Lung cancer leads in deaths more than breast, prostate, and colorectal cancers combined. In 2020, around 228,820 people in the U.S. were diagnosed with this disease, resulting in 135,720 deaths. This fact shows how vital early detection is for improving survival rates in people at risk. The ct lung cancer screening guidelines now primarily use *low-dose CT scans* to find lung cancer early, especially in high-risk people.
The newest guidelines have widened who can get screened, now including those 50 to 80 years old with a *20 pack-year smoking history*. This change means close to 5 million more people are eligible for screening each year. Plus, studies show talking well and making decisions together with doctors is key in lung cancer screening.
Key Takeaways
- Lung cancer is the leading cause of cancer deaths in the U.S.
- The updated guidelines broaden screening eligibility significantly.
- Low-dose CT scans are essential for effective lung cancer early detection.
- Shared decision-making enhances participation in screening.
- Criteria now focus on both current and former smokers with 20+ pack-year histories.
Introduction to Lung Cancer Screening
Lung cancer is the top cause of cancer death in the U.S. Finding it early is key to fighting it. Low-dose CT (LDCT) scans are now the best way to spot it early. They are much better than old screening methods.
The ct lung cancer screening guidelines lay out who should get screened. These rules are based on age and how much someone has smoked. The guidelines help find those who would benefit the most from screening. This is usually older adults, especially those who smoke or used to smoke a lot.
Studies prove LDCT scans lower the chance of dying from lung cancer in heavy smokers. The National Lung Screening Trial found big benefits for smokers aged 55 to 74. They smoked a pack a day for 30 years. Getting screened every year for three years helped a lot.
LDCT screenings for lung cancer have clear benefits. But, there are some negatives, like false positives. These can lead to tests you don’t need. This is why sticking to the screening rules is important. It makes sure the right people get screened. This helps find and treat lung cancer early.
Importance of Early Detection
Finding lung cancer early improves chances of successful treatment. Studies show that the sooner lung cancer is found, the better the survival rates. For example, if caught early, the 5-year survival rate is about 56%. However, this drops to 5% when it’s advanced. Starting routine screenings can catch it early, when it’s most treatable.
The benefits of screening with low-dose computed tomography (LDCT) are major. The American Cancer Society suggests yearly screenings for those 50 to 80 who have smoked the equivalent of 20 packs a year. Screening early can find lung cancer before any symptoms show. This is crucial because many don’t have noticeable symptoms until it’s late.
Regular screenings mean earlier treatment, which is usually less intense and leads to better outcomes. Yearly LDCT scans are key to saving lives, especially in people at high risk. It’s vital for people to know how important it is to find the disease early and understand their risks.
Talking about lung cancer screenings in regular health checks helps people make informed decisions about their health. Early detection is key in battling lung cancer. It shows why screenings are critical for those at higher risk.
CT Lung Cancer Screening Guidelines
It’s very important to know the ct lung cancer screening guidelines. These guidelines help find people who could benefit from early detection. The rules are designed to make early lung cancer treatment as effective as possible. They recommend regular screenings for people at high risk to raise the chances of survival.
Eligibility Criteria for Screening
These guidelines focus on adults aged 50 to 80 years with a heavy smoking history. To qualify for yearly screening, one needs a 20 pack-year history of smoking. This means smoking a pack a day for 20 years or something similar. It’s vital to look at each person’s smoking habits and when they quit during the screening process.
Age and Smoking History
Age is key when deciding who should get lung cancer screenings. The rules say to start screening at 50 and stop at 80, if the smoking criteria are met. People who haven’t smoked in 15 years should stop getting screened. This ensures the focus is on those with the highest risk.
Annual Screening Recommendations
Yearly screenings are advised to use low-dose computed tomography (LDCT). This method is effective for finding lung cancer early in at-risk folks. The ct lung cancer screening guidelines highlight this approach to catch lung cancer early, making treatment more effective. It’s also smart to pair screening with efforts to quit smoking to promote better health.

