Did you know about 10-15% of lung cancer cases are because of inherited genes? This fact shows how genetics and lung cancer are connected. It’s a disease that leads to many deaths yearly in the U.S. Knowing how genes affect lung cancer risk helps us make better health choices.
Researchers are trying to understand why some people are more likely to get this disease. For those interested, there’s a lot of info out there. This includes how certain gene changes can cause cells to grow out of control. You can find out more about this at MedlinePlus.
Key Takeaways
- Understanding genetic factors is essential in assessing lung cancer risk.
- 10-15% of lung cancer cases relate to inherited genetic factors.
- Research continues to uncover the links between genetic mutations and lung cancer.
- Informed health decisions can significantly impact lung cancer outcomes.
- Recognizing individual genetic predispositions can aid in early detection strategies.
Understanding Lung Cancer
Lung cancer is a major health issue caused by cells growing out of control in the lungs. It’s vital to know the Lung Cancer Basics for awareness and prevention. This cancer comes in two main types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). They differ in behavior and how they’re treated.
Signs of lung cancer can look like other breathing problems. A constant cough, losing weight, and breathlessness are key signs. There can also be chest pain and blood when coughing. These make it hard to catch early.
The Causes of lung cancer include several factors, with smoking being the top one. Smoking greatly increases cancer risk. Being around harmful pollutants, like asbestos, adds to this risk. Having lung cancer in the family might also make you more prone to it, due to genetics.
Knowing these facts helps us understand the risks better. And it shows how early detection and healthy living can lower lung cancer risks.
| Type of Lung Cancer | Characteristics | Treatment Options |
|---|---|---|
| Non-Small Cell Lung Cancer (NSCLC) | Most common type, slower growth | Surgery, chemotherapy, targeted therapy |
| Small Cell Lung Cancer (SCLC) | Aggressive and fast-growing | Chemotherapy, radiation therapy |
The Role of Genetics in Health
Genetics is key in shaping our health. The health impact of our genes can make us more likely to get sick, like with lung cancer. Our genes outline not just how we look, but also our risk for health issues. Knowing our genetic risks helps create personal health plans.
Genes affect us in many ways. They can change how our bodies process things, react to the environment, or keep cells healthy. As we learn more, we see how vital genetics are for our health. They lead us to new ways to prevent and treat diseases.
Personalized medicine is now more important than ever. It moves us beyond general treatments. Instead, care is based on our unique genes. This can make treatments work better and improve lives.

| Inherited Trait | Potential Health Impact |
|---|---|
| Family History of Lung Cancer | Increased risk of developing lung cancer |
| BRCA Gene Mutations | Higher likelihood of various cancers |
| Heightened Cholesterol Levels | Risk for cardiovascular diseases |
| Predisposition to Diabetes | Increased risk of metabolic disorders |
Learning about genetics and health helps us better care for ourselves. Knowing our genetic risks means we can focus on preventing and catching diseases early. This proactive stance on health management is a game-changer.
Genetic Factors That Contribute to Lung Cancer Risk
Knowing the genetic factors that affect lung cancer risk is crucial. It helps in both stopping and treating the disease. Scientists have found many genes related to lung cancer. These can greatly raise a person’s chance of getting sick. Spotting these genes helps doctors pick better treatments.
Specific Genes Linked to Lung Cancer
Experts have pinpointed several key genes tied to lung cancer. Each has a critical role in how the disease starts and grows. Here are some important ones:
- EGFR: Changes in this gene are found in a common type of lung cancer called non-small cell lung cancer.
- ALK: Rearrangements in this gene lead to a certain lung cancer type. It’s often in young, non-smoking patients.
- KRAS: This gene’s variants mean a worse outlook for lung cancer patients, showing the need for specific treatments.
Impact of Gene Variants on Lung Health
Some gene variants can change pathways that are vital to lung health. This can make cancer more likely. These changes also impact how well treatments work for some people. For instance, certain variants may make common treatments less effective. This shows why tailored healthcare is key in fighting lung cancer.
How Heredity Affects Lung Cancer Susceptibility
The link between genetics and lung cancer risk is key in grasping an individual’s risk. Knowing if family members had lung cancer is important. Studies show a strong link between family history and increased risk in relatives.
Having a first-degree relative with lung cancer makes you more likely to get it too. This fact highlights how big a role genetics play in lung cancer risk.
