Lung cancer is the top cause of cancer deaths in the US, with over 150,000 lives lost each year. With such high numbers, finding effective treatments is urgent. The good news is, lung cancer treatment is improving. New pills are being developed that could change patients’ futures.
A big step forward is sotorasib, a drug recently approved by the FDA. It works well against a specific genetic change in the KRAS gene. This new therapy not only shrinks tumors but also helps people live longer.
As we learn more about lung cancer, it’s clear how important genetics and new treatments are. This article looks at the latest in lung cancer care. It shows how targeted treatments and gene tests are key to fighting lung cancer.
Key Takeaways
- Lung cancer is the leading cause of cancer-related deaths in the United States.
- Sotorasib, a newly approved drug, targets the KRAS gene mutation, enhancing patient survival.
- Latest treatment options are focused on targeted therapy and precision medicine.
- Research is pivotal in discovering effective lung cancer pills and therapies.
- Genomic testing plays a crucial role in identifying the best treatment strategies.
Introduction to Lung Cancer and Current Challenges
Lung cancer is the second most common cancer in the United States. It leads to many cancer deaths. In 2023, we expect around 238,340 new cases and 127,070 deaths. Understanding lung cancer statistics is key. It helps raise awareness and better treatment outcomes.
Even with early detection like low-dose CT scans, many find out too late. This makes treating lung cancer hard.
Lung adenocarcinoma (ADC) makes up about 40% of lung cancer cases. Patients face many challenges, especially with rare types like pulmonary sarcomatoid carcinoma (PSC). These patients often have a bad outlook and few treatment options. Gene mutation analysis helps find about 93.8% of mutations. This is crucial for personalized therapy.
Many people don’t know enough about lung cancer. This lack of awareness leads to high death rates in advanced stages. For non-small cell lung cancer (NSCLC), death rates are 45% to 76% within five years after surgery. More research and better treatment methods are needed.
There’s work on new treatments, but challenges remain. We are learning more about the genetic side and how to overcome resistance. This research gives hope. It aims to improve survival rates and life quality for lung cancer patients.
For instance, radiation therapy could improve current treatments. It might help deal with some issues in treating non-small cell lung cancer.
For more info on this research, check out current lung cancer research efforts.
Understanding Lung Cancer Types and Stages
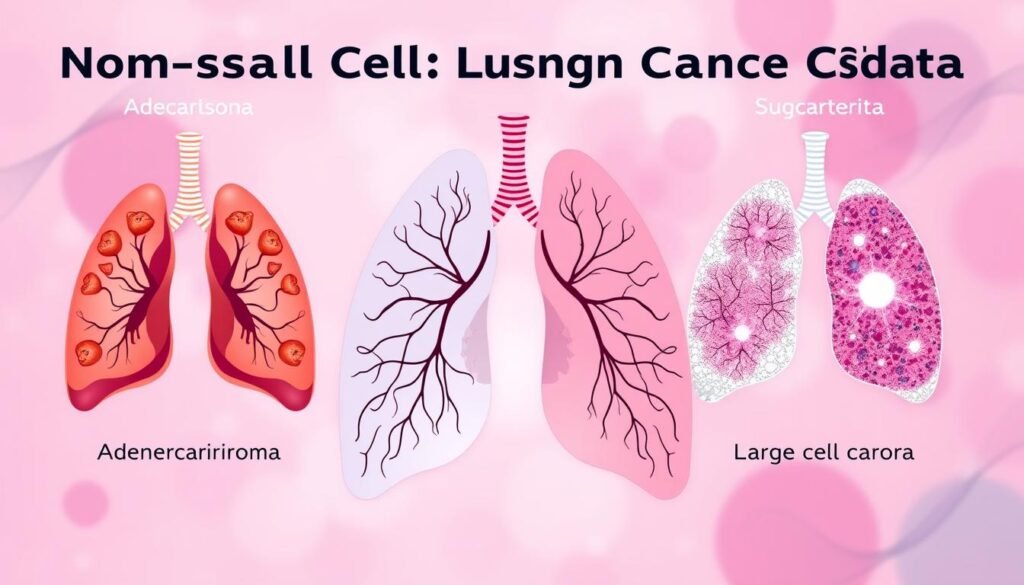
Lung cancer is mainly split into two types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC makes up about 80% to 85% of all lung cancer cases. Knowing these types and their lung cancer staging helps choose the right treatment.
There are different kinds of NSCLC, like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Each one grows differently. For example, adenocarcinoma is common in smokers and non-smokers alike. Squamous cell carcinoma, however, is more linked to smoking.
About 10% to 15% of lung cancers are SCLC. This cancer is aggressive and spreads fast. It’s very different from NSCLC, especially in how it’s treated and staged.
