Did you know that more than half the people worldwide could have thyroid nodules? Yet, we find only a few during regular check-ups. This fact highlights why knowing the key factors in thyroid nodule risk assessment is vital. Checking these nodules is key not just to figure out thyroid cancer risk but to decide how to manage the nodules. With more ultrasound use, we’re finding more nodules. So, understanding the risk factors is key to caring for patients well.
Evaluating thyroid nodules means looking at several things: clinical risk factors, how the nodules appear on ultrasounds, and lab tests. All these parts help figure out the cancer risk better, so doctors can plan the best care. Knowing how to predict risks can mean getting help early and better chances for those with thyroid nodules. You can learn more about these methods in studies here.
Key Takeaways
- Thyroid nodules are common, and we’re finding more thanks to better imaging tech.
- It’s crucial to know the risk factors to make good predictions.
- Clinical looks and ultrasound views are really important for assessing thyroid cancer risks.
- Tests in the lab help make the risk picture clearer and guide how to manage nodules.
- Assessing risks well means making smarter choices in treating thyroid nodules.
Introduction to Thyroid Nodules
Thyroid nodules are unusual lumps in the thyroid gland, which is shaped like a butterfly and located at the front of your neck. These lumps can be big or small. They might be felt or not felt at all. An overview of thyroid nodules shows they’re common, affecting nearly 68% of people when checked by ultrasound. Most of the time, these lumps don’t cause any symptoms. They’re found by accident during tests for other health issues.
It’s key to focus on thyroid health. Knowing about thyroid nodules helps us deal with different thyroid problems. While most nodules are harmless—90% to 95% of them—some can be cancerous. The chance of cancer in inactive lumps ranges from 14% to 22%, based on their look and other test results. For instance, Bethesda category 5 nodules have a 60% to 75% chance of being cancerous.
Also, research shows that women are more likely to have thyroid nodules than men, by a factor of four. It’s important for anyone with nodules to be watched over time. This is because up to half of all people might have them without knowing. Many of these cases need more tests. This ensures they are handled right, depending on how likely they are to be a problem.
| Statistic | Findings |
|---|---|
| Prevalence in Adults | 5-7% (Physical exams) / 20-76% (Ultrasound) |
| Male vs Female Prevalence | 0.8% in men / 5.3% in women |
| Risk of Malignancy | 14-22% for nonfunctioning nodules / 60-75% for suspicious nodules |
| Benign Nodules | 90-95% of all thyroid nodules |
| Incidence of Thyroid Cancer | 8% in men / 4% in women |
Prevalence and Detection of Thyroid Nodules
The prevalence of thyroid nodules is a big topic in medicine today. Recent studies show concerning numbers. For instance, out of 45,023 healthy adults, about 29.8% had thyroid nodules detected, summing up to 13,437 cases. This points out how crucial early thyroid nodule detection is for health.
Who gets thyroid nodules varies with age and gender. People over 30 and women are more at risk. Also, being overweight, having high blood sugar, and obesity raise the chance of getting nodules. Each of these factors makes nodules more likely.
A study in Korea checked 72,319 people for thyroid issues with an ultrasound. They found 34.2% had nodules or cysts. Many of the nodules discovered were 1 cm or smaller. This shows why we need good detection methods.
As more people get regular health check-ups, we find more thyroid nodules. Knowing about prevalence of thyroid nodules helps us stay aware. It makes us go for check-ups often.
Factors Considered in Nodule Risk Calculations
Healthcare providers use several factors to calculate nodule risk. This helps them figure out if thyroid nodules might be cancerous. They look at clinical risk factors, ultrasound details, and lab tests. These things help with accurate diagnosis and treatment.
Clinical Risk Factors
There are key clinical risk factors that matter a lot. They are:
- A hard consistency of the nodule
- Rapid growth of the nodule
- Local symptoms like hoarseness or dysphagia
- Cervical lymphadenopathy
- A history of thyroid cancer
These factors raise concern about cancer. Having several of these signs increases worry.
