Did you know nearly 228,000 Americans get diagnosed with lung cancer each year? This huge number shows why it’s so important to stage lung cancer correctly. Staging helps figure out which treatment works best. Lung cancer comes in different stages and types. Each one affects how the cancer spreads and what treatments you can use.
An overview of lung cancer and how it’s staged is given here. We’ll look at how lymph nodes play a part in how the cancer grows. Getting the stage right is key. It helps make a good treatment plan and predict how well patients will do. The TNM system checks the tumor size, lymph node involvement, and if the cancer has spread. This gives important information about this complex illness.
Key Takeaways
- Lung cancer lymph node staging is crucial for determining disease severity and treatment options.
- The TNM staging system assesses tumor size, lymph node spread, and metastasis.
- Non-small Cell Lung Cancer has distinct stages, ranging from 0 to IV.
- Accurate staging directly influences the selection of treatments and prognosis.
- Statistical indicators guide effective treatment planning based on staging characteristics.
Introduction to Lung Cancer Staging
Lung cancer staging is key to understanding how far the disease has spread. It guides doctors to manage the cancer effectively. Knowing the size of lung nodules, the location of cancer cells, and if it has spread is vital. This information shapes customized treatment plans and predicts outcomes for patients.
The lung cancer staging process uses the TNM system. It looks at the tumor’s size and location (T), checks lymph node involvement (N), and finds any distant metastasis (M). Advances in PET scans have improved early detection of lung cancer. This leads to quicker, more effective treatments.
Knowing the stages of lung cancer helps doctors and patients make better decisions. It gives patients crucial information about their health. This knowledge makes discussions about treatment options more productive.
More information on staging methods is available from the International Association for the Study of Lung. Understanding lung cancer staging shows the value of early detection. Early diagnosis greatly improves patient outcomes.
Importance of Accurate Staging
Accurate lung cancer staging is key to finding the right treatment. It shows how far the disease has spread, including if it has reached the lymph nodes. This helps doctors decide the best way to treat it.
The more precise the staging, the better the outcomes for patients. For example, a study showed accurate staging is great at spotting metastases. If the cancer hasn’t moved beyond the primary tumor, patients have a better chance. This proves that early and correct diagnosis sets the stage for what to expect.
Multidisciplinary teams (MDTs) play a vital role in treating lung cancer. By bringing together lung doctors, radiologists, and cancer specialists, patients get diagnosed faster and more accurately. This joint effort means quicker treatment and better survival chances.
However, challenges remain despite medical advances and FDA-approved treatments. Many healthcare professionals don’t follow the guidelines for checking lung nodes closely. Patient worries and not having enough time also make sticking to these protocols hard. This highlights the ongoing need for education and improvement.
In short, getting lung cancer staging right is critical. It guides the treatment plan and impacts patient survival and the quality of care. Working with a team approach improves the precision of staging. This, in turn, helps with better managing the patient’s care and outcomes.
The Basics of Lung Cancer Diagnosis
Diagnosing lung cancer is crucial for effective treatment. It often starts with X-rays and CT scans. These tests spot potential issues in the lungs. Symptoms might point to problems, or doctors might find something during routine checks.
Screening is key for those at higher risk. This includes people over 50 who smoked a lot. It’s also for those who quit smoking in the last 15 years. This early detection can greatly improve treatment success.
To confirm cancer, doctors may need to do a lymph node biopsy for lung cancer. Getting an accurate diagnosis is important. Lung cancer stages go from 1 to 4. Early stages mean the disease is less widespread. Knowing the stage helps doctors treat it right.
Most lung cancers are called non-small cell lung cancer (NSCLC). They make up about 80–85% of cases. The rest are small cell lung cancer (SCLC), about 15–20%. Catching lung cancer early is key to helping patients.
