Did you know only about 6 percent of people with stage 4 lung cancer live five years? This fact shows the tough battle with advanced lung cancer. Knowing what this means is key for patients and their families.
When lung cancer reaches the final stages, treatments aimed at curing often don’t work. Focus shifts to easing pain, emotional support, and looking into hospice care. Patients deal with hard symptoms like big weight loss, breath shortness from fluid, and brain issues if cancer spreads. It’s important for families to know these signs to help and support their loved one.
As the illness gets worse, patients might pull away from people and think deeply about life and death. Getting this helps create a caring place where patients feel dignity. It puts comfort and the best quality of life first every day.
Key Takeaways
- Stage 4 lung cancer has a 6 percent five-year survival rate.
- End stages focus on pain management and symptom alleviation.
- Emotional and spiritual changes are common in patients nearing death.
- Hospice care plays a vital role in providing comfort and support.
- Recognizing the symptoms of end-stage lung cancer is crucial for caregivers.
- Patients may experience unexpected surges of energy close to death.
Introduction to Lung Cancer
Lung cancer is a major health problem, causing about 25% of cancer deaths in the U.S. The lung cancer introduction shows why it’s important. Knowing about it helps catch it early and improve chances of survival. Every year, over 230,000 new cases are found. This shows how common this cancer is.
There are mainly two types of lung cancer: non-small cell (NSCLC) and small cell (SCLC). NSCLC has a better outlook if found early. Early-stage patients might not need heavy treatments like chemotherapy. SCLC, however, is often found at later stages, making treatment harder.
It’s crucial to know the risks, like smoking and pollution, to prevent lung cancer. Early symptom awareness boosts the chance for successful treatment. Knowing the possible progression helps understand the seriousness of the condition. For more on lung cancer stages, check the American Cancer guidelines.
What are the Causes of Lung Cancer?
Lung cancer is the top cause of cancer deaths around the world. It’s mainly caused by smoking, which accounts for about 90% of cases. Both people who smoke and those around secondhand smoke are at risk. In the U.S., secondhand smoke is the third leading cause of lung cancer.
People who’ve smoked for years are especially at risk. Small cell lung cancer often hits those who’ve smoked a lot over time. This kind of cancer is very serious.
Lung cancer falls into two types: small cell (SCLC) and non-small cell (NSCLC). SCLC makes up about 20% of cases. But NSCLC includes different kinds, like squamous cell carcinoma and adenocarcinoma. This shows how complex and varied lung cancer can be.
There are other causes beyond smoking. Radon gas exposure is a big risk, especially for non-smokers. It’s the second largest cause of lung cancer. Other dangers include asbestos, chromium, and specific chemicals.
Air pollution and arsenic in water also increase lung cancer risks. These factors are harmful to our health. They make the situation worse.
People with a family history of lung cancer should be extra careful. Genetics play a role in your cancer risk. Knowing all the causes and risks helps us be more aware. It highlights how vital it is to prevent lung cancer.
https://www.youtube.com/watch?v=ihCnDjyJv5c
Lung Cancer Symptoms to Watch For
Knowing lung cancer symptoms is crucial for early treatment. Early signs may hint at the start of the disease. Late signs often mean the cancer is advanced. Spotting these signs early is key for timely care.
Common Early Symptoms
Spotting lung cancer early is crucial. Early symptoms show up before the disease gets worse. Some common early symptoms are:
- A persistent cough that does not improve
- Coughing up blood or rust-colored sputum
- Chest pain that worsens with deep breathing or coughing
- Hoarseness and difficulty swallowing
- Unexplained weight loss and loss of appetite
- Shortness of breath and fatigue
- Weakness and recurring infections
- New onset of wheezing
Early symptoms can lead to early diagnosis. This improves the chances of successful treatment.
Symptoms in Advanced Stages
Advanced lung cancer, especially stage 4, shows different signs. Patients may have:
- Severe pain, especially if cancer spreads to the bones
- Swelling of lymph nodes
- Changes in the nervous system, like confusion and headaches
- Yellow skin and eyes (jaundice)
In advanced stages, lung cancer can cause specific syndromes. For example:
- Horner syndrome: Leads to drooping eyelids and smaller pupils.
- Superior vena cava syndrome: Causes swelling in the face and neck.
There are also paraneoplastic syndromes that impact many body parts. These include:
- Paraneoplastic endocrine syndromes: SIADH, Cushing syndrome, and high calcium levels.