Staging lung cancer is crucial to understand how far the disease has progressed. Doctors often use the TNM system. It looks at the tumor size (T), lymph node involvement (N), and whether it has spread (M). This system helps plan the patient’s treatment.
| Staging Category | Description |
|---|---|
| Stage 0 | Carcinoma in situ; early-stage non-invasive cancer. |
| Stage I | Localized cancer; hasn’t spread outside the lungs. |
| Stage II | Beyond Stage I; may have reached nearby lymph nodes. |
| Stage III | Locally advanced cancer; potentially spread to nearby areas and lymph nodes. |
| Stage IV | Advanced cancer; has spread to distant organs like the liver or brain. |
Knowing a patient’s specific type and stage of lung cancer is key. It lets doctors create a personalized treatment plan. This could mean surgery for early stages or various therapies for more advanced ones. Understanding whether the lung cancer is small cell or non-small cell, along with its stage, is crucial for treatment choices and how well patients do.
What is a Lung Cancer Pill?
A lung cancer pill is a type of oral medication aimed at fighting lung cancer. It uses targeted therapy to zero in on specific genetic changes linked to the disease. This allows for treatments tailored to each patient’s unique situation. By blocking the cancer’s growth mechanisms, these pills can slow down the tumor’s spread effectively.
Definition and Overview
Lung cancer pills include a variety of oral medications that act as targeted therapies. A key example is osimertinib, which treats non-small cell lung cancer (NSCLC) patients with certain EGFR gene mutations. This form of targeted treatment has shown great promise in enhancing patient survival and well-being. According to the ADAURA trial, 88% of patients treated with osimertinib survived five years post-treatment in early-stage NSCLC, proving its effectiveness.
Mechanism of Action in Targeted Therapy
Targeted therapies like osimertinib work by interrupting the signals that cause cancer cells to grow. They attach to specific mutated proteins and stop them from functioning, which slows down tumor growth. For patients with early-stage NSCLC, testing for EGFR mutations is crucial to see if osimertinib is a suitable treatment. This approach is a cornerstone of personalized medicine in lung cancer care.

Latest Treatment Options for Lung Cancer
There have been great strides in lung cancer treatment. Targeted therapies and immunotherapy are pushing the limits of traditional methods. This leads to better outcomes for those battling lung cancer.
Targeted Therapy Innovations
Targeted therapies have seen significant advancement recently. One key discovery is sotorasib, aimed at treating the KRAS G12C mutation found in some lung cancer cases. Clinical trials showed sotorasib could shrink tumors in 82% of patients. Moreover, the latest lung cancer treatments like sotorasib not only reduce tumor sizes but also extend patient survival times, averaging 12.5 months in studies.
Beyond sotorasib, there are therapies like alectinib for ALK-positive lung cancer. These options cater to unique genetic mutations, offering improved outcomes over standard treatments.
Immunotherapy and Its Role
Immunotherapy is now essential in treating lung cancer, especially with checkpoint inhibitors like pembrolizumab. It boosts the immune system to fight cancer more effectively. Combining immunotherapy with certain chemotherapy agents has shown better success rates in trials, prompting further research into combined treatments.
Pembrolizumab treatment can cause side effects, from fatigue and rash to severe immune reactions. It’s key for patients and doctors to be aware of these risks. With the new drug approvals, lung cancer treatment is constantly evolving.

Precision Medicine and Personalized Treatment Approaches
Lung cancer is the top tumor type worldwide, making up 12.9% of all tumor cases each year. This fact stresses the need for new treatment options. Precision medicine offers hope by tailoring treatments to each person’s genetic makeup. By analyzing genomes, transcripts, proteins, and metabolites, doctors can create custom lung cancer treatments for everyone.
Non-small cell lung cancer (NSCLC) is especially complicated, with less than half of its driver genes known. This shows there’s much we still need to learn and explore in targeted therapies. Precision medicine has led to effective treatments, especially for specific gene mutations like EGFR-TK and EML4-ALK. Patients with these mutations have seen improved outcomes in advanced stages of lung cancer thanks to these precision treatments.
Immunotherapy has become a key player in treating lung cancer. It uses checkpoint inhibitors like CTLA4, PD-1, and PD-L1 to open new treatment avenues. PD-L1’s presence is a clue for how well immunotherapy might work, though results vary. Researching these markers is crucial for developing more effective treatments.
Liquid biopsies are a major step forward in precision medicine. This non-invasive test looks at tumor cells in the blood. It’s great for people who can’t have traditional biopsies. By combining this info with usual treatments like surgery and chemo, precision medicine aims to treat patients more effectively and personally.
