lung cancer cases.
- Radon exposure, particularly in indoor environments, is a major risk factor.
- Occupational hazards from substances like asbestos and diesel exhaust raise lung cancer risks.
Understanding Lung Cancer Risk Factors
Lung cancer leads in cancer deaths worldwide. Knowing the risk factors is crucial for everyone and public health efforts. There are modifiable and non-modifiable risk factors. Things like smoking can be changed, but age and family history cannot.
It’s widely thought that smoking alone causes lung cancer. Yet, people who’ve never smoked also get lung cancer. This shows the need for thorough cancer prevention education. Other risks include radon gas, previous radiation treatments, family health history, and certain job exposures.
Smoking a lot and for a long time raises lung cancer risk. But quitting smoking can lower this risk greatly. Knowing these risks helps people make smarter choices and find ways to prevent lung cancer.
The Dominance of Smoking in Lung Cancer Risk
Smoking is the top risk factor for lung cancer. It leads to many cases and deaths. Studies show a strong link between smoking and lung cancer risk. Smokers, especially men, are 23 times more likely to get lung cancer than non-smokers.
Statistics on Smoking and Lung Cancer
Smoking causes 80% to 90% of lung cancer deaths in the U.S. The Surgeon General’s 2004 report confirmed smoking’s link to cancers, like lung and bladder cancer. Lung cancer in never-smokers is also a major concern globally. It’s the seventh most common cancer. Rare cases in young patients are being studied for genetic causes.
Impact of Cigar and Pipe Smoking
Cigars and pipes are just as harmful as cigarettes. They contain the same cancer-causing compounds. For example, both have polycyclic aromatic hydrocarbons and nitrosamines. Cigar smoking risks come from the high levels of carcinogens in each puff. Meanwhile, pipe smoking risks are often ignored. Yet, they are linked to serious health issues, including cancers. Experts continue to study these risks to help stop tobacco use.
Secondhand Smoke Exposure and Its Effects
Secondhand smoke exposure is a major public health issue. It’s the third leading cause of lung cancer in the U.S. Those who don’t smoke but are around environmental tobacco smoke face a bigger risk of getting lung cancer. Research shows a 20-30% increase in lung cancer rates because of secondhand smoke.
But secondhand smoke doesn’t only cause lung cancer. For example, women exposed while pregnant may have babies with low birth weight. This can lead to many health problems for the baby. Children breathing in secondhand smoke face serious health issues. They can get lung infections like pneumonia and bronchitis. They are also at a higher risk for sudden infant death syndrome (SIDS).
- Non-smokers exposed to secondhand smoke suffer nearly 34,000 premature deaths from heart disease each year.
- The risk of stroke increases by 20–30% among non-smoking adults exposed to secondhand smoke.
- More than 19,000 deaths annually in the United States are attributed to secondhand tobacco smoke.
- Children face elevated risks of conditions such as fluid in their ears and increased frequency of ear infections, often requiring operations like ear tube drainage.
It’s important to understand how dangerous secondhand smoke is. This knowledge can help protect non-smokers. By addressing these dangers, we can improve public health and safety. For more details on lung cancer causes and effects, see this resource.
| Health Effects | Statistics |
|---|---|
| Lung Cancer Deaths Among Non-Smokers | More than 7,300 annually |
| Increased Risk of Lung Cancer | 20–30% for non-smokers exposed to secondhand smoke |
| Premature Deaths from Heart Disease | About 34,000 annually in the U.S. |
| Pregnant Women’s Risks | Increased likelihood of low birth weight infants |
| Children’s Risks | Increased risks for SIDS and respiratory infections |
Environmental Risks: The Role of Air Pollution
Air pollution greatly affects our health, causing issues like lung cancer. Cities often have more pollution, raising concerns about air quality and cancer. The World Health Organization says air dirt can cause lung cancer. It’s important to tackle these environmental dangers.
Air Quality and Lung Cancer Correlation
Studies show a link between air pollution and lung cancer. Places with more air dirt see more lung cancer cases, especially in certain groups. A small increase in PM 2.5 particles can lead to 9 percent more lung cancer cases. Kids, the elderly, and the sick are more at risk, showing we need better air.
Diesel Exhaust and Its Contribution to Risk
Diesel smoke is a big pollution source, raising lung cancer risks. It has cancer-causing parts, adding to environmental cancer dangers. Long contact with diesel smoke or wildfire smoke makes health worse. It can cause more breathing diseases. We must act fast to make the air cleaner.

The Risk of Lung Cancer Increases with Occupational Hazards
Occupational hazards are linked to a higher risk of lung cancer. In many workplaces, workers come into contact with dangerous substances. These substances, like asbestos, uranium, arsenic, and cadmium, can lead to lung cancer.
