Every year, over 150,000 people in the United States deal with malignant pleural effusion (MPE) because of lung cancer. This condition deeply affects their life expectancy and care quality. Lung cancer is the top cause of cancer deaths worldwide, bringing about issues like fluid in the lungs. It’s critical for patients and their doctors to understand what lung cancer fluid in lungs means for life expectancy.
The average life span for those with MPE from lung cancer is between three to twelve months. With advances in healthcare, managing symptoms and discussing future outcomes have become crucial. These efforts help people find the right treatments. For more insights, check out this article.
Key Takeaways
- Malignant pleural effusion complicates care for over 150,000 lung cancer patients annually in the U.S.
- Median survival for patients with MPE can range between 3 to 12 months.
- Understanding the prognosis of pleural effusion in lung cancer is crucial for effective treatment discussions.
- Effective symptom management and communication significantly enhance patient quality of life.
- Healthcare providers often face challenges predicting patient survival accurately.
Understanding Lung Cancer
Lung cancer begins when cells in the lungs grow uncontrollably. This can lead to spreading, or metastasis, to other body parts. There are two main kinds: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC makes up about 80-85% of cases and grows slower than SCLC.
People with lung cancer may notice several symptoms. These include a constant cough, chest pain, and hard time breathing. It’s crucial to catch these signs early for a better chance at survival. For example, stage 1 lung cancer patients have close to a 65% chance of surviving five years. But, this chance falls to around 5% for stage 4 lung cancer. Knowing early symptoms can really make a difference.
If you’re at high risk for lung cancer, watch for any lasting symptoms. Catching lung cancer early can improve treatment success and outcomes. For insights into spotting early lung cancer, check out early signs of lung cancer.
What is Fluid Buildup in Lung Cancer?
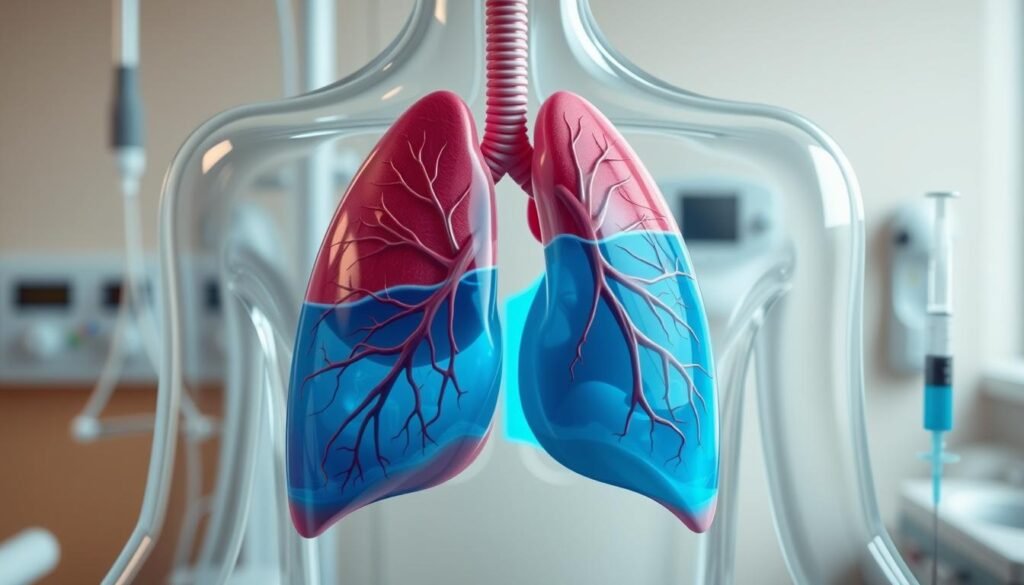
Fluid buildup in lung cancer, or pleural effusion, is when extra fluid collects around the lungs. This is a big worry for lung cancer patients because it might mean the cancer has spread to the pleura. The fluid often has cancer cells, pushing against the lungs and causing problems like shortness of breath and coughing.
