Lung nodules often appear in CT scans, but over 90% are benign. This fact highlights the importance of knowing what increases the risk of cancer. The American Thoracic Society (ATS) has found that small nodules rarely turn into lung cancer. Less than 5% do so. Understanding personal risk factors and nodule characteristics is key. This helps doctors and patients decide the best steps to take.
Key Takeaways
- Most lung nodules seen in CT scans are benign.
- Monitoring nodule growth can take several months to a year.
- The characteristics of nodules, such as size and growth rate, play a critical role in assessing cancer risk.
- Biopsy results are essential for determining treatment options.
- Early detection of lung nodules significantly influences treatment outcomes.
Understanding Lung Nodules
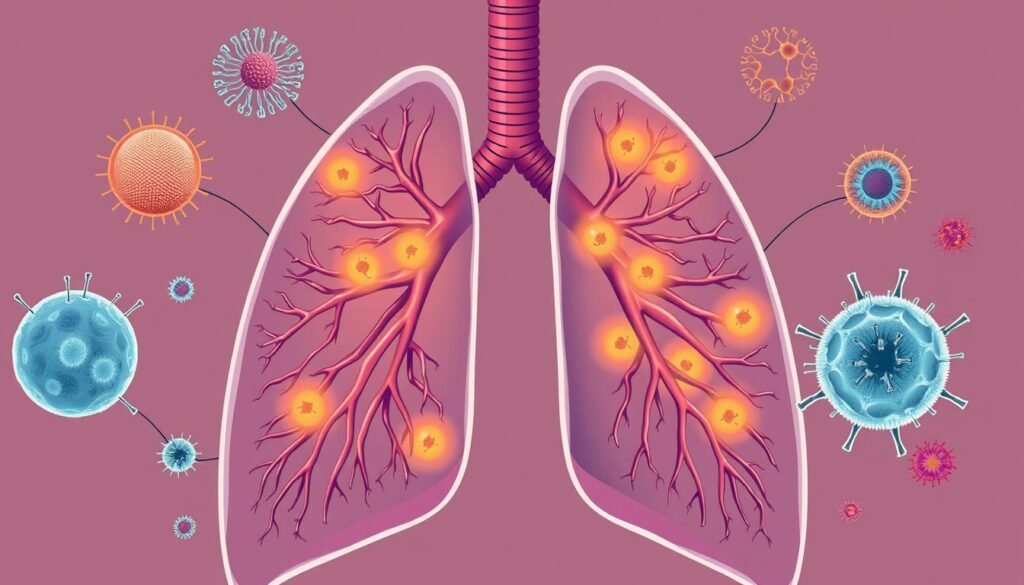
Lung nodules show up as small spots on tests like X-rays or CT scans. About half of adults see them during chest imaging for other reasons. Knowing about lung nodules is crucial for keeping lung health good and figuring out what to do next.
Most lung nodules are benign tumors. They can come from infections, scars, or lymph node swelling. Less than 5% are cancer. For example, 95% of nodules in people 50 to 75, especially those who smoke or used to, are not cancerous. This fact is why careful checks and follow-ups are vital.
Some factors, like how big a nodule is or how fast it grows, can hint at cancer risk. A larger, growing nodule is more likely to be harmful. But if a nodule doesn’t change for two years, it’s often harmless. The Fleischner Society has guidelines for handling nodules in patients over 35. These rules aid doctors in watching over and choosing treatment paths.
Doctors might use needle biopsies or video-assisted surgery (VATS) to learn more about a nodule. Catching and treating issues early is key, especially for those with a family history of lung cancer, smokers, and older adults.
The Temple Lung Center offers teams focused on lung nodule care. They give personalized, timely treatments as needed.
Staying informed about lung nodules is important for lung health. It encourages active involvement in one’s health care journey.
What Are Lung Nodules?
Lung nodules are small, round growths in the lungs. They are usually less than 3 centimeters across. Found during imaging studies like chest X-rays or CT scans, they often don’t cause symptoms. While many are harmless, some can indicate serious conditions, including cancer.
Their size and appearance can tell doctors a lot. For example, nodules under 6 millimeters usually have less than a 1 percent cancer risk. But, larger ones, especially over 10 millimeters, might show a 15 percent cancer risk. Details like spiculated borders and where they are in the lungs also matter. Plus, a person’s smoking history and age are important in assessing lung cancer risk. Keeping track with imaging studies helps monitor nodules and decide on treatments.