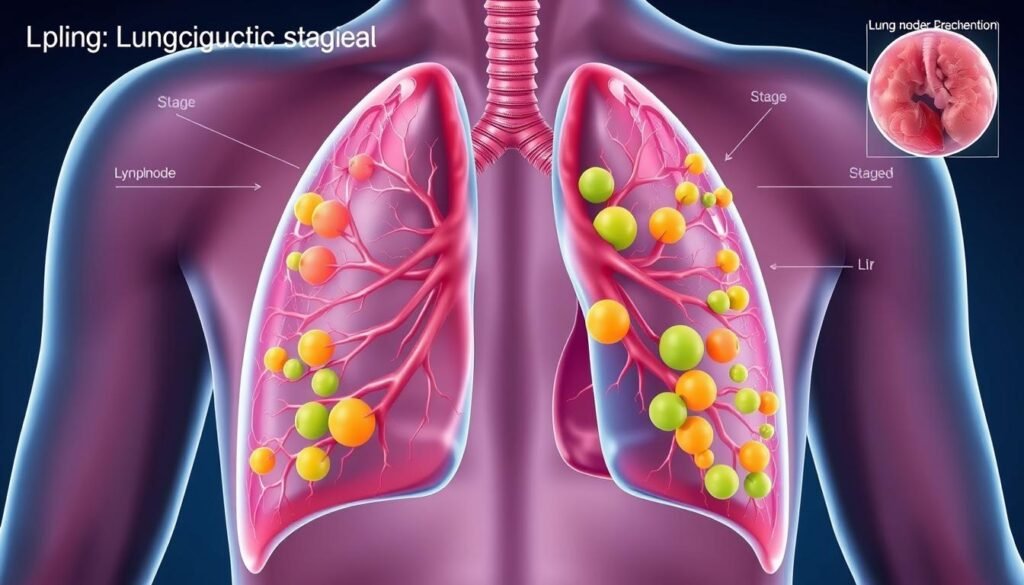
Understanding Lymph Node Involvement in Lung Cancer
Lymph nodes play a key role in our immune system. They are often where lung cancer starts to spread. Knowing the state of these nodes during staging is crucial for lung cancer. This affects treatment decisions and how well a patient might do in the future. Even early-stage lung cancers, like stage 2A, can spread to lymph nodes without being called metastatic.
To assess lymph node involvement, doctors use several tools. These include CT, MRI, PET scans, and endobronchial ultrasound. A precise check-up shows how far the cancer has spread and outlines possible treatments. The lymph nodes are classified from N0 to N3 in the TNM system. NX means doctors can’t tell if nodes are involved. Survival rates drop as the cancer spreads from N0 to N3. This makes understanding these classifications vital.
The table below shows important details on lung cancer lymph node staging:
| Classification | Definition | Survival Rate |
|---|---|---|
| N0 | No lymph node involvement | 62.8% |
| N1 | Spread to nearby lymph nodes | 34.8% |
| N2 | Spread to mediastinal nodes | 34.8% |
| N3 | Spread to distant lymph nodes | 8% |
Symptoms like neck swelling or chest pressure may hint at lymph node involvement. Depending on the lung cancer stage and general health, surgery like SLND might be an option. The link between lymph nodes and patient outcomes underlines the need for careful staging.
The TNM Staging System Explained
The TNM staging for lung cancer is key in knowing how far the cancer has spread. It breaks down into three main parts: tumor size, lymph node involvement, and metastasis. Grasping these parts helps doctors predict the cancer’s behavior and plan treatment.
In the latest TNM edition, changes were made. These include more detailed tumor size categories and new classifications for tiny cancers. Moreover, the way doctors define distant metastasis has been refined, improving accuracy.
Staging starts with the tumor’s size and spread, referred to as the T component. Next is the N component, which looks at lymph nodes nearby. These factors are crucial because they help determine the survival chances and treatment success.
The M component deals with distant metastases, pointing to a more serious stage of lung cancer. This detailed TNM system aids doctors and researchers in understanding the disease better. It leads to more personalized care for patients.
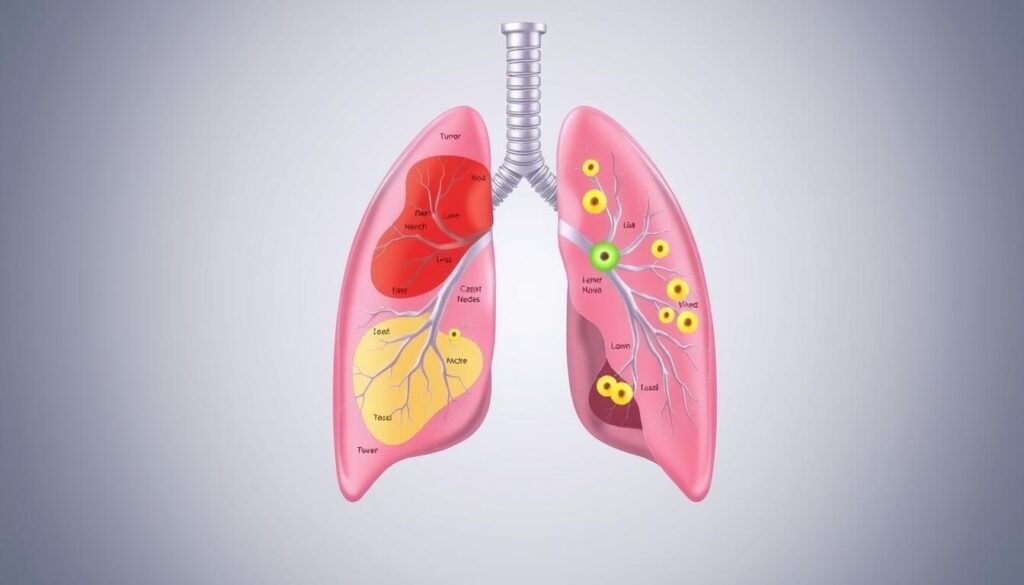
Components of Staging: Tumor, Node, and Metastasis
Staging lung cancer is key for planning treatment and predicting outcomes. The TNM system helps understand the disease’s severity. It looks at tumor size, if cancer has spread to lymph nodes, and if there is metastasis. This detailed check-up guides in choosing the best treatment for the patient.