Ultrasound Characteristics
Ultrasound tells us a lot about nodules. Signs that suggest a higher cancer risk include:
- Solid composition
- Irregular margins
- Microcalcifications
- Taller-than-wide shape
- Marked hypoechogenicity
Doctors use ultrasound details to decide on further tests like a biopsy.
Laboratory Tests and Biomarkers
Labs tests also give important clues. A key test is the serum TSH level:
- A low TSH often means the nodule is benign
- A high TSH suggests more tests might be needed, like a thyroid scan
Cancer biomarker tests add to this knowledge. They play a big role in spotting cancers and planning treatment.
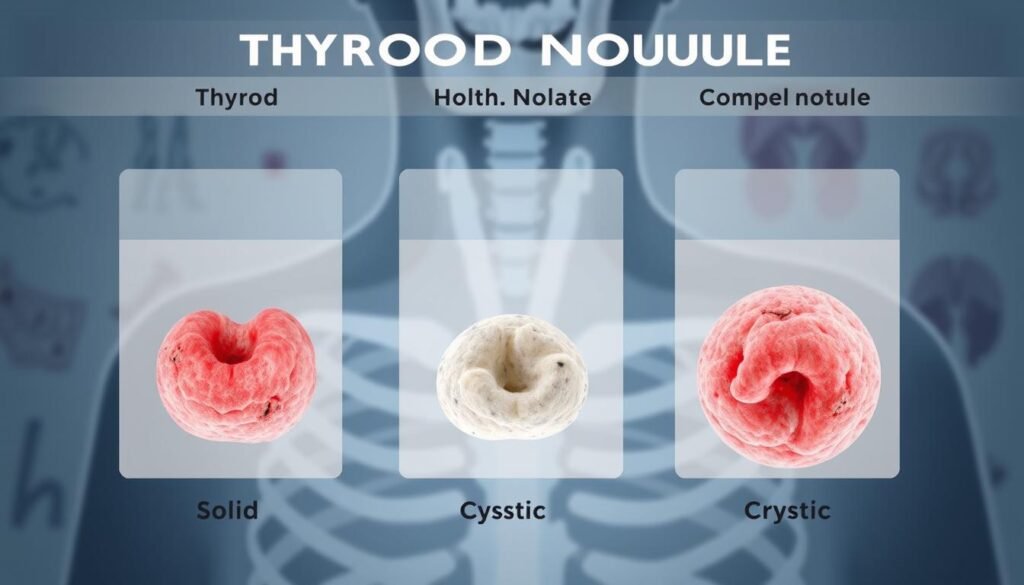
Nodule Types and Their Implications
There are different types of thyroid nodules, each with its own features. Some common types are colloid nodules, cysts, and follicular adenomas. The serious ones include thyroid cancers like papillary and follicular. Knowing these types helps doctors decide on treatment plans.
About 90-95% of thyroid nodules are not cancerous. It’s vital to tell benign nodules apart from malignant ones. Solid nodules are often more concerning than cystic ones. This is why proper tests, like imaging and needle aspirations, are key.
Choosing the right treatment for thyroid nodules requires knowing their traits. A full evaluation aids patients and doctors in making informed choices. This leads to better care for each person’s needs.
| Type of Nodule | Risk of Malignancy | Common Characteristics |
|---|---|---|
| Colloid Nodules | Low | Fluid-filled, often benign |
| Cysts | Very Low | Fluid-filled sac, rarely cancerous |
| Follicular Adenomas | Low to Moderate | Solid, well-circumscribed, benign growths |
| Papillary Thyroid Cancer | Moderate to High | Most common type of thyroid cancer, slow-growing |
| Follicular Thyroid Cancer | Moderate to High | Coarsely lobulated, can metastasize |
Nodule Size and Its Impact on Risk
Nodule size and risk are key in assessing thyroid nodules. Generally, bigger nodules have a higher cancer risk. Nodule size matters when we look at specific sizes: studies show that cancer risks go up for nodules larger than 0.5 cm for papillary thyroid cancer and bigger than 2 cm for follicular thyroid cancer. Knowing about nodule size helps in managing thyroid nodules well.