Genomic Testing: A Key to Effective Treatment
Genomic testing is crucial in lung cancer care. It helps doctors find specific mutations to create the right treatment plans. This leads to better molecular profiling for patients, letting doctors craft more personalized therapies.
Importance of Molecular Profiling
Molecular profiling is key in cancer treatment. It spots genetic changes like EGFR, ALK, and KRAS mutations. These are vital for choosing the right targeted therapies. Now, over 500 genes can be tested, giving a full view of a tumor’s genetic make-up. This information makes it easier to pick treatments likely to work well for each patient.
Identifying Mutation-Specific Therapies
Mutation-specific treatments make a big difference. For example, 10-15% of NSCLC patients have EGFR mutations. They do well on EGFR tyrosine kinase inhibitors (TKIs), with response rates of 60-80%. This can extend the time without disease worsening by 9-12 months. ALK rearrangements, present in 3-7% of cases, also respond well to targeted treatments.
Thanks to new techniques like liquid biopsies and next-generation sequencing, doctors can quickly pinpoint mutations driving cancer. These advances improve treatment options and increase chances for patients to join clinical trials for mutation-specific therapies. This approach greatly advances personalized medicine for lung cancer patients.
| Mutation Type | Prevalence in NSCLC | Recommended Therapy |
|---|---|---|
| EGFR | 10-15% | EGFR TKIs |
| ALK | 3-7% | ALK inhibitors |
| KRAS | 20% | Targeted therapies under investigation |
| BRAF | 2-4% | BRAF inhibitors |
| HER2 | 2% | HER2-targeted therapies |
Exploring Specific Drugs: EGFR and ALK Inhibitors
Lung cancer drugs have made big advances recently. Targeted therapies now focus on attacking specific mutations in non-small cell lung cancer (NSCLC). EGFR and ALK inhibitors have changed the game in treatment, showing the big leaps in drug development.
EGFR Inhibitors: Current Developments
EGFR inhibitors are now key for treating NSCLC patients with EGFR mutations. Drugs like osimertinib are making a big difference. They delay the cancer from getting worse and help patients live longer. Yet, many patients eventually become resistant to these drugs. Research is ongoing for new medicines that target both new and resistant mutations.
Studies prove EGFR mutations respond well to drugs such as afatinib and dacomitinib. These have shown to be more effective in fighting cancer in patients.
ALK Inhibitors: Advances and Clinical Trials
ALK inhibitors are also making strides in lung cancer treatment. They are especially good for people with ALK gene changes, like those who are light or non-smokers with a certain type of NSCLC. Drugs such as lorlatinib and alectinib are proving to be very effective. Their development has led to many clinical trials. These trials test their effectiveness and probe new drug combinations.
For example, recent tests combining ALK inhibitors with EGFR TKIs are giving promising results. They seem to work better together, improving the outcomes for patients.
Research into targeted therapy is ongoing. It’s leading to new treatments that might change how we fight lung cancer in the future.
Emerging Research and Future Directions
The way we treat lung cancer is quickly changing, thanks to new research. Scientists are focusing on lung cancer research to find better treatments. Clinical trials are key to testing new therapies. They are working on lung cancer pills that could make a big difference for patients.
Clinical Trials Overview
Recent studies have shown exciting progress in understanding lung cancer better. David Rimm’s team made a breakthrough test for HER2 more sensitive. Now, over 60% of lung cancer patients might benefit from T-DXd. Before, only 2% could.
About 700 drugs are being tested in clinical trials right now, including T-DXd. These trials are moving us towards treatments that fit each person’s unique genetic makeup. This means better results and longer survival for people with non-small cell lung cancer (NSCLC).
Potential for New Lung Cancer Pills
In the future, we might have many new drugs for lung cancer, like AM-101. This drug works well in NSCLC and makes radiation more effective. Funding for this research is coming from trusted sources, showing a team effort in this fight.
These discoveries are very important. Soon, checking different biomarker levels might be a regular thing in cancer care. The outlook is hopeful for lung cancer patients, thanks to better tests and new treatments from ongoing trials.
For the latest on lung cancer treatments, check out recent studies and clinical findings.
Conclusion
The field of lung cancer treatment is changing fast. New treatments like lung cancer pills are making a big difference. These treatments are tailored to each person’s genetic makeup, improving care.
Durvalumab is one example. It helps patients live longer. However, it’s costly. This brings up questions about who can get these important treatments.
Research is ongoing, showing hope for future therapies. As studies continue, we look forward to cheaper and better treatments. This will help more people. Lung cancer pills are more than just medicine. They are a move towards care that meets individual needs.
To wrap things up, there’s a lot of work still to be done in lung cancer treatments. But, the progress we’re seeing is a big leap forward. Working together, researchers, doctors, and patients can create a brighter future for lung cancer care.