Defining Tumor Size and Location
The size and place of the tumor are crucial for lung cancer staging. In the TNM system, tumor stages range from T1 to T4. T1 means the tumor is small and only in the lung. T4 means the tumor is big and may have spread. Knowing the tumor’s exact size and where it’s located helps decide on the right treatment.
Assessing Regional Lymph Node Involvement
It’s important to know if cancer has spread to lymph nodes. The N stage tells us this, from 0 to 3. N0 means no spread to lymph nodes. N3 means a lot of spread. Knowing this helps choose treatments, like radiation or medicines to stop further spread.
Understanding Metastasis Status
Knowing if cancer has spread far is critical. In the TNM system, M0 means no spread. M1 means it has spread far, like to the liver or brain. This stage, IV, may need different care to make life better. Learning about metastasis helps make care decisions that fit the patient’s needs.
If you want to know more about lung cancer stages, check the TNM staging system. It’s always getting better to help manage cancer more clearly.
Key Factors in Lung Cancer Staging
It’s vital to grasp the key factors in lung cancer staging for accurate diagnosis and managing treatment. Elements like tumor type, size, and the patient’s health are important. About two-thirds of people first found to have non-small cell lung cancer (NSCLC) show symptoms.
75% of these patients have a persistent cough. Symptoms such as shortness of breath affect 50% to 60%, and coughing up blood impacts 25% to 40%. These signs can show the disease’s extent, helping doctors make a thorough lung cancer diagnosis.
Wheezing or stridor could mean the cancer has advanced. Spotting and tackling these symptoms early is key for setting the right treatment path.
Some patients may develop paraneoplastic syndromes, indicating serious disease. For instance, 35% might have clubbing of the fingers, linked to severe illness.
The AJCC TNM staging system is key in lung cancer categorization. It considers tumor size, lymph node spread, and organ spread. This system is crucial for deciding on lung cancer treatment options and understanding the prognosis.
About one in three small cell lung cancer (SCLC) cases are found in the limited stage. Most others show extensive disease. Staging affects treatment choices. The TNM findings are vital for therapy decisions, underlining the importance of research and learning for better outcomes.
| Factor | Description | Impact on Staging |
|---|---|---|
| Tumor Size | Measurement of the primary tumor’s physical dimensions | Affects T category in TNM system |
| Lymph Node Involvement | Assessment of cancer spread to nearby nodes | Affects N category in TNM system |
| Metastasis | Evaluates spread to distant organs | Affects M category in TNM system |
| Overall Health | Patient’s general health will influence treatment options | Guides personalized treatment plans |
Insights show early detection greatly boosts outcomes. Recognizing primary symptoms and the lymphatic spread of lung cancer is crucial. Visit this resource to learn more. Understanding these key factors in lung cancer staging is vital for effective treatments and patient care.
What is Lung Cancer Lymph Node Staging?
Lung cancer lymph node staging is key in understanding how far the disease has progressed. It checks the regional lymph nodes for cancer involvement. This is crucial for deciding on treatment.
The TNM system is used to classify lymph node involvement. Nodes are labeled as eN0 (no cancer), eN1, eN2, or eN3, based on the extent of spread.
Non-small cell lung cancer has four stages, from I to IV, with more detailed classifications like IIIA or IIIB based on tumor size. Contrarily, small cell lung cancer is either “limited” or “extensive.” This difference affects treatment choices a lot.
The role of regional lymph nodes in lung cancer is huge. They clue in doctors on whether the cancer might spread. To check the nodes, doctors might do a biopsy through various ways such as bronchoscopy or CT-guided needle biopsy.
- Understanding lymph node involvement: Determines treatment strategy.
- Staging aids in predicting outcomes: Higher stages usually mean a tougher fight ahead.
- Imaging techniques: CT and PET-CT scans help doctors get the full picture.

In summary, knowing about lymph node involvement in lung cancer is vital. It helps create better treatment plans and can improve a patient’s chances. Recognizing symptoms early and getting medical advice is crucial in fighting lung cancer.
| Staging Classification | NSCLC | SCLC |
|---|---|---|
| Stage I | Tumor localized | Limited Disease |
| Stage II | Localized with lymph node involvement | Limited Disease |
| Stage III | Regional lymph node involvement (N1, N2, N3) | Extensive Disease |
| Stage IV | Metastasis to distant organs | Extensive Disease |
Pathologic vs. Clinical Staging
Understanding the difference between pathologic staging and clinical staging is key in treating lung cancer. Clinical staging happens before any treatment starts. It uses imaging and biopsies to check how far the cancer has spread. Doctors use it to plan treatments and surgeries.