Doctors should use more than nodule size in their evaluations. They need to look at ultrasound results and other clinical info too. This helps them better judge the cancer risk. Even small nodules can sometimes be cancerous, studies say.
It’s crucial for healthcare pros to keep up with the latest in treatment and management. They should use a well-rounded approach to decide on biopsies and patient check-ups. For further details, one can look into a study that dives deeper into this subject.
Patient Age as a Risk Factor
It’s vital to know how patient age affects thyroid cancer risk. Studies show a big difference in risk based on age. This affects how nodules are looked at and handled. People over 60 more often have cancerous nodules, unlike those under 20.

A study with 6,391 patients found a big difference in cancer rates. Younger people had a higher incidence of 22.9%, compared to 12.6% in older individuals. This shows why thyroid nodule assessment by age is important. Older patients might have more dangerous types of thyroid cancer.
The number of nodules people have goes up as they get older. From ages 20-30, the average is 1.5 nodules. But for those over 70, it jumps to 2.2. With age, the chance of having more than one nodule increases by 1.6% each year. However, the risk of these nodules being cancerous drops slightly until age 60, then it levels off.
The following table shows how age ties to the risk of thyroid nodule cancer:
| Age Group | Cancer Incidence (%) | Average Nodules per Patient | Risk of Multinodularity (% increase/year) |
|---|---|---|---|
| 20-29 | 22.9 | 1.5 | 1.6 |
| 30-39 | Initial data shows a decreasing trend | Increases gradually | 1.6 |
| 40-49 | Further decrease observed | Progressively increases | 1.6 |
| 50-59 | Reduction continues | Increasing number | 1.6 |
| 60-69 | Stabilizes at lower levels | Further steady increase | 1.6 |
| 70+ | 12.6 | 2.2 | 1.6 |
Age greatly impacts how healthcare providers assess thyroid nodules. Different age groups have different risk profiles. This helps in choosing the right tests and treatments, leading to better care for patients.
Role of Family History in Thyroid Cancer Risk
If you have a family history of thyroid cancer, it’s important for checking thyroid nodules. Studies show that if your close family members had thyroid cancer, your own risk goes up. The risk increase is quite high, with an odds ratio (OR) of 4.1, pointing out how genetics play a role in cancer risk.
Those with thyroid cancer in their immediate family especially face a higher chance of getting papillary thyroid carcinoma (PTC). Their risk jumps, with an odds ratio of 4.6 for PTC. If a sibling has it, the risk is even higher, with an OR of 7.4. This suggests people with family history need careful monitoring.
Having a family member with thyroid cancer means a higher chance of developing multifocal primary tumors. In fact, 68.8% of PTC patients with a family history have multiple tumors, unlike 35.5% of those without. This highlights the need for thorough screening for those with genetic links to thyroid cancer. Conditions like Multiple Endocrine Neoplasia type 2 (MEN2) also elevate the risk.
Though thyroid cancer diagnoses have increased due to better tests, family history still plays a crucial role in thyroid nodule assessment. Recognizing genetic risks is key in how we manage and care for patients.
Smoking History and Thyroid Nodule Risk
Studies show a tricky link between smoking and thyroid health. This includes how likely it is for smokers to get thyroid nodules and cancer. Though current smokers seem to have a lower chance of getting thyroid cancer, with a hazard ratio of 0.68, this does not fit the normal patterns seen in other cancers.
Smoking might offer some protection against thyroid cancer, but it changes with lifestyle choices like drinking. Non-drinkers who smoke show a much lower hazard ratio of 0.46. This points out how our life choices mix together to affect our thyroid health. Surprisingly, smokers, both current and former, often face lower odds of getting thyroid nodules than non-smokers. This makes us question the usual bad rap smoking gets concerning thyroid issues.
Generally, more women get thyroid nodules than men. The link between how much and how long people have smoked and a lower risk is clear. But, this protective effect doesn’t apply to former smokers in the same way.
