Every 2.3 minutes, someone in the U.S. finds out they have lung cancer. That’s about 230,000 new cases every year. This shows how urgent it is to deal with lung cancer and how it differs across areas. Lung cancer is the top reason people die from cancer in the U.S. It affects 1 in 16 people at some point in their lives. The latest lung cancer statistics for 2024 show that some states, like Kentucky, have much higher rates. Knowing how common lung cancer is in each state is the first step to tackling it. It helps us understand who is most affected and why.
This article looks at states with the most lung cancer cases, especially Kentucky, Louisiana, and Arkansas. These states are trying hard to fight this health crisis. Seeing the numbers helps us realize that we need to battle lung cancer in specific places to make a difference.
Key Takeaways
- Kentucky leads the U.S. with the highest lung cancer rates at 503.4 new cases per 100,000 residents.
- The Southeast, especially the Appalachian region, exhibits the most significant lung cancer prevalence.
- Socioeconomic status significantly influences access to healthcare and cancer screenings.
- Smoking remains a primary risk factor, contributing to increased lung cancer diagnoses.
- Lung cancer accounts for 21% of all cancer deaths in 2022, highlighting its mortality impact.
- Understanding demographic disparities is vital for developing targeted intervention strategies.
- Ongoing research and data analysis are essential for tracking trends in lung cancer rates.
Understanding Lung Cancer Statistics
Lung cancer is the top cause of cancer deaths in the U.S., with a shocking 20.4% of all cancer deaths. Around 234,580 new cases are expected in 2024. This is 11.7% of all cancer cases. These lung cancer statistics show how big a problem it is for public health.
The rate of lung cancer deaths varies a lot by state. For example, Kentucky’s rate is very high at 53.5 per 100,000 people. In contrast, Utah’s rate is much lower, at 16.4. Out of all states, twenty-one have death rates above the national average of 34.8 per 100,000 people.
Looking at diagnosis rates helps us understand how to fight lung cancer. These numbers help health officials know where to focus their efforts. The five-year survival rate for localized lung cancer is about 63.7%. This shows why finding cancer early is so important.
The Importance of State-Specific Data
Understanding state-specific lung cancer data is vital. It shows how lung cancer rates vary from one state to another. This is because of differences in health policies, living standards, healthcare access, and the environment. Such specifics help public health experts design actions that meet the local community’s needs.
In places like Kentucky, lung cancer rates are high. This calls for unique health initiatives there. On the other hand, states with better healthcare systems see higher survival rates. This link between detailed cancer research data and health results shows why local data is crucial.
Areas with fewer uninsured people tend to have better lung cancer survival rates. Knowing state data well lets health officials pinpoint where to focus their efforts. This way, they can better distribute resources, helping detect and treat cancer earlier in communities that need it the most.
| State | Lung Cancer Incidence Rate (per 100,000) | 5-Year Survival Rate (CSV) |
|---|---|---|
| Kentucky | 93.5 | 38.6% |
| Connecticut | – | 38.6% |
| Colorado | 43.4 | 30.2% |
| Pennsylvania | 64.0 | – |
Top States with Highest Lung Cancer Rates
An analysis shows some U.S. states have high lung cancer rates. Kentucky is at the top, followed by Louisiana and Arkansas. This shows a need for health efforts.
Kentucky: The State with the Highest Rates
Kentucky leads in lung cancer rates with 82.8 cases per 100,000 people. The high rate of smoking is a big problem here. Efforts to cut down smoking are crucial.
Louisiana and Arkansas: Close Contenders
Next is Louisiana, with lung cancer rates at 78.5 per 100,000. This situation calls for preventive steps and better healthcare. Arkansas also faces these problems, with rates at 76.2 per 100,000, showing a regional issue.
Contributing Factors to Lung Cancer Rates
The landscape of lung cancer rates in the United States involves many factors. Knowing these factors helps with coming up with prevention strategies. Smoking is the biggest risk factor for lung cancer. But other environmental and job-related exposures also matter a lot.
Smoking Rates and Lung Cancer Correlation
Cigarette smoking leads to most lung cancer deaths, about 80% to 90%. Smokers have a 15 to 30 times higher risk of getting lung cancer than non-smokers. The more and longer people smoke, the higher their risk.
However, those who quit smoking do reduce their risk. But they still have a higher chance of getting lung cancer than those who’ve never smoked.
Impact of Air Pollution
Air pollution significantly affects lung cancer rates. If you live in a high pollution area, your risk goes up. This is because of carcinogens in the air.
Pollutants like particulate matter and toxic gases harm cells. This shows the strong link between air pollution and lung cancer. So, reducing emissions is key to lowering risks.