- Paraneoplastic neurologic syndromes: Lambert-Eaton syndrome and damage to the cerebellum.
Understanding lung cancer symptoms helps patients and families act fast. It makes interacting with doctors more effective.
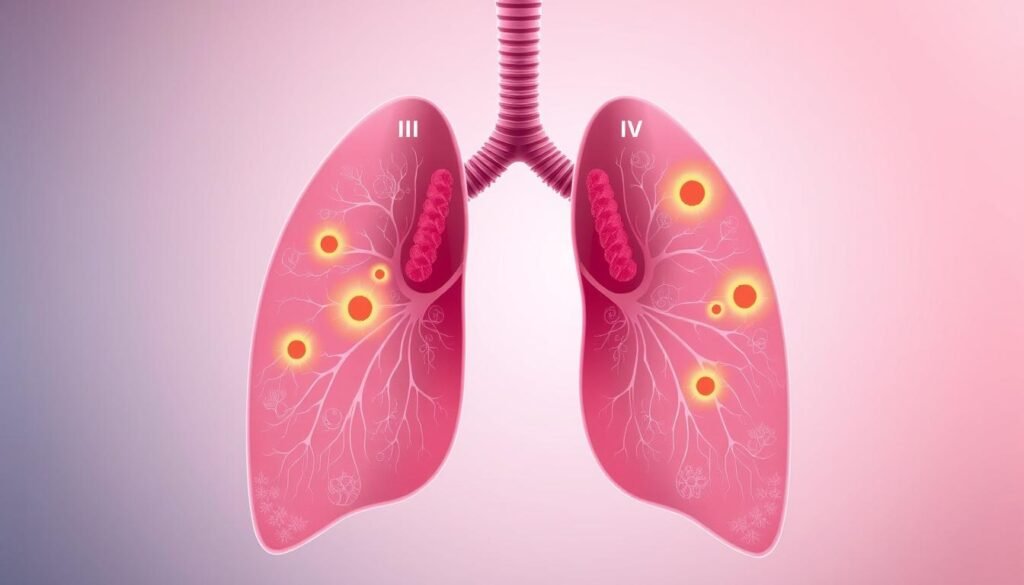
Understanding Staging of Lung Cancer
Lung cancer staging is crucial in diagnosing and treating the disease. The TNM system measures tumor size (T), lymph node involvement (N), and distant spread (M). This lets doctors figure out the stage of Non-Small Cell Lung Cancer (NSCLC), from stage 0 to IV.
Stage 0 is very early lung cancer, called carcinoma in-situ. Stage I has sub-stages 1A and 1B for slightly more advanced cases. By stage II, the disease is divided into IIA and IIB, showing further progression.
Stage III includes sub-stages IIIA, IIIB, and IIIC for extensive disease. Stage IV is the most advanced, with cancer spreading beyond the lungs.
Small Cell Lung Cancer (SCLC) has two stages: limited and extensive. Limited stage means cancer is in one lung and possibly nearby nodes. Extensive stage means the cancer has spread further, even to opposite lungs or distant organs.
KUnderstanding cancer stages helps with prognosis and treatment choices. The TNM system uses detailed assessments for treatment plans. It helps doctors predict patient outcomes better.
| Cancer Stage | Non-Small Cell Lung Cancer (NSCLC) | Small Cell Lung Cancer (SCLC) |
|---|---|---|
| Stage 0 | Carcinoma in-situ | N/A |
| Stage I | Sub-stages I-A and I-B | N/A |
| Stage II | Sub-stages IIA and IIB | N/A |
| Stage III | Sub-stages IIIA, IIIB, IIIC | N/A |
| Stage IV | Advanced, with metastasis | Extensive stage, with spread to distant organs |
The staging process gets more precise with scans and biopsies. This helps decide if cancer can be removed surgically. It leads to better treatment plans and patient outcomes.
End Stages of Lung Cancer
The last stages of lung cancer are a crucial period for patients. It is important for families and caregivers to know what signs to look for. This knowledge helps everyone be more ready and supportive.
Physical changes may happen that are hard to see. Being prepared and informed helps everyone cope better.
Recognizing Signs of End Stage
The final stage of lung cancer brings several clear symptoms. You might see:
- Persistent cough.
- Shortness of breath.
- Fluid build-up around the lungs.
- Severe fatigue.
- Loss of appetite.
- Nausea.