Pathologic staging, on the other hand, is done after removing the tumor. Doctors closely examine the removed tissue. This helps them know the cancer’s real size and spread. Studies show that about half the time, clinical and pathologic staging match. Proper T staging was accurate in 73.9% of cases. Some patients were found to be overstaged or understaged.
Clinical staging can sometimes get the cancer’s spread wrong, especially in the lymph nodes. About 19.4% of patients were overstaged, and 25% understaged. These mistakes show why pathologic staging is crucial for correct treatment.
New methods are making staging more precise, especially determining TNM status. This status looks at tumor size, lymph node involvement, and whether the cancer has spread. Before surgery, 48% of certain stage patients were underestimated. After surgery, the staging was confirmed for 52%.
The TNM system helps guide the right treatment for each patient. By knowing both staging methods, better choices can be made for the patient. For more details on these staging differences, check this link.
Impact of Staging on Treatment Options
The stage of lung cancer plays a key role in choosing treatments. Knowing the cancer’s stage helps doctors decide on the best treatment plan. The disease’s stage lets doctors know if surgery, chemotherapy, immunotherapy, or radiation is best.
Custom treatments aim to improve patients’ chances of beating lung cancer. The right therapy can target the disease’s specific traits.
Types of Treatments Based on Staging
Different stages of lung cancer need different treatments. See the table below for the usual treatments based on cancer stage:
| Stage | Treatment Options | Rationale |
|---|---|---|
| Stage I | Surgery, possibly followed by adjuvant chemotherapy | Localized disease with a good prognosis; aims for complete removal of the tumor |
| Stage II | Surgery with adjuvant chemotherapy or radiation | Higher risk of recurrence; need for additional treatment to eliminate residual cancer |
| Stage III | Chemotherapy, radiation therapy, and possibly surgery | Involvement of lymph nodes; combination treatments can enhance effectiveness |
| Stage IV | Targeted therapy, immunotherapy, or supportive care | Advanced disease with potential metastasis; focus on quality of life and symptom management |
Lymph node involvement affects treatment choices for lung cancer. Knowing the N stage helps pick patients for pre-surgery treatment, which can lead to better outcomes. Early and correct staging guides the best treatment, helping improve survival rates.
Lung Cancer Prognosis Factors
The outlook for those with lung cancer hinges on several factors. These include the stage of cancer, the patient’s health, and how well they respond to treatment. A key factor is whether the cancer has reached the lymph nodes, which is crucial for predicting outcomes.
Staging lung cancer based on lymph node involvement helps gauge how far the disease has spread. Survival rates differ significantly depending on this factor. Information from the SEER database shows varying survival rates for non-small cell lung cancer (NSCLC) based on lymph node involvement. Here’s what the data tells us:
| Stage | 5-Year Survival Rate for NSCLC (%) |
|---|---|
| Localized | 65 |
| Regional | 37 |
| Distant | 9 |
| All Stages Combined | 28 |
For small cell lung cancer (SCLC), the numbers look a bit different:
| Stage | 5-Year Survival Rate for SCLC (%) |
|---|---|
| Localized | 30 |
| Regional | 18 |
| Distant | 3 |
| All Stages Combined | 7 |
These survival rates show the significant impact that lymph node status has on outcomes. The more lymph nodes affected, the worse the prognosis typically is. Additional factors such as symptoms, tumor size, and blood vessel involvement also affect the prognosis negatively.
Understanding these prognosis factors is crucial for those diagnosed and their families. It makes discussing treatment options and outcomes more informative. Knowing the details of one’s lung cancer stage and prognosis factors can change how they approach their care and management.
For more details on how lymph node involvement affects lung cancer outcomes, you can check a detailed study here.
Conclusion
Lung cancer lymph node staging is key for correctly diagnosing and treating lung cancer. It helps find out how far the disease has spread. This is important for choosing the best lung cancer treatment. Since non-small cell lung cancer (NSCLC) is the most common, knowing all about staging can really help patients.
Getting the stage right makes a big difference in lung cancer survival chances. For advanced stages with lots of lymph node involvement, survival rates are low. Only less than 5% live for five years in advanced stages. But, if only one N2 zone is positive, the survival rate jumps up. This shows why it’s critical to get a very precise staging and keep an eye on it during treatment.
Understanding your own staging details can give you power in your treatment path. Using modern methods like FDG PET to check for metastases focuses on the best treatment options. It also looks at new ways to improve lung cancer lymph node staging. This is all part of the ongoing fight against cancer.