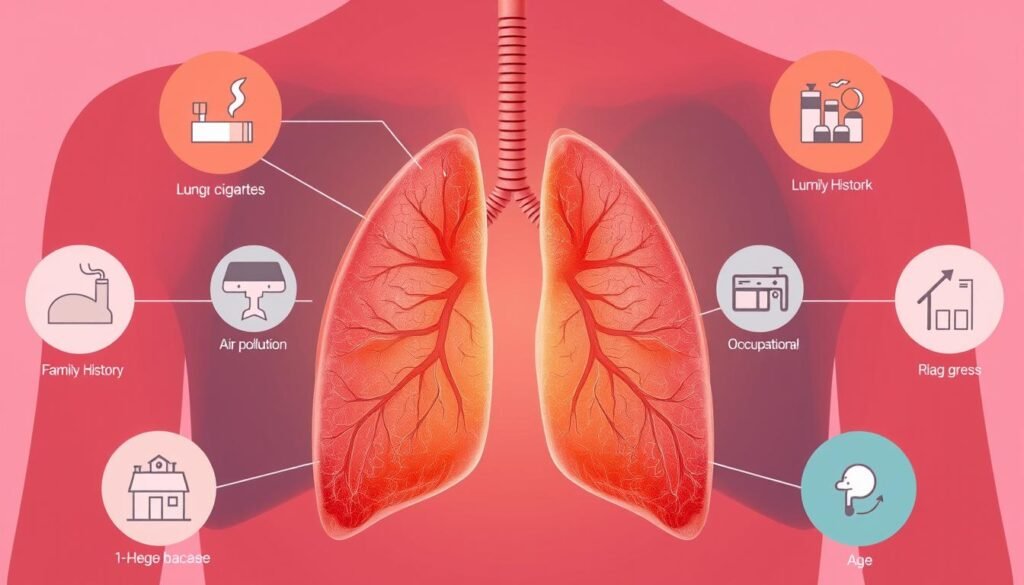
Understanding Lung Cancer Risk Factors
Many risk factors for lung cancer exist, but smoking is the top one. Knowing these factors is key for doctors to find who needs screening.
Smoking and Cumulative Exposure
Smoking causes about 90% of lung cancers. The smoking history guidelines show that long-term smokers are at a higher risk. They define risk in terms of pack-years – one pack a day for a year.
If you’re 55 to 74 years old and have smoked a lot for 30 years, your lung cancer risk is high. Smokers are 20 times more likely to get lung cancer than non-smokers. This shows how important it is to screen people who have smoked a lot.
Other Risk Factors for Lung Cancer
Other things besides smoking can also raise your lung cancer risk. Being around radon, asbestos, and certain chemicals is dangerous. So is having certain diseases like COPD.
Genetics matter too. If lung cancer runs in your family, you might be more likely to get it. Doctors need to consider all these risks to decide who needs lung cancer screening.
Low-Dose CT Scans: The Screening Method
In recent years, the low-dose CT scan has become key for lung cancer screening. It spots abnormalities well but uses less radiation than normal CT scans. This makes it safer for regular checks.
Benefits of Low-Dose CT Scans
The benefits of low-dose CT scans are huge. They catch lung cancer early, which helps people live longer. New guidelines could let more people get screened.
This includes groups at higher risk. Finding cancer early can change lives. It means better chances and outcomes for patients.
Limitations and Considerations
But, this method isn’t perfect. Sometimes, it shows cancer when there isn’t any. This can cause stress and lead to more tests. Patients should know these risks.
Understanding their choices helps. Knowing more about the process improves the experience. For more on effective lung cancer screening, doctors should check the latest advice.
| Feature | Standard CT Scan | Low-Dose CT Scan |
|---|---|---|
| Radiation Exposure | Higher | Lower |
| Sensitivity for Lung Cancer | Standard | High |
| Use in Screening | Limited | Widely Recommended |
| False Positive Rate | Lower | Higher |
| Accessibility | Restricted | Improved |
We must weigh the pros against the cons of low-dose CT scans. The balance between benefits and challenges is crucial. Research and new criteria will keep improving lung cancer detection.
Shared Decision-Making in Screening
Shared decision-making is key in discussing lung cancer screening. This teamwork between healthcare providers and patients talks about the screenings’ pros and cons. They consider things like overdiagnosis, false positive rates, and radiation exposure. This approach helps patients make informed decisions, building trust and satisfaction.