Delirium is common in the last days. This could mean changes in consciousness, pulling away, or feeling upset. Some patients may also see things that aren’t there as life ends.
Understanding these symptoms helps families get ready. It allows for talks about care wishes.
Physical Changes in Patients
Patients go through many physical changes at the end stages of lung cancer. Extreme tiredness is a big one, leading to sleep issues and weakness. Trouble breathing often gets worse because of the cancer and other lung diseases.
There are ways to manage pain with different medicines. Some can be given without needing to swallow, which can be helpful.
Patients might also deal with coughing, constipation, and eating problems. Treatments are available for these symptoms. Fever could signal infection, a reaction to drugs, or cancer actions. Sometimes, unexpected bleeding happens, showing the need for care that makes patients comfortable.
This information helps families face the emotional hard times during this stage.
For more info on dealing with lung cancer, including how it affects quality of life and treatment choices, families can visit this resource.
Impact of Lung Cancer on Quality of Life
Lung cancer changes lives deeply. It impacts not just those sick but also their families and caregivers. The disease is serious, with over 219,000 new cases each year in the United States. The death toll is over 159,000, showing the heavy lung cancer impact.
Many patients face hard physical symptoms every day. About 98% of them feel very tired, and 94% have trouble breathing. These challenges limit what they can do and cause emotional pain. Losing appetite, coughing, and constant pain take away from daily joys.

The emotional side of life with lung cancer is also tough. Many face stigma, feeling alone or judged by others. This is true for 30% to 95% of patients. Such stigma lowers their self-esteem, similar to other cancers.
Life quality differs for everyone, depending on money and age. Men often feel they have a better quality of life than women. This is especially true in social and mental areas. Older patients show different results. Some live worse than younger people, while others don’t.
Having good social support is key. It improves life quality for lung cancer patients. Getting support helps lessen loneliness and aids in better handling treatment. A good support group makes life with lung cancer easier to manage. It builds strength and fosters a sense of community.
Treatment Options During End Stages
In the last stages of lung cancer, the treatment goal changes. Instead of trying to cure, the aim is to improve the patient’s life quality with palliative care. This means managing symptoms in the best way possible. There are many treatment options to support patients during this time.
Doctors first review the patient’s health to choose the best treatments. Symptom management becomes key. They often prescribe medication for pain and other treatments to reduce any discomfort from lung cancer.
- Radiation therapy can be used to lessen pain or help with breathing problems caused by the cancer.
- Other end-stage treatment options may use targeted therapies that focus on the cancer’s genetic changes.
- Immunotherapy can also be an option, helping the immune system attack the cancer.
Talking clearly with doctors about treatment goals is very important. Patients and their families should think about what matters most to them. Adding palliative care means looking at all the patient’s needs, physical and emotional.
Choosing the best treatment for the final stages allows patients to face their journey with respect. It makes sure they get the care they want, keeping them as comfortable as possible during tough times.
Role of Palliative and Hospice Care
Palliative and hospice care are key for patients facing lung cancer, especially in the final stages. They aim to comfort patients and their families, making this tough time a bit easier. These services help manage pain, tiredness, and emotional distress, common in advanced lung cancer.
How Palliative Care Works
Palliative care helps ease suffering at all illness stages, complementing other treatments. It’s given by a team, including doctors, nurses, and social workers. They work with the patient’s healthcare team. They focus on:
- Managing pain, nausea, and side effects
- Providing emotional support and counseling
- Helping with future planning and treatment goals
- Offering nutritional advice and support
This care can begin with a lung cancer diagnosis. Starting early helps with symptom relief and overall health. Resources from organizations like the American Lung Association are helpful. Visit this link for more information.
When to Use Hospice Care
Hospice care focuses on comfort in the last months of life, not on curing. It’s for when patients have six months or less to live, as Medicare states. This care aims to ease physical and emotional pain, helping patients find peace. It includes:
- Support for families and caregivers
- 24/7 access to healthcare pros
- Coordinating care at home, in hospitals, or hospice facilities
Knowing when to switch to hospice care is important for families to provide comfort and support. Discussing with healthcare providers is crucial to understand these options in the complex journey of end-of-life care.
Importance of Pain Management
Pain management is key for patients with lung cancer. It improves life quality by easing pain. This allows people to stay comfortable and dignified, even in late stages. There are various ways to manage pain, like opioids and other medicines.