The main pleural effusion causes are tied to the fluid balance being upset by the tumor. Lung cancer is the top reason for malignant pleural effusion, making up about one-third of the cases. Breast cancer and lymphoma can cause it, too. Finding the root cause is key for choosing the right treatment.
About 7% to 23% of lung cancer patients get malignant pleural effusion. It affects about 15% of people with cancer. Almost half the time, this happens in stage 4 cancer. These numbers show how serious pleural effusion is in lung cancer. They stress the importance of spotting it early and managing it right away.
When there’s too much fluid in the pleural space, the body tries to fix it. But cancer makes it hard. Treatments like thoracentesis can help in 60% to 90% of cases. Pleurodesis is also an option to stop more fluid from building up. It’s vital for patients and doctors to understand how malignant pleural effusion shows up. This helps in managing it better.
The Connection Between Lung Cancer and Pleural Effusion
Lung cancer and pleural effusion have a strong link. This is mainly because lung cancer spreading can affect the pleura. The pleura is a double-layered membrane around the lungs. When affected, it changes how fluid is normally handled in the pleural cavity. This leads to a condition called malignant pleural effusion (MPE). There are many reasons why this develops, showing the complex pleural effusion mechanisms involved.
About half of all lung cancer patients might face pleural effusion. This fact underlines why doctors must watch out for this complication. The cancer triggers an inflammation, causing more cytokines to release. These cytokines help fluid build up in the pleural space. They play a big role in the lung cancer pleural effusion connection. They not only help create the fluid but also keep it there, starting a harmful cycle.
Lung cancer spreading can make treating the disease harder and varies by the type of cancer. Differences exist between small cell lung cancer and non-small cell lung cancer types like squamous cell carcinoma, adenocarcinoma, and large cell carcinoma. Each has its own way of affecting the pleura. Knowing the pleural effusion mechanisms helps with early diagnosis and planning the right treatment as lung cancer gets worse.
| Factor | Impact on Pleural Effusion |
|---|---|
| Lung Cancer Type | Different types may exhibit varying rates of pleural effusion development. |
| Metastatic Spread | Increased incidence of effusion with pleural involvement. |
| Inflammatory Response | Stimulates cytokine release, promoting fluid buildup. |
| Patient Prognosis | Pleural effusion presence can complicate treatment outcomes. |
Symptoms of Pulmonary Effusion in Lung Cancer
People with lung cancer often face many symptoms. These symptoms can greatly affect how they feel every day. One major concern is pleural effusion, which has clear signs.
- Shortness of breath: This makes it hard to breathe, especially when lying down or doing exercises.
- Sharp chest pain: Fluid buildup can cause sharp pains in the chest.
- Cough: A lasting cough may get worse over time.
- Fatigue: Feeling tired and weak can change daily life.
- Unexpected weight loss: Losing weight without trying can be concerning.
Lung cancer symptoms like these show the disease may be getting worse. It’s important to notice these signs early. Early spotting means better chances to manage and treat them. If you’re dealing with lung cancer, keep an eye on these symptoms. Talk about any worries with your doctor.
| Symptom | Description |
|---|---|
| Shortness of breath | Difficulty in breathing, especially when lying down. |
| Sharp chest pain | Stabbing pain in the chest area, often worsening with deep breaths. |
| Cough | A persistent cough that can become increasingly severe. |
| Fatigue | A general feeling of tiredness that does not improve with rest. |
| Unexpected weight loss | Significant weight loss without trying, often accompanied by decreased appetite. |
Knowing these symptoms is key to handling lung cancer well. Patients and those caring for them should talk often with doctors. Doing so helps make sure treatments are working as they should.
Diagnosis of Malignant Pleural Effusion
To diagnose malignant pleural effusion, a careful plan is needed for accuracy and effective treatment. First, doctors use imaging like chest X-rays or CT scans to find pleural effusion. These images show how much fluid is there and help guide what to do next.