Eligibility for lung cancer screening is specific. You need to be aged 55 to 77. Current smokers have to have a 30-pack year smoking history. Former smokers must note how long it’s been since they quit. This helps make sure recommendations fit each person’s health and personal history.
In shared decision-making visits, healthcare providers walk through the procedure. They also cover how to handle other health issues and stress the need for yearly low-dose CT screenings. Talks on quitting smoking for current smokers and keeping former smokers from starting again are crucial.
Discussing how to quit tobacco is part of the conversation. It aims to get patients involved and underline the discussions’ thoroughness.
| Aspect | Details |
|---|---|
| Age Range | 55-77 years |
| Current Smokers | 30-pack years minimum |
| Former Smokers | Time since quitting documented |
| Counseling Focus | Benefits, harms, smoking cessation |
| Adherence Rate | 55% in studies after baseline screening |
Shared decision-making does more than check eligibility; it matches lung cancer screening with patient health goals. Reaching out to those at risk can be hard because of mistrust and not knowing much about health. Using telehealth after COVID-19 looks promising for better engagement and helping with screening.
For more info, check out the detailed guidelines. They go in-depth on a patient-focused approach to lung cancer screening.
Implementation and Uptake of Screening Programs
Lung cancer screening is key for finding the disease early, especially in high-risk groups like smokers. Even though these programs are beneficial, getting people to take part is hard. Making people aware and giving better access is important for getting those at risk to join.
Screening in High-Risk Populations
Outreach nowadays aims at those most at risk due to heavy smoking and other factors. It’s vital to get these people involved to boost screening rates. The UK Lung Screen Uptake Trial showed a 52-53% participation when specifically inviting these groups.
Current Status of Lung Cancer Screening
In the US, screening programs have greatly helped reduce deaths from lung cancer. The National Lung Screening Trial showed a 20% drop in deaths with low-dose CT scans. The USPTF supports these screenings, citing these results. Yet, just 14.4% of those who should get screened actually do. This shows we need to work harder on getting people screened.
The evidence is growing on the benefits of catching lung cancer early. We must push harder to get more high-risk people screened. The ACR Lung Cancer Screening Registry helps with this effort, tracking who gets screened.
Radiologist Recommendations and Follow-Up Protocols
Radiologists are key in lung cancer screening. They read low-dose computed tomography (LDCT) results carefully. Their skills make sure that follow-up plans work well. This helps keep an eye on patients with lung nodules.
Using tools like Lung-RADS is important. It makes communication and management suggestions about nodules clearer.
It’s important to follow set protocols. This reduces the chance of diagnosing cancer when it’s not there. These protocols also make sure patients get care on time. The American College of Radiology says yearly screening is needed for people 55 to 74 who have smoked a lot. They highlight the importance of having clear steps to take if results are positive.
Below is a table summarizing the follow-up recommendations based on nodule characteristics detected during screening:
| Nodule Size (mm) | Follow-Up Recommendation | Next Imaging |
|---|---|---|
| Less than 5 | Regular screening | 12 months |
| 5 to 6 | Consider follow-up | 6 to 12 months |
| Greater than 6 | Further evaluation needed | 3 months or refer to specialist |
These radiologist recommendations help patients get the most from lung cancer screening. They also lower the risks. Talking with healthcare providers about the pros and cons of screening is good for patients. It makes the screening process better.
Conclusion
The CT lung cancer screening guidelines stress the need for early detection and prevention. They focus on people aged 55 to 77 who have smoked a lot, at least 30 pack-years. For good results, it’s key that doctors and patients talk together. This helps patients understand the benefits and risks of LDCT screening.
Studies show that LDCT screenings are good at lowering deaths from lung cancer. They can reduce lung cancer deaths by 20% when compared to chest X-rays. Yet, there are challenges, like false positives and monitoring the screening process carefully. Putting these guidelines into practice can greatly help, especially those at high risk.
As more people learn about and can get to lung cancer screenings, we have a better chance to lower death rates from this terrible illness. We must keep educating and using the CT lung cancer screening guidelines. This effort will improve outcomes and give a brighter future to those in danger. For more details on these guidelines, visit the systematic review.