Occupational Exposure Risks
Some jobs expose workers to substances that increase lung cancer risk. Being around asbestos, diesel exhaust, and chemicals like arsenic and silica is dangerous. Those in high-risk jobs face more exposure over time. This highlights the need for strict safety rules at work.
Understanding job-related risks helps focus on reducing lung cancer in those most at risk.

Demographic Factors Influencing Lung Cancer Prevalence
Demographic aspects are key to grasping lung cancer spread in varying groups. Both genetic factors and socioeconomic status and cancer deeply impact its incidence and outcomes. Some groups face augmented risks from these elements.
Genetic Factors and Family History
Certain genetic factors heighten the risk of lung cancer. Having family members with the disease increases your risk notably, especially for close kin. A genetic link means those with family histories need vigilant screening and awareness.
Socioeconomic Status and Access to Healthcare
Socioeconomic status and cancer outcomes are tightly connected. Those with lower incomes struggle to get high-quality healthcare. This often leads to late cancer diagnoses. Late detection means worse survival chances. Studies link higher lung cancer rates with poverty, due to fewer chances for early care and screenings.
Analysis of Lung Cancer Screening Rates
Lung cancer screening is key to better patient results. It aims to lift screening rates nationwide. Yet, certain areas show big gaps in how often people get screened. This can affect chances to catch lung cancer early. Early spotting is key for successful treatment and higher survival chances.
States with Lowest Screening Rates
Some states’ screening stats are worrying. For instance, Kentucky’s rates are very low, even though it has the most lung cancer cases. The use of low-dose computed tomography (LDCT) varies a lot in the US. These differences help target public health efforts to lessen lung cancer caught at late stages.
Impact of Early Detection on Survival Rates
Spotting lung cancer early can greatly boost survival odds. New Mexico saw a 28% rise in early findings due to more LDCT screening. This shows why all states need to up their screening game. Efforts might include easier access to screening sites and local info campaigns, especially where early detection is still rare.
New screening and diagnostic tech open doors for early treatment of lung cancer. Getting more people into screening can vastly better health results. This brings hope of healthier futures for many.
For deeper insight into lung cancer screening rates, check out the CDC’s in-depth research here.
Comparative Lung Cancer Mortality Rates by State
Lung cancer is a major public health issue in the United States. In 2021, it caused 22% of all cancer deaths, taking 134,592 lives. Different states show big differences in death rates.
In 2019, Mississippi had the highest lung cancer death rate, 178.8 per 100,000 people. Kentucky and West Virginia had rates of 176.1 and 173.7, respectively. This shows that some states need more help to fight lung cancer.
On the other hand, Utah had the lowest rate, only 117.8 per 100,000. Colorado and Hawaii had rates of 126.0 and 126.7. This shows the big differences in lung cancer rates across the country. It points out the need for local plans to fight this disease.
The table below shows lung cancer death rates in selected states. It gives a clearer picture of how different states compare:
| State | Lung Cancer Mortality Rate (per 100,000) |
|---|---|
| Mississippi | 178.8 |
| Kentucky | 176.1 |
| West Virginia | 173.7 |
| Louisiana | 169.8 |
| Arkansas | 165.4 |
| Utah | 117.8 |
| Colorado | 126.0 |
| Hawaii | 126.7 |
These numbers reveal important facts about lung cancer deaths. They show that some states have bigger challenges than others. We need to work together on prevention, education, and healthcare access to tackle these differences.
Lung Cancer Prevalence by State: A Comprehensive Overview
It’s crucial to know how common lung cancer is in different states. This tells us about public health in the U.S. Some places have more lung cancer cases, which shows we need specific plans to help those areas.
From 2007 to 2016, lung cancer was less common in big cities than in rural areas. Particularly, in 2007, rural men had lung cancer 60% more than women. By 2016, this gap got smaller, but it was still 40% higher in men.
In big cities, both men and women saw a faster drop in lung cancer rates. The biggest decrease for men was in cities, especially those aged 45–54. For younger people in rural areas, aged 35–44, there was a significant decrease. Women in cities also saw drops in most age groups, except those under 35.
Older men, 55 and up, in rural areas had the highest lung cancer rates. This shows age and where you live play big roles in lung cancer rates. Yet, in younger people, from 35-54, the gap between men and women is smaller. This hints at the influence of smoking, location, and healthcare access.