Then, a procedure called thoracentesis is usually done. It involves taking out some fluid to examine under a microscope for fluid analysis. This step is key to see if cancer cells are present. If it’s hard to tell from the fluid, more tests, like biopsies, may be needed for a clear diagnosis.
For doctors, understanding how to diagnose malignant pleural effusion is vital. It helps them make the best treatment plan. Diagnosing malignant pleural effusion on time makes a big difference for patient care. It affects how long patients live and how well treatments work.
Lung Cancer Fluid in Lungs Life Expectancy
Having fluid from lung cancer in your lungs can change how long a patient might live. It’s key to know how this fluid buildup impacts a person’s survival chance. This knowledge is vital for understanding what those diagnosed with this issue might face.
Impact of Fluid Buildup on Prognosis
Malignant pleural effusion, or MPE, means there’s fluid in the space around the lungs. It’s linked to shorter survival times. If a patient has lung cancer with fluid buildup, their life expectancy could drop to between three to twelve months. This fact highlights the urgent need for effective treatment plans.
Statistics on Life Expectancy with Lung Cancer and Pleural Effusion
Lung cancer is a top cause of death from cancer. About 25% of all cancer deaths come from lung cancer. Here are some facts:
- The 5-year survival rate for lung cancer is about 18.6%.
- Small cell lung cancer’s 5-year survival rate is only 3%.
- Non-small cell lung cancer (NSCLC) has an 8% survival rate for those with cancer that has spread far. Stage 4 NSCLC has a very low survival rate of 9%.
- Between 25-30% of people with advanced NSCLC might live less than three months.
These statistics show how serious lung cancer is, especially when it comes with fluid in the lungs. It stresses the need for proper treatment and care. This information is crucial for those dealing with these complications.

Treatment Options for Malignant Pleural Effusion
Treating malignant pleural effusion focuses on easing symptoms and bettering life quality. Methods vary because each case is different. The main aim is to control fluid build-up. It’s key for patients and caregivers to understand the options for treatment. This knowledge helps make choices about care.
Palliative Care Approaches
Palliative care for lung cancer aims to comfort and support those with MPE. It includes strategies like:
- Thoracentesis: This is when a needle removes excess fluid, easing shortness of breath.
- Chemical pleurodesis: A substance is used to stick the pleura together, helping prevent more fluid build-up.
- Indwelling pleural catheters: These allow for ongoing fluid drainage, improving comfort for the patient.
Innovative Therapies in Managing Fluid Buildup
Research is bringing new treatments for pleural effusion. These may lead to better results for patients. Some advancements include:
- Immunotherapy: This method boosts the body’s defense against tumors, hoping to enhance patient outcomes.
- Targeted drug delivery systems: These focus on getting medication right where it’s needed, with fewer side effects.
- New generation agents like lobaplatin: Studies suggest this drug could make the pleura stickier, cutting down hospital stays.
Staying updated on new treatments brings hope to those dealing with MPE. As care options evolve, the focus is on tailored approaches. This is essential for improving comfort and life quality for patients.
| Treatment Method | Type | Benefits |
|---|---|---|
| Thoracentesis | Palliative | Immediate fluid removal providing breathlessness relief |
| Chemical Pleurodesis | Palliative | Prevents future fluid accumulation |
| Indwelling Pleural Catheter | Palliative | Continuous drainage for enhanced comfort |
| Immunotherapy | Innovative | Potentially boosts immune response against tumors |
| Lobaplatin | Innovative | Improves adherence, reduces hospitalization |
Managing Fluid in Lungs with Lung Cancer
Managing fluid in the lungs is vital for lung cancer patients. It includes medical treatments and care support. Many with lung cancer have malignant pleural effusion (MPE). This makes managing lung fluid crucial.
Thoracentesis and drainage catheters offer relief for those with MPE. These methods are key to managing lung fluid. They ease symptoms and boost life quality. Care plans should be tailored to each patient’s needs.