It’s important to understand pulmonary nodules. Knowing if a nodule is benign or serious affects treatment choices. This knowledge is key for those concerned about their lung health.
Factors that Increase the Risk of a Nodule Turning Cancerous
It’s really important to understand what makes a lung nodule likely to be cancerous. This helps doctors diagnose and treat effectively. They look at the size of the nodule and how fast it grows. They also check its appearance on scans.
Size and Growth Rate of Nodules
How big a nodule is can tell a lot about its cancer risk. Small nodules, less than 0.6 cm, are usually not cancerous. But if a nodule is larger than 1 cm, the risk increases to about 15%.
Growth speed is also key in judgement. Nodules growing more than 20% in a set time might be malignant. It’s crucial to keep an eye on them. If a nodule doesn’t change for two years, it’s likely not cancerous.
Nodule Characteristics on Imaging
Scans give detailed info about nodules. For example, nodules that look irregular or spiky are more concerning than smooth ones. CT scans are a big help here. They make it easier for doctors to spot risky changes over time.
| Nodule Size | Cancer Risk |
|---|---|
| Less than 0.6 cm | Less than 1% |
| 1 cm – 2 cm | Approximately 15% |
| Greater than 2 cm | About 40% to 50% |
In conclusion, knowing about the size, growth, and look of nodules helps doctors figure out the cancer risk. This knowledge is crucial for a good nodule management plan.
Lung Cancer Risk Factors
Lung cancer has certain risk factors that greatly affect someone’s chance of getting sick. Smoking and family history are very important to note. Knowing about these can help people watch out for the disease early on.
Smoking History
Smoking is the top cause of lung cancer, leading to about 80% of deaths from the illness. It’s especially linked to 90% of lung cancer cases. People who smoke cigarettes are at a big risk, especially for a type called small cell lung cancer.
Being around smoke, even if you don’t smoke, also poses risks. Secondhand smoke is the third leading cause of lung cancer in the U.S.
Family History of Lung Cancer
Having relatives with lung cancer increases your risk. If lung cancer runs in your family, your own risk might double. This could be due to genetics or the environment your family shares.
If you have two or more close relatives with lung cancer, your chance gets even higher. It’s critical that people in these families pay close attention to this risk.

Environmental Exposures
Environmental exposures significantly influence the risk of developing lung cancer. Carcinogens and radon gas are key factors not to be ignored. Understanding these can help in better prevention and strategy development.
Exposure to Carcinogens
Tobacco smoke is a major lung health threat. Asbestos and secondhand smoke also greatly increase lung cancer risks. Research shows long-term exposure to these substances makes lung cancer more likely. This highlights the need to tackle these dangers.
Radon Exposure
Radon is an invisible gas coming from natural uranium decay in soil. It’s a top lung cancer cause for non-smokers. This gas can build up inside homes, especially if they’re not well-ventilated. Knowing about radon is crucial, especially in high-radon areas, to protect your lungs and health.
The Role of Age and Gender in Lung Nodules
Age and gender are key in lung nodule risk and growth. Older adults often face a higher chance of having dangerous nodules. This is very important for doctors to consider when looking at lung nodules.
When we talk about gender, the picture gets more complex. It’s been found that men get lung cancer more often than women. This difference could be because of varying exposure to smoking and other harmful substances. Interestingly, women smokers may face a unique risk due to certain genetic changes, like the tp53 mutations. These changes can increase lung cancer risk.
In studies where lung nodules were removed for examination, more were found to be cancerous in women than in men. This shows that women could be more at risk in certain situations. It highlights how important gender is in understanding lung nodule risks.
Knowing about how age and gender affect lung nodules is vital. It helps in making personalized care plans. Such plans can guide doctors in how they treat and manage lung nodules, considering these personal factors.
| Demographic Factor | Impact on Lung Nodules |
|---|---|
| Age | Increased likelihood of malignant nodules |
| Gender (Male) | Higher incidences of lung cancer |
| Gender (Female) | More frequent harboring of tp53 mutations; increased risk from secondhand smoke |
Nodule Characteristics that Indicate Malignancy
Knowing about nodule characteristics is key in figuring out if a lung nodule might be cancerous. This looks at the nodule’s physical features. Features like spiculated borders and certain calcification patterns are major malignancy indicators.