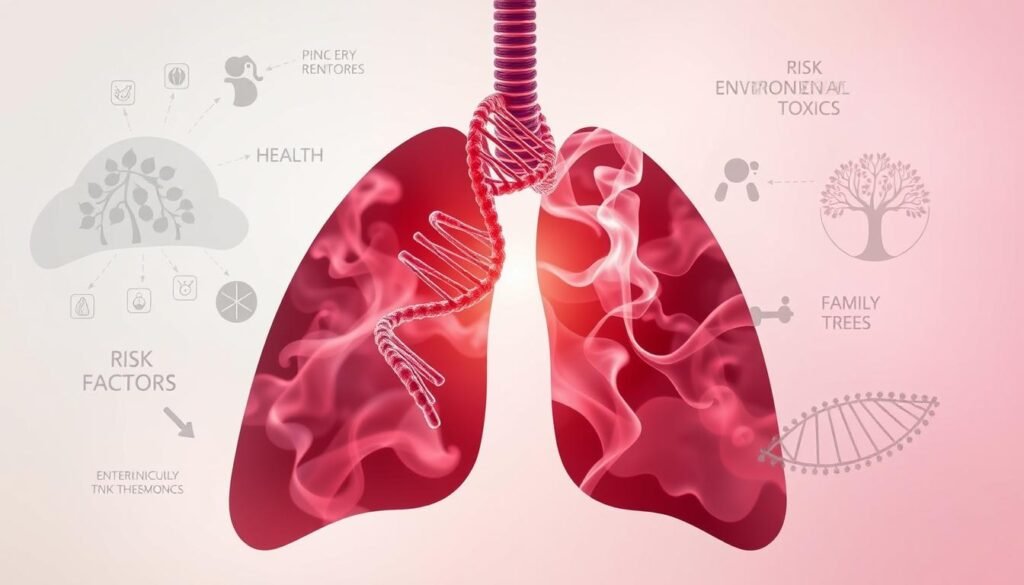
Research points to specific genes that might make lung cancer more likely. It’s important to know your family’s health history. Genetics and shared environments get passed down, raising lung cancer risk in families.
| Family History | Lung Cancer Risk Level |
|---|---|
| No Family History | Low Risk |
| One First-Degree Relative | Moderate Risk |
| Two or More First-Degree Relatives | High Risk |
| Family History of Other Cancers | Variable Risk |
Knowing how genetics mix with personal risks is crucial for prevention and awareness. Being aware of your family history helps make smarter choices about health, screenings, and prevention.
The Importance of DNA and Chromosomes in Cancer Development
It’s crucial to know how DNA and chromosomes relate to cancer. DNA is the blueprint for cell functions. Chromosomes keep our genetic material safe. When this balance fails, cancer can start.
The Structure of DNA
DNA is made of two strands that twist into a double helix. It has nucleotide sequences that carry genetic info. Each nucleotide has three parts: a phosphate group, a sugar unit, and a nitrogenous base. This structure guides cell behavior and disease risk. If DNA’s stability is at risk, mutations may occur, leading to cancer.
Chromosomal Abnormalities and Cancer
Chromosomes face changes that affect cells and may lead to cancer. These include duplications, deletions, and translocations. Such shifts can mess up gene function. This can cause cells to grow out of control. To help prevent cancer, genetic counseling and checking for environmental risks are key. For more on reducing risks, see this preventive healthcare guide.
Understanding Gene Expression and Its Role in Lung Cancer
Gene expression is key in how lung cancer forms and grows. It’s how certain genes turn on to make proteins that change cell behavior. If gene expression goes wrong, it can cause cells to grow out of control and turn into tumors. Different patterns of gene expression tell us about the types of lung cancer and how they work.
Studies show that changes in how some genes are expressed can lead to lung cancer spreading. For example, oncogenes might get switched on, making cells divide more. At the same time, tumor suppressor genes might stop working right, letting cells grow too much. Knowing about these changes helps us understand lung cancer better.
Looking at gene expression can help find markers for early detection and treatment. When we know which genes are linked to lung cancer, we can create therapies aimed at those specific problems. This way, treatment can be more directed and effective.

The Relationship Between Congenital Disorders and Lung Cancer
People born with certain genetic conditions may face a higher risk of getting lung cancer. These conditions can make them more vulnerable to cancer-causing factors in their environment. Knowing about these risks is important for early detection and prevention.
Studies have found that congenital pulmonary airway malformations, or CPAMs, can increase the risk of lung cancer. This happens because of harmful gene variants related to this cancer. It’s critical to understand how these genetic conditions can increase lung cancer risk. This knowledge can help in finding it early and possibly preventing it with surgery.