Common Workplace Carcinogens
Some jobs have a higher exposure to carcinogens. Common ones include:
- Asbestos
- Arsenic
- Diesel exhaust
- Chromium
- Nickel
Workers in rubber manufacturing, iron and steel, and painting are more at risk. This is because they’re often exposed to harmful materials. Such exposure can result in severe health issues later.
Asbestos Exposure and Related Risks
Asbestos is well-known for its link to lung cancer. Construction and manufacturing workers face a higher risk. They might come across asbestos directly or indirectly. And it’s not just the workers; their families are at risk too. Asbestos fibers can stick to clothes, posing a risk at home.
The Importance of Safety Regulations
To reduce these risks, there must be strict safety rules. By following safety measures, we can lower the exposure to carcinogens. Training, ventilation, and protective gear are key to keeping workers safe. It’s vital to keep improving these rules to protect against lung cancer from work hazards.
Radon Exposure: A Stealthy Risk Factor
Radon gas comes from the breaking down of uranium in soil and rocks. This invisible gas can enter homes undetected, raising the risk of lung cancer. In fact, it’s the second main cause of lung cancer in the U.S., linked to about 21,000 deaths yearly. This includes those who have never smoked. Knowing about radon’s dangers is key to a healthy home.
What Is Radon and How Does It Affect Health?
Radon is worrying because it’s closely linked to lung cancer. The EPA warns that any radon level can be harmful. They say to take action if levels hit 4 pCi/L or higher. Yet many people don’t know about the risks radon brings to their homes. It’s even worse for smokers, as radon greatly increases their lung cancer risk.
Testing for Radon in Homes
It’s crucial to test your home for radon regularly. The EPA suggests testing every two years or after making changes to your home. Testing is easy with available kits. If radon levels are high, solutions like sub-slab depressurization can make a big difference.

| Radon Level (pCi/L) | Risk Level | Actions Recommended |
|---|---|---|
| Below 2.0 | Low | Consider testing periodically |
| 2.0 – 4.0 | Moderate | Regular testing advised |
| At or above 4.0 | High | Immediate mitigation required |
Dealing with radon is crucial for clean air at home and lowering lung cancer risk. Everyone should test their homes and use fixes if needed. Such steps are key to protecting our health.
Family History and Lung Cancer Risk
Family history is key in determining lung cancer risk. If lung cancer runs in the family, you’re more at risk. This is especially true when genetic factors meet environmental ones. The mix of inherited cancer traits and the environment matters a lot.
Genetic Factors in Lung Cancer
Having a close family member with lung cancer can up your risk. Your risk can go 1.51 times higher, even when other factors are considered. Siblings face the highest risk, with their odds going up to 1.82.
Even if you’ve never smoked, a family history can still increase your risk. If a sibling has lung cancer, your risk rises, showing an odds ratio of 1.44. Genetics play a big role in our vulnerability to lung cancer.
Shared Environmental Risks within Families
Families often face the same environmental risks for lung cancer. Secondhand smoke is a major risk for those with a lung cancer history in the family. Also, a family history of chronic bronchitis is linked with higher lung cancer risk. It’s crucial for families to understand these risks to prevent cancer in the future.
Chronic Obstructive Pulmonary Disease (COPD) and Cancer Risk
COPD greatly affects lung health and raises the chance of getting lung cancer. This disease slows down airflow and changes how the lungs work. This makes it easier for cancer to start. Studies have shown a strong link between COPD and lung cancer. They tell us how vital lung health is in figuring out cancer risk.
How COPD Changes Lung Health
People with COPD often see their lung health get worse. The disease causes ongoing inflammation and harms lung tissue. This makes it easier for cancer-causing substances to do damage. Important data shows how COPD and cancer are connected:
| Statistic | Value |
|---|---|
| Global Prevalence of COPD | Approximately 251 million people |
| Health Expenditure in Australia | $929 million per annum |
| Percentage of Adults with COPD (Developed World) | 8–10% |
| Percentage of Smokers with COPD | 15–20% |
| Projected Deaths from Lung Cancer by 2030 | 10 million per year |
| 5-Year Survival Rate for Lung Cancer Patients | 16% |
| Lung Cancer Deaths Attributed to COPD | 4% to 33% of total deaths |
| Relative Risk increase of Lung Cancer with COPD | 4- to 6-fold |
In smokers, COPD comes before lung cancer in 70–80% of cases. Small drops in airflow are closely tied to a higher risk of lung cancer. Even slight airflow problems can greatly increase the risk of cancer.