Spiculated Borders and Calcification Patterns
Spiculated borders on lung nodules suggest a higher cancer risk. If a nodule’s edges look irregular or spiky, doctors get concerned. This usually leads to more tests like imaging or biopsy. Meanwhile, calcification in nodules gives clues about their nature. Nodules with harmless calcification patterns, like spread-out or central, are less likely to be cancer.
Recent research shows that small nodules, less than 6 mm, rarely are cancerous, nearly 0% to 1% risk. But if a nodule is larger than 10 mm, its cancer risk jumps to 15.2%. This info helps professionals decide how to best watch and recheck nodules. Proper management of lung nodules is crucial.
Underlying Lung Disease and Its Impact
Chronic lung diseases bring big challenges. They intertwine with cancer risk in several ways. Conditions like Chronic Obstructive Pulmonary Disease (COPD) reduce lung function. They may also increase the chance of getting lung cancer.
The link between these chronic conditions and the possibility of cancer is key. It helps us understand how to care for patients and assess their risks.
Chronic Conditions Contributing to Cancer Risk
Knowing how chronic lung disease ups cancer risk is important. It helps with finding ways to prevent and treat it. Inflammation and changes in lung tissue architecture are factors in this link.
- Chronic Obstructive Pulmonary Disease (COPD) harms lung function, leading to more lung nodules.
- People with COPD have a higher risk of lung cancer due to ongoing inflammation and lung tissue damage.
- In older people, lung disease ups the risk of cancer. This is especially true with a history of smoking or environmental exposures.
- Chronic conditions make screenings tough. This can make reading lung nodules harder.
Recent stats show the concern over lung nodules in chest X-rays. About 150,000 cases are found each year in the U.S. Patients with chronic lung diseases are included in this number. It shows how chronic conditions and cancer risk are closely linked.
| Chronic Condition | Impact on Lung Cancer Risk |
|---|---|
| COPD | Increased risk due to lung damage and inflammation |
| Pulmonary Fibrosis | Scarring of lungs may lead to higher malignancy potential |
| Asthma | Chronic inflammation may correlate with increased cancer risk |
| Chronic Bronchitis | Persistent inflammation can contribute to malignancy risk |
Genetic Mutations and Risk Assessment
It’s key to understand how genetic mutations affect lung cancer risk. Some mutations make people more likely to get lung cancer. This shows the role of genes in lung nodules.
Doctors can use genetic tests to check lung nodule risks. This helps find out who might be at higher risk of cancer. By knowing this, doctors can watch and treat these patients carefully.
New technologies like the ThyroSeq genomic classifier are important. They can tell if nodules are benign or cancerous. The test found 94% of cancerous nodules before surgery and has a low rate of missing cancer.
- Pathologists often can’t tell if a third of thyroid nodules are cancer.
- The ThyroSeq test said 61% of nodules were benign, and 39% were cancerous in 257 nodules.
- Many nodules seemed benign in traditional pathology reports.
- Genetic tests look for changes in 112 genes tied to thyroid cancer, which helps in risk assessment.
Genetic mutations are key for diagnosing lung cancer. Doctors use them, along with environmental info, to plan prevention and treatment. This leads to better care for lung cancer patients.
| Type of Finding | ThyroSeq Result | Traditional Pathology Result |
|---|---|---|
| Benign | 61% | 72% |
| Cancerous | 39% | 24% |
| Borderline Malignancy | N/A | 4% |
| Accuracy Identifying Cancerous Nodules | 94% | N/A |
| False-Negative Rate | 3% | N/A |
Conclusion
Understanding lung nodules and their risk of becoming cancerous is very important. The size, growth speed, and what they look like on scans matter. Knowing these helps doctors find people who might be at higher risk. They can then watch these patients more closely.
Being aware of what in the environment could make lung health worse is key to preventing cancer. People need to keep an eye on their lung health. They should talk to doctors about any worries. Making good choices for your health and getting regular checks can lower the risks from lung nodules.
Watching lung nodules closely, making smart health decisions, and being proactive are important. If you stay informed and get advice that fits you, you can work towards a healthier future. This can help find and treat problems early.