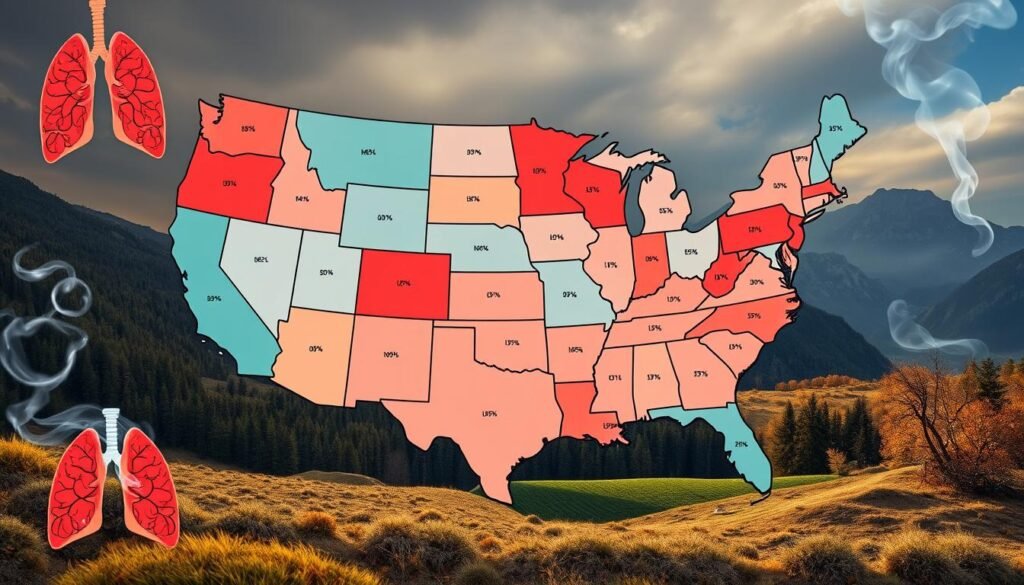
Recent data shows people in rural areas smoke more and quit less. This smoking trend, and different lung cancer rates, means we need a better approach in public health messages and services for these communities.
Taking a close look at lung cancer by state helps us find trends. These trends guide the health policies and efforts to lower lung cancer countrywide.
Addressing Radon Levels in Homes
Radon exposure greatly increases lung cancer risk, making it a critical health issue in the US. This harmful gas can build up inside, especially where air doesn’t move much. Knowing and managing radon levels in homes is key to lowering health risks. Testing homes for radon is the first important step to find out if action is needed.
Health Risks and Safety Measures
About 21,000 people die from lung cancer linked to radon in their homes every year in the US, according to the Environmental Protection Agency. The Consumer’s Guide to Radon Reduction says the risk goes up the more you’re exposed, especially for smokers. Even a radon level of 10 pCi/L can greatly increase lung cancer risks, showing why prevention is crucial for all homes.
More people now understand that radon is a big risk for lung cancer. A study found that 42% of cancer plans mentioned radon activities. These strategies aim to get more homes tested for radon, as reported by 32% of these plans. About 16.9% of the plans talked about fixing homes with high radon levels.
Yet, the number of homes being tested for radon is still low. Focusing on groups at higher risk, such as heavy smokers, could make radon prevention more effective and affordable. The cost to prevent one lung cancer death using radon tests and fixes is about $3 million. This shows both the challenges and opportunities for health projects.
| Radon Level (pCi/L) | Risk for Never-Smokers | Risk for Ever-Smokers |
|---|---|---|
| 0 | 1 in 1,000 | 1 in 3 |
| 2 | 1 in 1,000 | 1 in 7 |
| 4 | 2 in 1,000 | 1 in 3 |
| 10 | 18 in 1,000 | 150 in 1,000 |
Doing radon tests regularly and using good reduction systems can seriously cut radon levels and health risks in homes. By understanding how critical these steps are, communities can better shield people from radon’s dangers.
Conclusion
The article shows that lung cancer rates are not the same in every state. Kentucky has the highest rates, almost 2.4 times more than Utah, which has the lowest. This information is crucial. It tells us how common lung cancer is and how long people live after getting it. It shows why we need to work harder to make people aware of lung cancer.
In the last five years, new lung cancer cases have gone down by 8%. This shows that public health efforts might be working. But, only 26.6% of lung cancer cases are found early. Sadly, not enough people are getting screened. This tells us we need better access to screening and to teach patients more about it. Also, not everyone gets the treatment they need. This situation offers a chance for health leaders and lawmakers to work together. They can make more screening and treatment options available.
Lung cancer doesn’t come from just one thing. It can be due to smoking or being around harmful stuff in the environment. We need to keep researching and finding specific ways to fight lung cancer. Public health campaigns must focus on lowering lung cancer rates everywhere in the country. By acting early and preventing lung cancer, we aim for better health results. We also want to improve life for those who might get lung cancer.