It’s crucial to understand pain’s complex nature. Pain from lung cancer can come from the disease, treatment, or psychological factors. An effective pain plan helps patients and their families feel better overall.
Working together in healthcare is important. Teamwork, especially with palliative care experts, can provide customized care. It’s important to look at all pain relief options. Studies show starting palliative care early helps manage symptoms and lowers emotional stress from cancer pain.
| Type of Pain Management | Description | Example Treatments |
|---|---|---|
| Pharmacological Interventions | Use of medications to alleviate pain. | Opioids, NSAIDs, adjuvant analgesics |
| Non-Pharmacological Interventions | Techniques to manage pain without medications. | Physical therapy, acupuncture, meditation |
| Palliative Care | Comprehensive care aimed at improving quality of life. | Counseling, symptom management, holistic approaches |
| Hospice Care | Care provided during the end stages of life. | Comfort measures, emotional support, pain relief |
Knowing these pain management methods is vital for handling lung cancer pain. Caregivers must pay attention to both physical and emotional pain. Honest discussions can improve coping and healthcare results. For more information on managing lung cancer pain, visit this resource.
Emotional and Psychological Considerations
The journey for lung cancer patients and their caregivers is tough. It can change their life’s quality. Those with lung cancer often feel more upset, adding to their symptoms. Studies show 43.4% of them face emotional distress. This is higher than the cancer patient average of 35.1%. Knowing this, we must address lung cancer’s psychological impact. It’s key for providing the right emotional support.
Support for Caregivers
Caregivers are crucial for lung cancer patients. They face a lot of stress, both emotionally and physically. Supporting caregivers properly is essential. It helps them handle their duties and the stress that comes with them. By understanding caregivers’ needs, we can offer specific support. This ensures they get the necessary help to stay well. Through counseling, support groups, and learning programs, caregivers can become stronger. This helps them care better for their loved ones.
Addressing Emotional Distress
Tackling the emotional pain of lung cancer needs several steps. It’s important to spot emotional issues when first diagnosed. This allows for early help, managing symptoms before they get worse. Good talks between doctors and patients are vital. They help everyone understand the mental challenges of lung cancer. This opens the door for better support. Letting patients share their feelings can boost their emotional health. This leads to better overall health results. For tips on symptom management, check out this resource.

End-of-Life Planning for Lung Cancer Patients
End-of-life planning is vital for lung cancer patients. It ensures their wishes are heard and their care choices are met. Talking about advance directives can lower stress for patients and their loved ones.
These legal papers, like a living will and power of attorney, help make big medical and financial choices at key times.
Studies show that lung cancer patients have mixed feelings about end-of-life planning. About 30%-40% have advance directives, but only 20% say doctors talk about these crucial topics. This makes the family’s role very important; around 70% of patients include their families in these talks.
This helps them clearly state their care choices.
Support groups are a big help, with 60% of lung cancer patients joining to deal with the tough feelings about end-of-life planning. Also, about 45% use professional support, like social workers or counselors. These pros offer advice during these hard times.
Patients have many options to think about. They can choose at-home hospice, assisted living, or inpatient hospice care. Those who pick at-home hospice need a full-time caregiver.
Talking openly with healthcare providers is key. It helps patients understand their situation better. This lets them make good choices about their treatment and care wants.
As they go through these tough discussions and choices, they might find help in writing in a journal, therapy, and spiritual support. These methods improve emotional health and help patients play a big part in their end-of-life planning.
| Aspect | Statistics |
|---|---|
| Advance Directives Usage | 30%-40% |
| Support Group Participation | 60% |
| Power of Attorney Assignment | 25% |
| Doctors Initiating Discussions | 20% |
| Family Involvement in Discussions | 70% |
| Use of Professional Support Services | 45% |
| Journaling Practice | 30% |
Conclusion
Understanding advanced lung cancer is vital for patients and their families. The path of cancer is complex and full of emotions. As one nears life’s end, physical changes like more sleep, swallowing issues, and different breathing occur.
These signs show key moments are near. They signal a shift in care goals and support methods.
Supporting families in these hard times is critical. Caregivers often feel confused and sad. Help is out there, from healthcare workers to counselors.
They discuss emotional, spiritual, and practical needs. This includes handling physical symptoms and legal end-of-life care matters.
Knowing these signs and the emotional journey helps families. It allows them to face the end with compassion and respect. This ensures patients and caregivers get the needed support in these tough times.