Looking deeper into how genetic issues linked with birth defects can affect lung cancer is key. Some genetic changes can interfere with how the lungs grow and develop. They might raise the chances of getting cancer. Learning more about these mutations helps highlight their role in increasing lung cancer risk.
| Congenital Disorder | Associated Lung Cancer Risk Factors | Notable Genetic Factors |
|---|---|---|
| Congenital Pulmonary Airway Malformations (CPAMs) | Increased tumor development risk | Variants in genes regulating airway development |
| Genetic Syndromes (e.g., Li-Fraumeni, Cowden) | Higher susceptibility to lung cancer | TP53, PTEN mutations |
| Hereditary Hemorrhagic Telangiectasia (HHT) | Potential for lung vascular malformations leading to cancer | ENG, ACVRL1 mutations |
Learning about the link between congenital disorders and lung cancer can help create better ways to prevent the disease. As research continues, we’ll find out more about these connections. This will help in managing the risk of lung cancer more effectively.
You can get more details on this topic here.
Genotype Versus Phenotype: Impact on Lung Cancer Risk
The difference between genotype and phenotype is key in understanding lung cancer risk. Genotype is the unique genetic code of a person. Phenotype is the visible traits shaped by both genetics and environment. Knowing how they interact helps predict lung cancer risk and create personal prevention plans.
Defining Genotype and Phenotype
Genotype is the set of genes you have. These genes affect many body processes and may increase cancer risk. Phenotype includes things like physical traits and behaviors. For example, a person’s lung health, affected by both genetics and environment, is part of their phenotype.
Real-Life Implications of Genotype-Phenotype Correlation
Understanding the link between genotype and phenotype is crucial in lung cancer risk evaluation. It’s key to personalized medicine. Some genetic markers may make people more prone to lung cancer. Spotting these connections helps doctors prevent and keep an eye on lung cancer risks.
| Aspect | Genotype | Phenotype |
|---|---|---|
| Definition | Genetic makeup of an individual | Observable characteristics |
| Influence | Inherited from parents | Affected by environment and lifestyle |
| Relevance to Lung Cancer | Identifies genetic risk factors | Reflects health conditions and behaviors |
| Use in Healthcare | Guides genetic testing and counseling | Informs lifestyle modifications and monitoring |
Exploring Genomics and Lung Cancer Research
The genomics field is changing lung cancer research in big ways. It helps researchers break down complex genetic details. Now, they can find specific genetic changes that cause lung cancer. This knowledge is reshaping our understanding and treatment of the disease.
Researchers now focus on early detection and creating better treatment plans. They use genetic studies to achieve this goal.
Genome-Wide Association Studies (GWAS) show how genetic differences affect lung cancer risks. This work leads to targeted therapies that match a person’s genetic makeup. Personalized medicine is getting real, thanks to our deeper grasp of lung cancer genetics.
This offers new treatment paths that fit each person’s genes perfectly.
Combining different data types, like genomics and transcriptomics, opens new research doors. These methods help find genes linked to lung cancer. They spotlight potential new drugs and treatments.
Tools like MR-Egger regression and IVW are key in making sense of complex genetic data. They help keep lung cancer research accurate and meaningful.
Geneticists, oncologists, and researchers are working together more than ever. Their teamwork is set to bring breakthroughs in lung cancer care. This will lead to better treatments and a push towards personalized care.
For more on these research methods and their impact, check out Lung Cancer Research.
Epigenetics: A Key Player in Lung Cancer Development
Epigenetics helps us understand the complex link between our genes and environment. It explains how gene activity can change without altering the DNA itself. This knowledge is crucial when determining why some people get lung cancer while others do not.
How Environmental Factors Influence Epigenetics
Our surroundings greatly affect our epigenetic makeup. Things like air pollution, smoking, and what we eat can alter our genes in ways that increase our cancer risk. Knowing how these factors play together helps in identifying those more likely to develop lung cancer. It also points towards ways to prevent it.
The Potential for Epigenetic Therapies
Research in epigenetics is paving the way for new cancer treatments. These therapies focus on fixing the gene expression changes that contribute to lung cancer. They offer hope for customized care that tackles the disease and lessens the impact of harmful environmental factors. Such breakthroughs could revolutionize how we handle lung cancer.
Conclusion
This article highlights the link between genetics and lung cancer risk. It explores how DNA and family history impact health. Knowing about these factors helps people make better choices for their health.
Genetics is changing how we prevent and treat lung cancer. The use of new research lets us create personal care plans. It could lower the number of lung cancer cases and improve patient care. Ongoing studies about ethics in genetics are crucial too, as noted in this detailed report.
Seeing lung cancer through genetics opens new ways to manage it. Discovering genetic risks helps people choose the right health actions. This could lead to a better future in fighting lung cancer.