Treatment for cancer should align with fluid management. Options like pleurodesis can stop fluid from coming back. The choice depends on the patient’s health and cancer type. Sadly, those with MPE usually live between 3 to 12 months. This shows why early help and regular checks are needed.
It’s key to keep an eye on symptoms and get checked often. Patients need to know warning signs and tell their doctor about any changes. Early detection improves management. They can use resources like this guide to learn about symptoms.
| Management Strategy | Description | Expected Outcomes |
|---|---|---|
| Thoracentesis | Procedure to remove excess fluid from the pleural space. | Immediate symptom relief and diagnostic insights. |
| Drainage Catheter Placement | Indwelling catheter for continuous drainage. | Reduction of recurrent fluid accumulation. |
| Pleurodesis | Invasive procedure to adhere the pleurae, preventing fluid build-up. | Decreased recurrence rates for pleural effusions. |
Managing lung fluid in cancer patients needs teamwork. Doctors, patients, and families must work together. With the right knowledge and teamwork, we can better the treatment experience for everyone.
Survival Rates and Prognosis of Pleural Effusion in Lung Cancer
The outlook for lung cancer patients with malignant pleural effusion (MPE) is tough. On average, patients live three to twelve months after they’re diagnosed. Symptoms often lead to complications, lowering survival chances even more.
Many factors play a part in how long patients might live. Their overall health, the stage of cancer, and how well treatments work are key. Those with stage IV lung cancer without treatable mutations usually live about nine months. This highlights the disease’s seriousness.
Knowing the survival rates and prognosis helps patients and their families choose their treatment wisely. As medical care gets better, it’s important to keep track of how patients with MPE are doing.
| Condition | Median Survival (Months) | 1-Year Survival Rate | 5-Year Survival Rate |
|---|---|---|---|
| Unresectable Stage IV Lung Cancer | 9 | Less than 25% | Less than 1% |
| Symptomatic Malignant Pleural Effusion | 3 – 12 | Varies | Varies |
| Stage IIIA Lung Cancer | 10 – 14 | Less than 50% | Varies |
Factors Affecting Life Expectancy in Lung Cancer Patients
Life expectancy for those with lung cancer depends on many things. The kind of lung cancer and its stage when found are key. For instance, people with stage 4 non-small cell lung cancer (NSCLC) have only an 8% chance of living five more years if it spreads far. But, if the cancer spreads just nearby, the chance of living five more years goes up to 37%. Small cell lung cancer (SCLC) patients have only a 3% chance when the cancer is widespread.
Age also plays a big role. Older people usually have a harder time, facing low success with chemotherapy and more side effects like anemia. It’s also vital to consider a patient’s overall health. Previous health problems can make it harder to treat the cancer and shorten life expectancy.
The way patients respond to treatment affects their survival a lot. Advanced treatments like chemotherapy or immunotherapy are common, especially for late-stage SCLC. These treatments aim to fight the cancer, ease symptoms, and help patients live longer.
Dealing with malignant pleural effusion is another hurdle. It often requires care that focuses on easing both physical and emotional pain. About one-third of lung cancer patients find out they have it at stage 4. This shows why it’s crucial to catch it early and keep a close watch. For more on how age impacts this, see this study.
Conclusion
It’s crucial to grasp how lung cancer and fluid buildup are connected. This knowledge helps both patients and doctors. Pleural effusion, or fluid around the lungs, often means a worse outlook for lung cancer patients. Studies show these patients have a higher risk of shorter survival.
With new treatments for lung cancer, managing life expectancy is more possible than before. Doctors are finding better ways to ease symptoms caused by fluid buildup in the lungs. This focus on the patient and their education can truly make life better for those dealing with lung cancer.
The rise in lung cancer cases highlights the importance of understanding pleural effusion’s impact. Current research says the average survival time is four to seven months for those with this issue. Continued efforts in research and new treatments are key to helping these patients live longer and better lives.