It’s key to understand how COPD affects lung health. Experts think COPD will soon be the third leading cause of death worldwide. We need to know more about its link to lung cancer. By taking care of our lungs, we can lower our cancer risk and live healthier.
Advanced Age as a Risk Factor for Lung Cancer
Being older significantly increases the risk of lung cancer. This is especially true for those in their later years. As people age, their chances of getting this disease go up. This increase is due to more exposure to harmful substances like pollution and tobacco smoke.
Smoking is a top reason why men over 65 get lung cancer. For women of the same age, the risk depends on if they smoked and when they quit. These factors are crucial in understanding lung cancer risks.
Most lung cancer patients are older adults, with 61% being over 70. In the U.S., about 68% are diagnosed after turning 65. Only a small fraction, less than 0.5%, of lung cancer deaths happen in those under 40. The average age for lung cancer diagnosis is about 70. This shows why it’s vital for older people to get regular health checks.
As people get older, their immune system gets weaker. Also, they have more inflammation, which can lead to cancer. Often, lung cancer in the elderly is found early, especially in those over 75.
It’s important for older individuals to know about lung cancer risks. Being aware and getting screened early can improve survival chances. For more info on lung cancer and screening, visit Lung Cancer Awareness Month.
| Age Group | Lung Cancer Incidence |
|---|---|
| Under 40 | Less than 0.5% |
| 65 and older | 68% |
| 70 and older | 61% |
| 80 and older | 14% |
Genetics and Their Role in Lung Cancer Development
The study of lung cancer shows that genetics play a big part. Many studies have shown that some people are more likely to get lung cancer because of their genetics. This means it’s very important to understand your family’s health history.
Inherited Susceptibility to Lung Cancer
About 10 to 25 percent of lung cancers happen in those who never smoked. This highlights the importance of genetics. Research has found around 50 DNA spots linked to lung cancer, showing who may be at higher risk.
Mutations in genes like TP53, EGFR, and KRAS are common in lung cancer. These changes in genes are important clues for cancer screening and prevention. Knowing about these can help in getting the right treatment early.
Studies with twins and families have helped us understand genetics in cancer. They show that 8 to 20 percent of lung cancer risk is due to genetics. In Asia, 80 percent of women with lung cancer never smoked, pointing to genetics. This highlights why genetic counseling is crucial for those with a family history of lung cancer.
| Genetic Factor | Role in Lung Cancer |
|---|---|
| TP53 Gene | Common mutation in lung cancers, linked to tumor suppression failure. |
| EGFR Gene | Involves mutations that can lead to uncontrolled cell growth. |
| KRAS Gene | Mutations associated with a worse prognosis in lung cancer patients. |
| Inherited Risk Variants | Potentially increase susceptibility to lung cancer, significant in families with histories of the disease. |
Studying lung cancer genetics could lead to better screening and treatment. Knowing about inherited risks is crucial. This helps in making health strategies for everyone. The goal is to find ways to reduce the risk posed by genetics.
The Impact of Diet and Supplements on Lung Cancer Risk
Studies have shown a link between what we eat and lung cancer risk. Researchers have looked closely at vitamins and dietary supplements. They found that some vitamins can be good for our health. But some can be harmful, especially for people who smoke.
Efficacy of Vitamins in Cancer Prevention
Research indicates that some vitamins might lower lung cancer risk. Vitamin C stands out in this area. Studies show that getting vitamin C from food can reduce lung cancer risk. The risk decreases to 0.82 for those who get their vitamin C from food, not supplements. Eating a balanced diet full of different vitamins and minerals may cut down lung cancer risk.
The Risks of Beta-Carotene for Smokers
But, beta-carotene supplements can be risky for smokers. Studies have found that they might raise lung cancer risk in male smokers. It’s important to eat healthily and know the risks of some supplements. Smokers should talk to doctors before starting any new supplements. This advice is to make sure they do not harm their lung health.
Conclusion
Lung cancer risk is shaped by many factors. This article has shown the importance of being aware of these risks. From smoking to environmental dangers like pollution and radon, knowing these risks helps us see the big picture. It’s also crucial to understand how our choices and job risks affect our health.
Lung cancer is one of the top causes of cancer deaths around the world, affecting millions. By screening early, we can save lives. But, very few high-risk individuals get screened. This shows we must do better in making cancer prevention techniques available to everyone. Building understanding, screening, and learning can greatly lower lung cancer cases.
It’s important for everyone to think about their health and family history concerning lung cancer. Efforts to encourage screenings, cut down tobacco use, and clean the air can help reduce lung cancer numbers. Armed with knowledge on risks and how to prevent them, people can make smart choices for their health.