As we learn more about how smoking affects the thyroid, future studies are key. Grasping how smoking impacts the thyroid will help create better ways to prevent and treat thyroid diseases.
| Category | Current Smokers | Former Smokers | Never Smokers |
|---|---|---|---|
| Odds of Thyroid Nodules | Reduced Risk | No Significant Change | Higher Risk |
| Hazard Ratio for Thyroid Cancer | 0.68 | N/A | Reference |
| Association with Alcohol | Stronger Protection | Varying Effects | Standard Risk |
| Gender Prevalence | Lower for Males | Lower for Males | Higher in Females |
Current Risk Prediction Models for Thyroid Nodules
New ways to predict thyroid nodule cancer risk are making a big difference. Doctors now consider a mix of clinical signs, ultrasound features, and test results. These tools help them figure out how likely a nodule is to be cancerous.
One study looked at 4,176 patients and 5,730 nodules bigger than 1 cm. Eighty-three percent of these patients were women, averaging 51 years old. This information helps explain cancer risk. Among these nodules, 20% that looked mostly solid were actually cancer.
Current guidelines use specific measures, like the nodule’s shape, to gauge cancer risk. For example, if a nodule’s long-to-short side ratio is close to 1, cancer risk goes up. Nodules with a ratio over 2 showed cancer in 14.6% of cases. Those with a ratio between 1 and 1.5 showed a 25.5% cancer rate.
Blood tests for thyroid function and antibodies also play a big part. They make it easier to decide on the right approach for each patient. This tailored assessment improves care and avoids unnecessary procedures.
Research keeps making these models better, offering hope for more personalized treatment plans. For more details on this topic, check out the study findings.
| Long to Short Ratio | Cancer Risk Percentage |
|---|---|
| Ratio > 2.00 | 14.6% |
| Ratio 1.51-2.00 | 19.7% |
| Ratio 1.00-1.50 | 25.5% |
Lung Nodule Management Techniques
Managing lung nodules is key for catching and treating possible lung cancer early. There are now many techniques that help doctors make smart choices. These techniques include screening guidelines that help check and follow up on patients, which is critical for timely treatment.
Research shows that 33% of people in screenings have noncalcified lung nodules. In studies without screenings, it’s only 13%. This shows why regular screenings are crucial for finding nodules early. Nodules smaller than 5 mm are usually not cancerous, so it’s important to manage them based on their size and other risks.
Following set guidelines is a big part of managing lung nodules. For example, the British Thoracic Society suggests a follow-up for nodules at 5 mm. The Fleischner Society suggests waiting until they reach 6 mm. Guidelines like these help decide if a patient needs more tests or treatments.
Management methods include:
- Watching nodules with regular images.
- Classifying nodules by size and volume.
- Biopsy for nodules that seem risky or grow fast.
It’s crucial to know how the size of a nodule can mean a higher cancer risk. Small nodules have a low risk, but nodules larger than 10 mm can often be cancerous. So, understanding size can guide what actions to take.
The Volume Doubling Time (VDT) can tell us about the nodule’s risk. A VDT under 400 days might mean cancer is more likely, leading to more tests. Those with many nodules or who have smoked before are at increased risk, highlighting the need for careful management.
CT scans are very important for small solid nodules, especially if they’re big enough to keep an eye on. For part-solid nodules, using specific types of CT scans can catch any growth early on.
| Nodule Size (mm) | Malignancy Prevalence (%) | Recommended Follow-Up |
|---|---|---|
| <5 | 0.4 | No follow-up |
| 5-10 | 1.3 | CT surveillance |
| >10 | 15.2 | Consider biopsy |
As we learn more about how to manage lung nodules, using proven guidelines and methods will improve patient outcomes. Understanding how nodule size and cancer risk are related helps us take early action for better lung health.

Conclusion
When it comes to thyroid nodule risk, a full understanding is key. Studies show we must look at many factors. These include clinical features, imaging results, and more.
This comprehensive look helps in figuring out the chance of cancer in thyroid nodules. Experts suggest using volumetric assessments for nodules that grow or change fast. Setting clear follow-up rules means fewer unneeded tests.
For nodules that are not solid, less aggressive care works well. This is because they often have a better outlook. Keeping up with new findings and talking about risks improves patient care. This way, everyone gets a treatment plan that fits their needs.